Abstract
Fingertip amputation is a challenging injury to manage. Among various reconstructive procedures, replantation results in superior outcome, but is seldom considered in many institutions. From the identification of vessel ends to reanastomosis of the submillimeter vessels, fingertip's highly specialized anatomy requires technical excellence. By addressing these anatomic challenges, fingertip replantation can be a routine reconstructive option for microvascular surgeons.
Keywords: fingertip amputation, replantation
Fintertip amputation distal to the extensor and flexor tendon insertion site on the distal phalanx (Zone I) was traditionally considered to be a nonreplantable amputation (Fig. 1).1 However, since the first report by Yamano et al,2 many hand centers have adopted routine replantation of fingertip as a valid reconstructive option fingertip. The early adopters have shown that successful fingertip replantation is superior, in form and function, to any other forms of fingertip reconstruction.3 The small-size artery as well as lack of a dorsal vein makes fingertip a demanding replantation. Mainly, there are three main challenges to fingertip replantation:
Fig. 1.
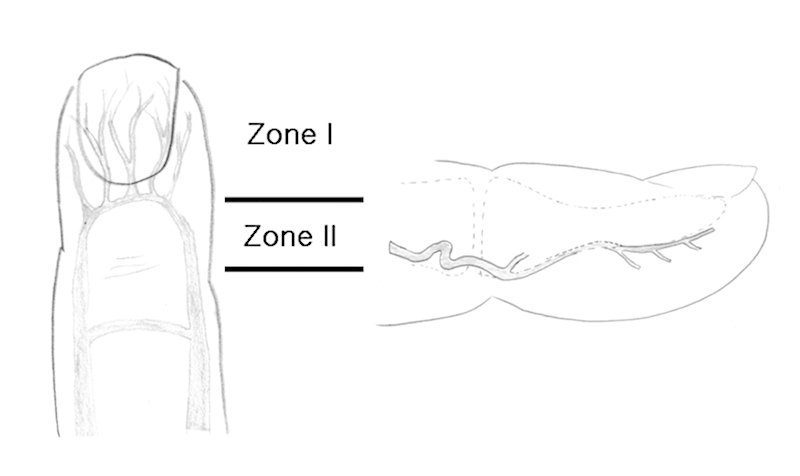
(Left) Classification of a fingertip injury. The terminal branches from the arcade correspond to zone I vessels. Zone II is proximal from zone I to the distal interphalangeal joint. (Right) The course of a digital artery is tortuous and adjacent to the periosteum of the distal phalangeal bone.
Identification of blood vessels
Anastomosis of small size vessel
Management of venous congestion
Understanding the anatomy is the initial step of forming fingertip replantation strategy.
Anatomy of the Fingertip
An intimate understanding of fingertip anatomy forms the basis of evaluation and treatment of fingertip amputation. The fingertip pulp is a predominant and unique feature of the fingertip. The fibrous septa that anchors the overlying skin to the periosteum of distal phalanx gives rise to the pulp and overlying skin a soft yet cohesive structure.4 The blood vessels of the fingertip forms an intimate anatomic relationship to the fibrous septa. Unlike at the proximal and middle phalanx, the neurovascular bundle is not surrounded by the Grayson ligament and the Cleland ligament at the distal phalanx. Instead, the terminal arteries and nerve branches are embedded in the pulp tissue and course between the fibrous septa, which run perpendicular to the dermis. The veins in the fingertip also run in the subcutaneous tissue of either the volar pulp or the paronychium.
Artery
The two palmar digital arteries usually collateralize at the midline—forming the pulp arcade at the level of lunula. The collateral arcade gives off several terminal branches that run parallel to the axis of the phalanx. These terminal branches (with diameters ranging from 0.3–0.7 mm) lie in a deep plane adjacent to the periosteum and anastomose with a branch of the dorsal network (Figs. 1, 2).5 During replantation, the redundant arterial course of this arcade is exploited to provide sufficient length needed for tension-free repair.
Fig. 2.
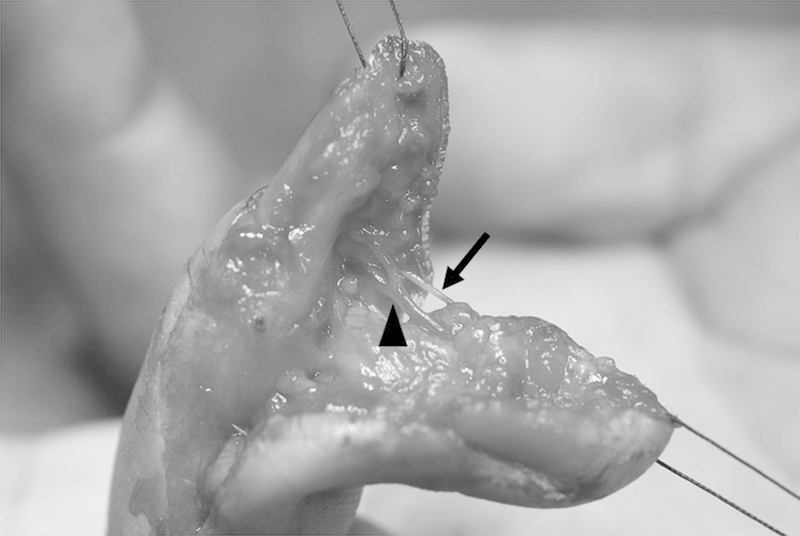
Digital artery (arrowhead). Digital nerve (arrow).
Vein
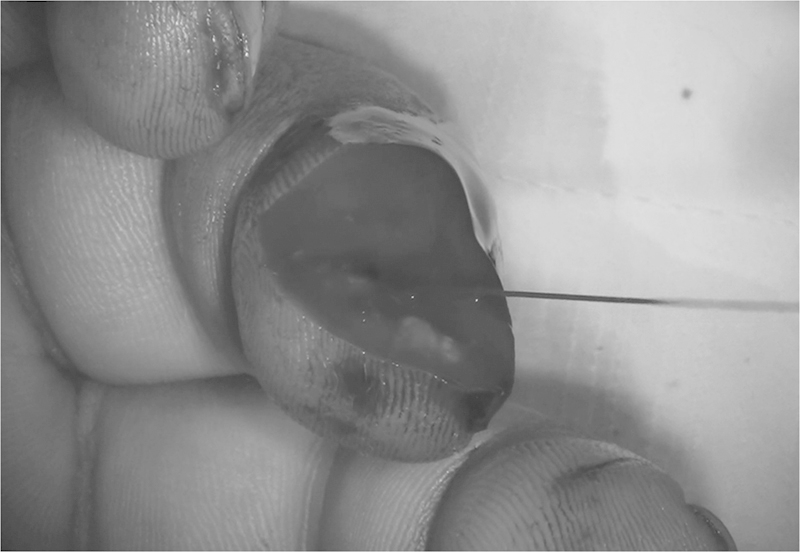
At the fingertip level, the veins are found in both volar and dorsal locations. The volar veins reside in the subcutaneous tissue just beneath the dermal layer where it takes a tortuous course through the fibrous septa. The terminal dorsal veins begin coalescing superficially at the distal paronychium and follow a proximal path in this plane. Next to the paronychium, the dorsal veins adhere tightly to the dermis, and its dissection is tedious. These veins fuse together at midline at around the level of distal interphalangeal (DIP) joint and drain into larger dorsal veins (Fig. 3).
Fig. 3.

The terminal dorsal veins arise from both sides of the paronychium. These veins fuse together and drain into larger dorsal veins.
Clinical Management
From initial presentation to postoperative management, the principle of fingertip replantation is in establishing and maintaining congestion-free revascularization of the amputated fingertip.
Emergency Room
History, specifically mechanism of injury, is usually an important aspect of initial assessment of fingertip amputation. Gross evaluation of the amputated fingertip is inadequate in assessing microvascular structures, but can reveal obvious soft tissue defects that would involve neurovascular bundles. It is important to match the amputated fingertip to the proximal finger stump. A gap created by a large soft tissue defect would render replantation impossible at this point and an alternative management should be sought. Finger x-ray is useful in determining amputation level and bony defect, if present. After a brief assessment, the proximal amputation site is dressed with lidocaine-soaked gauze to decrease pain. The amputated fingertip is wrapped with saline-soaked gauze for prevention of desiccation. An informed consent should include potential need for transfusion, alternative treatment options, as well as expected postoperative course and known complications.
Intraoperative Preparation
Brachial-plexus block is the preferred choice of anesthesia in replantation surgery. In children, general anesthesia is required, but a concomitant regional nerve block reduces pain and the risk of vasospasm in the perioperative period. A pneumatic tourniquet is applied to the arm after anesthesia is achieved. General anesthesia-induced hypotension can masquerade as a vasospasm or technical failure in anastomosis when the tourniquet is turned down; when the tourniquet is turned down to evaluate perfusion, it is important to ensure there is adequate systemic pressure. A finger tourniquet is an alternative in cases where local anesthesia is administered.
Microscopic Examination
Under magnification, the wound is evaluated for large soft tissue defects not apparent at initial presentation. Significant soft tissue defect prohibits replantation; an alternative management is sought. Foregoing such defect, focus is shifted to identification of the blood vessels.
First, tourniquet is turned down for pulsatile artery or bleeding in the proximal wound bed (Fig. 4). A lack of healthy blood flow to the wound bed implies problems of the artery at a proximal site, and its cause should be sought. Once proximal arterial flow is established, the amputated fingertip is examined for the terminal arteries previously mentioned. Spots of coagulated blood hint at the presence of blood vessels. If such clots are not present or is washed away in preparation, it is often possible to induce outflow by squeezing the amputated tissue. The proximal stump can provide an approximate mirror-image location of the artery. If these “clues” are unavailable, wound exploration should be focused on the plane adjacent to the periosteum, where the terminal arteries reside. After identification of the artery, both arteries are marked with 10–0 nylon suture on the vessel itself (Fig. 5).
Fig. 4.
The proximal artery can be identified with pulsation before applying a tourniquet.
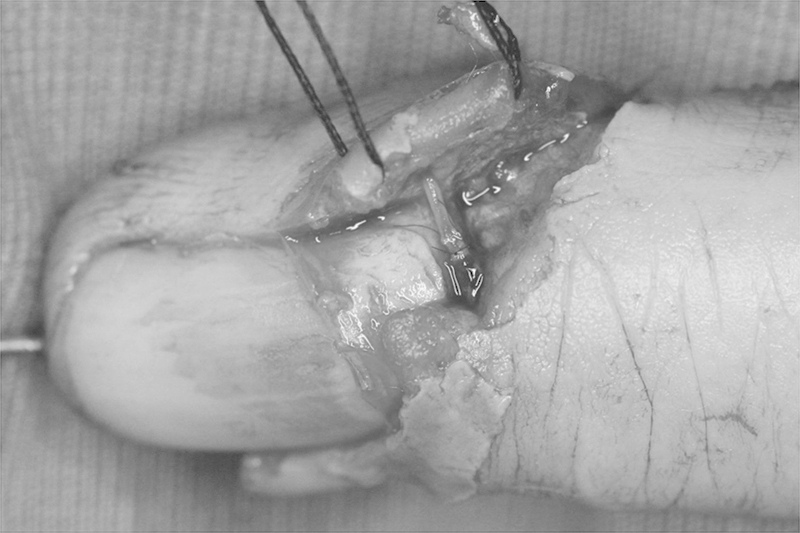
Fig. 5.
The artery on the amputated part was identified just above the periosteum and marked with 10–0 nylon for easy detection after fixation.
Next, the veins on the proximal digit stump are examined. The veins are identified also by the presence of blood clots or by the compression of the finger with retrograde venous flow toward the wound bed. When all veins are identified, their location is marked with either gentian violet in the pulp tissue or by a 10–0 nylon suture on the vessel itself. If these “clues” are unavailable, wound exploration should be focused on the plane just deep to the dermis where the subcutaneous veins reside. The proximal stump can provide an approximate mirror-image location of the subcutaneous vein as well.
Fixation of the Amputated Fingertip
If a significant arterial gap was present during the microscopic exam, the proximal bone should be shortened prior to fixation to avoid the interposition vein graft of the artery. A 0.9-mm K-wire is first inserted from the amputated fingertip from the amputation margin through the end of the fingertip. The fingertip is reapproximated to the finger with proper reduction of distal phalanx. The proximal end of K-wire is driven into the proximal segment while maintaining accurate reduction. Rigid fixation of the distal phalanx is often possible with a single axial K-wire (Figs. 6, 7). However, two parallel K-wires may be required for additional stability. Fixations involving the DIP joint is to be avoided to allow for early mobilization. If the DIP joint is fixated along with the distal phalanx, the K-wire through the joint should be withdrawn—freeing the DIP joint—before postoperative week 3.
Fig. 6.

Preoperative x-ray finding showed complete fingertip amputation of the ring finger and small finger.
Fig. 7.

K-wire fixation of the ring finger noted on postoperative x-ray.
With the skeletal axis stabilized, 6–0 chromic or nylon sutures are placed on both sides of the nailbed. In addition to approximating the nailbed, these sutures counterbalance the traction forces of stay sutures and prevent gross movement of amputated tip along the K-wire. After the nailbed is secured, the hand is stabilized in supination, and a wire holder is used to hold down the K-wire and the finger in extension. Avoiding injury to the subcutaneous veins, the proximal and distal amputation margins are retracted with traction sutures (Fig. 8).
Fig. 8.

Traction sutures were applied at both margins of the amputation for exposure of the vessels. These traction sutures make the arteries more superficial.
Arterial Anastomosis
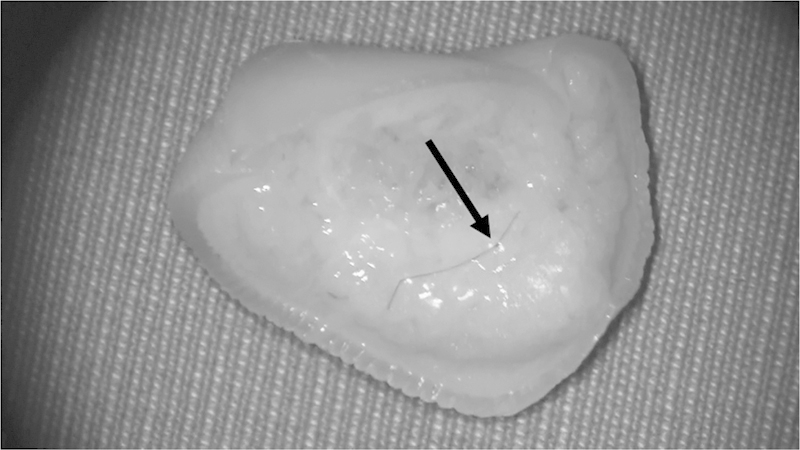
When volar skin on the distal margin of the wound is retracted with stay sutures, the pulp tissue becomes elevated. This brings the terminal branches of the pulp arcade to a more superficial and accessible location. Usually, there are two to three terminal arteries—all former branches of the pulp arcade. Selection of the anastomotic artery among these is dependent on the diameter, condition of the artery, and the location (Fig. 9).
Fig. 9.
The terminal branch was identified for anastomosis at the proximal margin.
If it is not able to approximate the proximal and distal artery to be anastomosed, these tortuous arteries can be straightened by dividing side branches, creating the most tension.6 The same maneuver is possible on the artery attached to the amputated finger (Fig. 10). Once the vessels have enough length for tension-free anastomosis, the digital arteries are anastomosed with simple, interrupted 10–0 nylon suture (Fig. 11). A 11–0 suture may be required for pediatric fingertip replantation. When the large arterial gap is present after debridement of crushed vascular ends proximally and distally, vein grafts are used (Fig. 12)7 instead of bone shortening or arthrodesis.
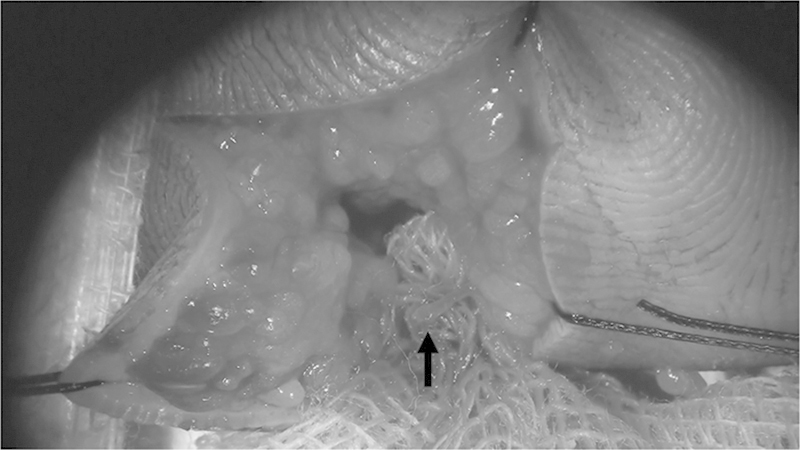
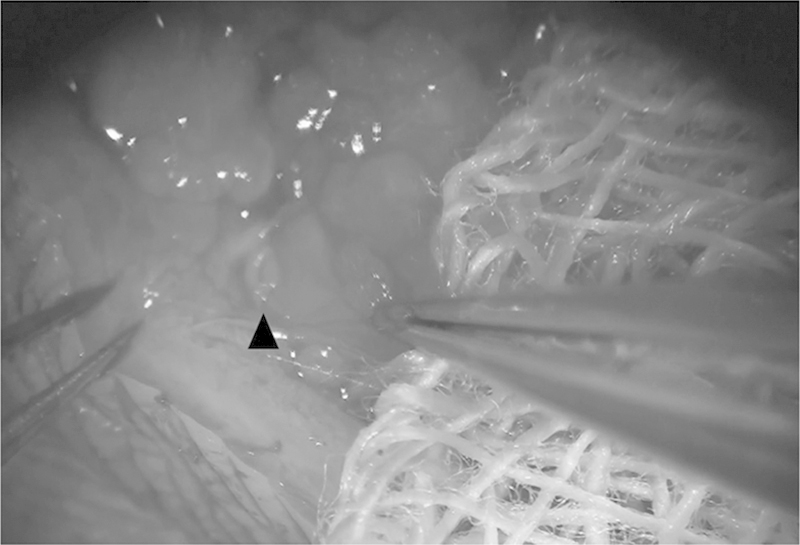
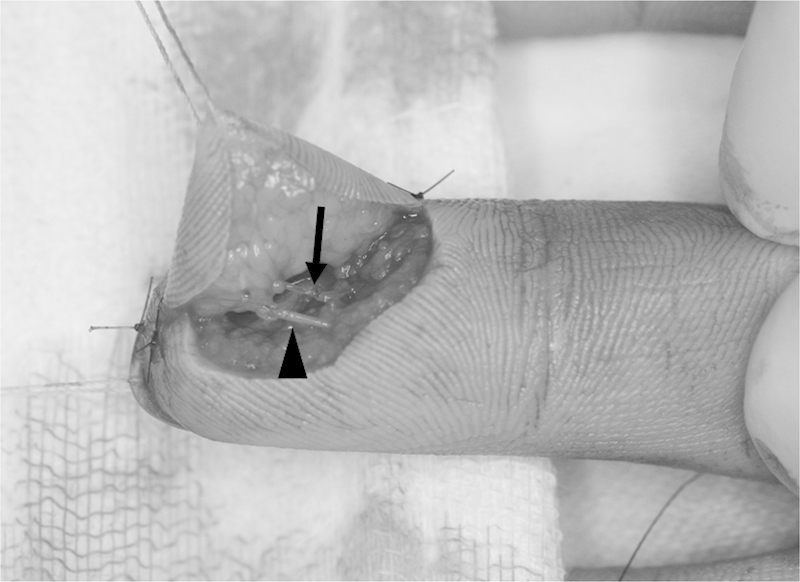
Fig. 10.
The terminal branch at the amputated part was pulled out gently with fine forceps (arrow). The side branch limiting elongation of artery was noted with the most tension (arrowhead).
Fig. 11.
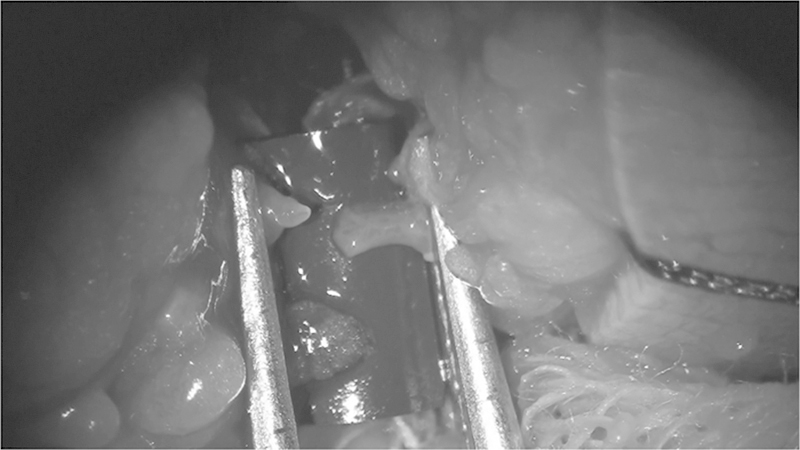
The arteries to be anastomosed are approximated with a vessel clamp.
Fig. 12.
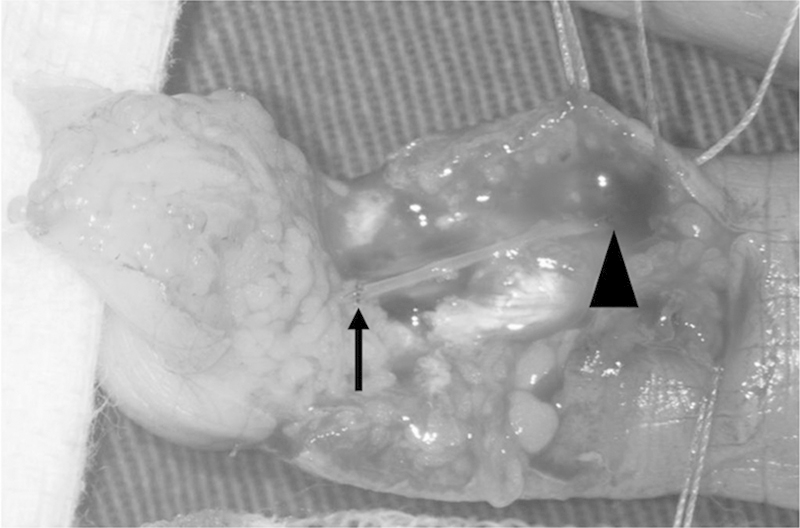
A vein graft harvested from the volar wrist was inserted to the arterial defect from arrowhead to arrow.
Neurorraphy
In the fingertip, the diameter digital nerve is diminutive. Even without neurorraphy, excellent sensory recovery has been reported.8 However, when a nerve is easily found, repaired whenever possible by the epineural repair method using 9–0 or 10–0 nylon suture after debridement; usually two to four sutures are used for nerve repair.
Venous Anastomosis
The technically demanding step in fingertip replantation is venous repair. Unlike proximal digital replantations, dorsal veins are not easily available in fingertip amputation cases because the dorsal area is occupied by nailbed. In fingertip amputation cases, however, volar subcutaneous veins or veins on either side of the nailbed (paronychium) are available for vein repair.
Identification of Volar Veins on the Proximal Part
Volar subcutaneous veins are located just beneath the dermis (Fig. 13). Exploration of veins should be focused on this area under the operating microscope. Exploration of a proximal vein is easier than a vein on the amputation part because engorged veins filled with blood at a proximal part are easily noted (Fig. 14). If engorged veins are not identified, a milking maneuver compressing the digit from proximal to distal can be performed to induce venous engorgement or bleeding from vein.
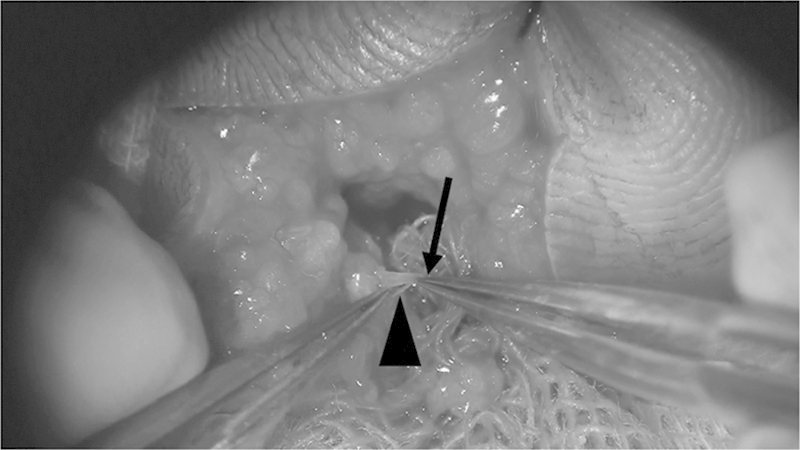
Fig. 13.
A volar vein was noted just underneath the dermis (arrowhead).
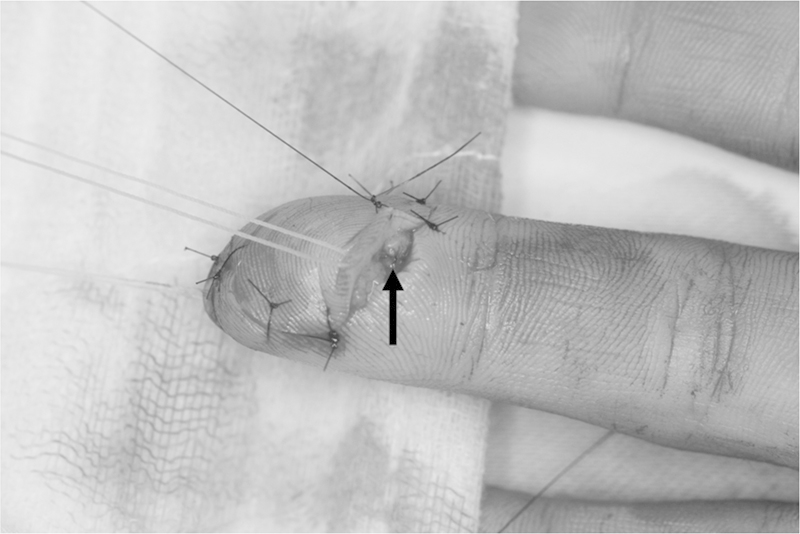
Fig. 14.
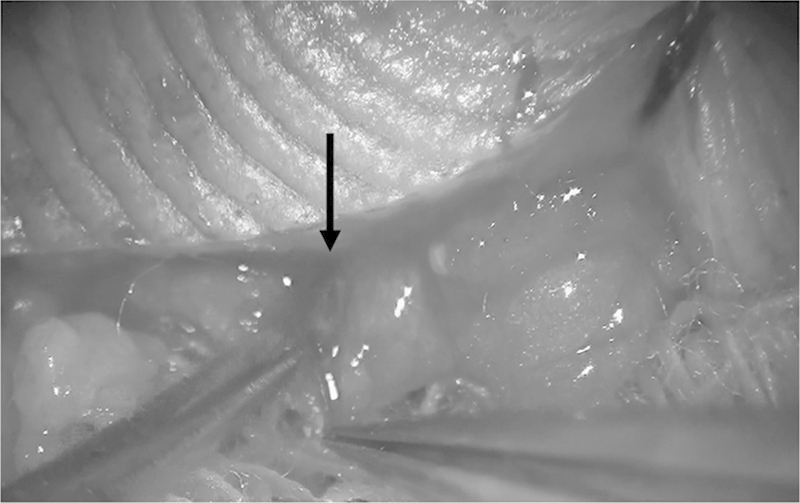
A blood-filled volar vein was identified easily at the proximal part (arrow).
Identification of Volar Veins on the Amputation Part
After a proximal vein is found, veins at the amputation part are explored with the help of mirror image. Because volar veins pass through the fibrous septa of pulp, exposure and mobilization of volar veins are limited by these structures. For venous anastomosis, 2 to 3 mm is the minimum length on both sides. Dissection is performed to mobilize vein. By cutting fibrous septa, the course of the vein gets straighter and the gain of length would be achieved. Because fibrous septa of pulp are very fine and sometimes these are not distinct, meticulous vein dissection should be done under the microscope to prevent damage. To identify fibrous septa, gentle traction of the vein is helpful after holding the vein with fine-tip microforceps (Fig. 15). Because the course of veins is angulated by dense fibrous septa, fibrous septa can be found where vein is angulated. Once cutting each fibrous septa, the vein can be mobilized. Isolation of the vein in between the fibrous septa should be performed until enough length of vein is achieved for anastomosis.
Fig. 15.
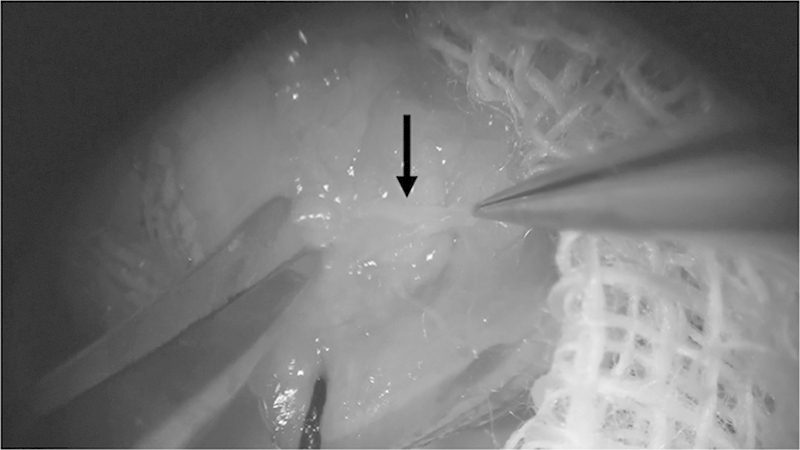
The volar vein in between fibrous septa was pulled out by microforceps (arrow). When fibrous septa are prominent with this maneuver, they can be cut with a micro-Metzenbaum easily.
Volar Vein Repair
Then, skin is sutured at a few millimeters apart from the anastomosis site to reduce the tension of vein anastomosis. If the ends of veins hiding behind skin edges are not visible under microscope, a stay suture with fine suture material is used for exposure of the venous anastomosis site. After adequate exposure of the vein without tension, vein anastomosis can be performed under an operating microscope (Fig. 16).
Fig. 16.
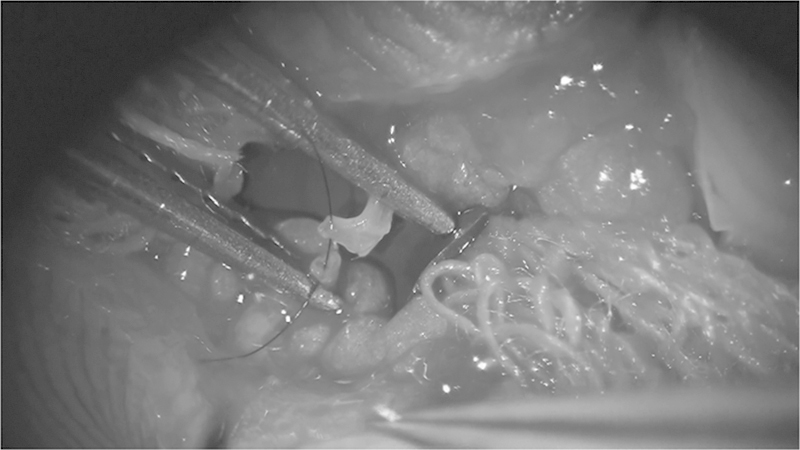
After approximation of the proximal and distal volar veins, the first passing of 10–0 nylon was made through them.
Dorsal Vein Repair
Another option of vein repair is to use the dorsal veins at both sides of nailbed. These veins are converged to center on dorsum of finger. However, dense fibrous tissue on paronychium makes skin mobility limited, vein dissection is not easy. A proximal vein is identified first with same method of volar vein. Then, a distal vein is exposed. When isolation of a distal vein on paronychium is difficult, a skin incision could be made along the nailbed and perionychium fold following the skin retraction with a stay suture (Figs. 17, 18). Usually, a vein could be found just beneath the skin parallel to the lateral margin of the nail bed. Meticulous dissection should be performed just beneath the paronychial skin under the operating microscope.
Fig. 17.
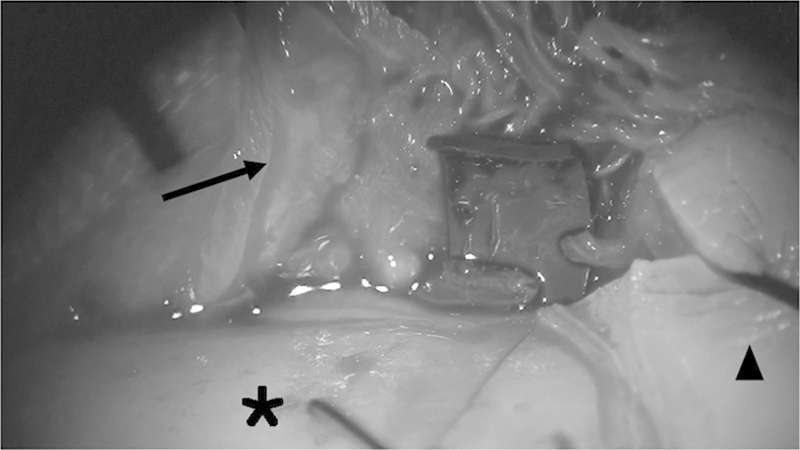
The paronychium (arrow) was retracted by a traction suture after a skin incision parallel to the margin of the nailbed (asterisk). Arrowhead points to the retracted eponychium. The isolated dorsal veins were noted on blue background.
Fig. 18.
The repaired dorsal veins.
Other Options for Prevention of Venous Congestion
If no vein is found on the amputated part, a collateral artery in the amputated part identified by returning blood flow from arterial anastomosis can be repaired to a vein on the proximal wound bed. If a vein is not available immediate after artery repair, delayed venous repair is another option.9 Developing venous congestion after replantation surgery, dilated subdermal veins are easily able to be detected on re-exploration. These dilated veins are usually enlarged and are easily anastomosed.
Skin Closure
The volar skin is approximated with minimal number of fine stitches. Tension is avoided to prevent venous compression and spontaneous evacuation of hematoma. Care should be taken to avoid injuring the superficial venous anastomosis or its tributaries.
Postoperative Management
Systemic heparinization is initiated in the operating room with 2000 IU every 4 hours, and continued for 2 weeks postoperatively. PGE1 is given for 7 days.
Monitoring
Careful monitoring of circulation is required during the first few days. Arteries and veins in the fingertip are susceptible to thrombosis or spasm due to its smaller size. Postoperative edema is common because blood flow is not distributed evenly across the fibrous septa in pulp tissue. Eventually, venous congestion is frequently developed even after vein repair. Transient venous congestion immediately after replantation by edema should be treated by temporary external bleeding for a specified time. Otherwise, venous collapse and continued edema result in irreversible tissue damage of the replanted part.
External Bleeding
If the vein is not repaired, external bleeding starts immediately after the operation and continues until neovascularization. Many methods can be adopted for external bleeding followed: a fish-mouth incision, dermal deepthelization (Fig. 19), nailhole, and periodic puncture of the fingertip, manual squeezing, local subcutaneous heparin treatment, dripping of heparinized saline (Fig. 20), or use of medical leeches (Fig. 21). During an external bleeding procedure, continuous bleeding is important to prevent venous congestion that can cause irreversible tissue damage more rapidly than ischemia.10 Authors prefer the use of a medical leech immediate after surgery. Because a leech finds best bleeding spot and makes spontaneous external bleeding for several hours. External bleeding and closed monitoring is crucial for the first postoperative night. Dermal de-epithelization is the preferred method to a fish mouth incision or nailhole. If the amputation stump is too small, a fish mouth incision will deepen and can injure the vascular system. Method of dermal de-eptheliztion is removal of only a small piece of skin from the replanted part like as harvest of split thickness skin graft. Many dermal perforators on the de-epithelized area are exposed. Maintenance of external bleeding can be achieved by gentle scrubbing with gauze or a 30-gauge needle. Topical dripping of heparin-mixed saline (25,000 IU heparin in 1 L of saline) is used for the prevention of a blood clot formation.
Fig. 19.

(Left) Deepithelization was made by No. 15 blade. (Right) Fresh bleeding came out from the dermal capillaries.
Fig. 20.
Continuous dripping of saline mixed with heparin prevents the formation of a blood clot.
Fig. 21.

A medical leech was used for the drainage of congested blood.
Evaluation and Maintenance of External Bleeding
Dark-colored external bleeding means venous congestion or permanent damage of the amputation part. If the color of bleeding is getting fresh color after drainage of congested blood, this means more vigorous external bleeding is required to maintain the balance between arterial inflows and venous drainage. But, if not fresh, this implies irreversible damage of the amputation part or the local trauma of external bleeding site.
Fresh bleeding after the pinprick with a 23-gauge needle on the amputation part means the time changing the bleeding spot with local trauma. After using one de-epthelized area for a few days, local trauma on the external bleeding site can be developed, which cause partial necrosis or significant atrophy. External bleeding site should be changed usually every 2 days before development of permanent damage.
External bleeding is continued until neovascularization is achieved. The average period of the neovascularization in a fingertip replantation without a vein is 7.6 days.11 Proper neovascularization can be evaluated by stopping external bleeding on the fifth day after surgery. If there is no venous congestion, external bleeding is not required any more. But if there is congestion, external bleeding should be continued and re-evaluate everyday.
Early Mobilization
Once neovascularization is finished, gentle motion of the hand is recommended with a splint. At 2 weeks after the operation, the splint is removed during the daytime for physical therapy. A splint is applied during the night for 2 more weeks. If a K-wire is fixed across a DIP joint, a K-wire is extracted from DIP joint at 3 weeks after operation and joint exercise should be started. The K-wire is totally removed at 4 to 6 weeks after the operation.
Conclusion
Challenges in fingertip replantation are technical in nature: identifying vessels, anastomosis of submillimeter vessels, and prevention/management of venous congestion. Identification of the vessels is made possible from a fundamental anatomical understanding of the fingertip. Vascular anastomosis of the so-called supermicrosurgery scale is discussed extensively in literature and has been challenged in major hand centers worldwide. The primary prevention of venous congestion is necessary for a successful replantation. If venous anastomosis is not possible, postoperative options are sought until neovascularization occurs. Even though fingertip replantation demands much in the way of concentration, microsurgical skills, and equally skilled support staffs, it is superior end-result (Figs. 22 23 24 25 26 27 28) should be the foremost guiding principle in choosing replantation as the reconstruction of choice.
Fig. 22.
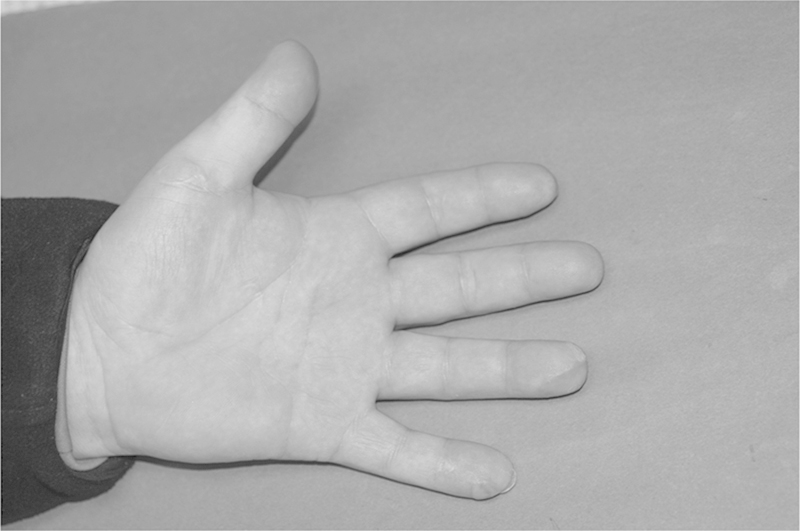
Postoperative results.
Fig. 23.

A case of complete amputation of the fingertip of the long finger, right hand.
Fig. 24.
The repaired arteries (arrow). The repaired nerves (arrowhead).
Fig. 25.
The repaired volar veins were filled with blood after removal of a vessel clamp.
Fig. 26.
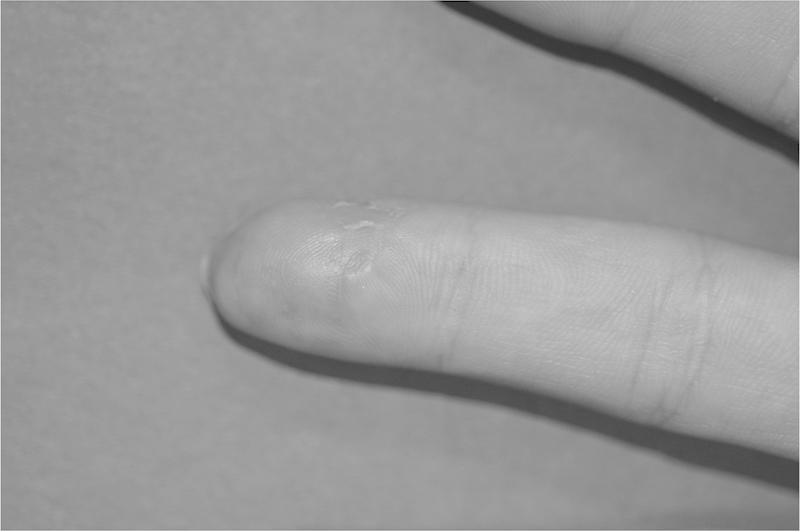
Postoperative results.
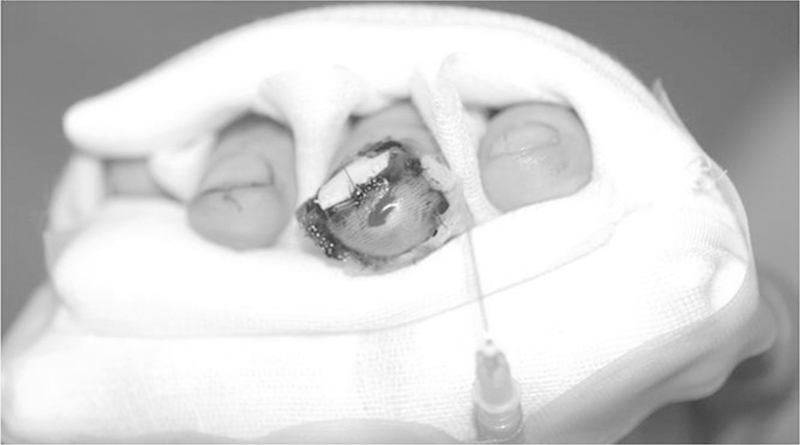
Fig. 27.

A 4-year-old child had fingertip injuries of the index and long fingers, right hand.
Fig. 28.
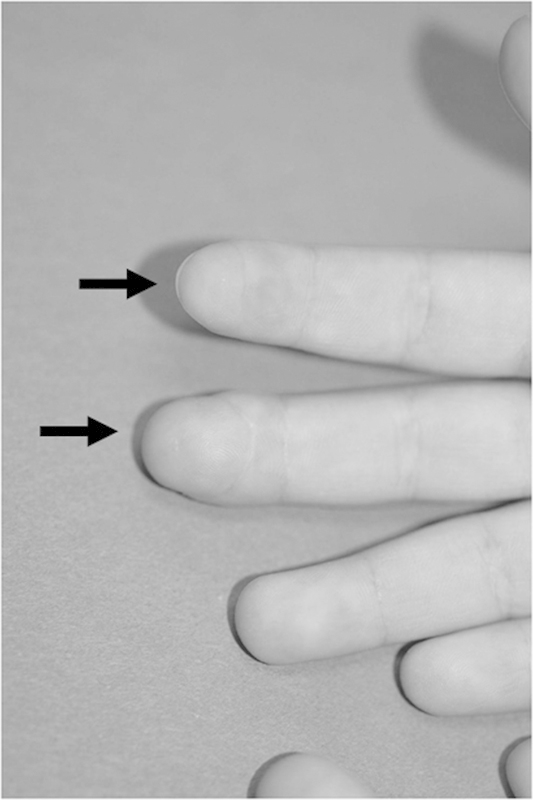
Postoperative results.
Acknowledgments
The authors deeply appreciate Aram Harijan Kim, MD, University of California, San Francisco East Bay, PGY 1, for his advice on this paper.
References
- 1.Tamai S. Twenty years' experience of limb replantation—review of 293 upper extremity replants. J Hand Surg Am. 1982;7(6):549–556. doi: 10.1016/s0363-5023(82)80100-7. [DOI] [PubMed] [Google Scholar]
- 2.Yamano Y. Replantation of the amputated distal part of the fingers. J Hand Surg Am. 1985;10(2):211–218. doi: 10.1016/s0363-5023(85)80107-6. [DOI] [PubMed] [Google Scholar]
- 3.Kim W K, Lim J H, Han S K. Fingertip replantations: clinical evaluation of 135 digits. Plast Reconstr Surg. 1996;98(3):470–476. doi: 10.1097/00006534-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Russell R C. Philadelphia, PA: WB Saunders; 1990. Fingertip injuries; pp. 4477–4478. [Google Scholar]
- 5.Strauch B, de Moura W. Arterial system of the fingers. J Hand Surg Am. 1990;15(1):148–154. doi: 10.1016/s0363-5023(09)91123-6. [DOI] [PubMed] [Google Scholar]
- 6.Dautel G, Barbary S. Mini replants: fingertip replant distal to the IP or DIP joint. J Plast Reconstr Aesthet Surg. 2007;60(7):811–815. doi: 10.1016/j.bjps.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 7.Yan H, Jackson W D, Songcharoen S. et al. Vein grafting in fingertip replantations. Microsurgery. 2009;29(4):275–281. doi: 10.1002/micr.20614. [DOI] [PubMed] [Google Scholar]
- 8.Ozcelik I B, Tuncer S, Purisa H. et al. Sensory outcome of fingertip replantations without nerve repair. Microsurgery. 2008;28(7):524–530. doi: 10.1002/micr.20543. [DOI] [PubMed] [Google Scholar]
- 9.Koshima I, Yamashita S, Sugiyama N, Ushio S, Tsutsui T, Nanba Y. Successful delayed venous drainage in 16 consecutive distal phalangeal replantations. Plast Reconstr Surg. 2005;115(1):149–154. [PubMed] [Google Scholar]
- 10.Hedén P Sollevi A Circulatory and metabolic events in pig island skin flaps after arterial or venous occlusion Plast Reconstr Surg 1989843475–481., discussion 482–483 [DOI] [PubMed] [Google Scholar]
- 11.Han S K, Chung H S, Kim W K. The timing of neovascularization in fingertip replantation by external bleeding. Plast Reconstr Surg. 2002;110(4):1042–1046. doi: 10.1097/01.PRS.0000021447.75209.0A. [DOI] [PubMed] [Google Scholar]


