Abstract
Purpose
The purpose of this study was to compare the biomechanical strength of the cephalomedullary nail InterTAN in cases of intertrochanteric fractures with the commonly used PFNA.
Methods
Sixteen fresh specimens of the proximal femur were used as intertrochanteric fracture models and were fixed using two fixation devices: the new proximal femoral nail (InterTAN) and proximal femoral nail antirotation (PFNA). An intertrochanteric fracture was created in composite bone models. Each specimen was loaded to simulate single leg stance while stiffness, migration (cut out), compressive force across the fracture site, and distal fragment rotation were monitored. The different internal fixation methods were tested by an experimental press analysis.
Results
Results of tests for femoral strength, stiffness, stability, and bearing capacity demonstrated that the biomechanical function of InterTAN was better than that of PFNA (P < 0.05). Compared with the PFNA nail, InterTAN showed increased strength, stiffness, and resistance torque of 30 %, 15 %, and 27 %, respectively.
Conclusion
Comparison of the treatment of intertrochanteric fractures with InterTAN and PFNA internal fixation showed that the InterTAN yielded improvement relative to the PFNA. InterTAN has a firmer and biomechanically superior performance and is therefore an ideal internal fixation method for treating intertrochanteric fractures. Additional research in osteopenic bone is necessary to comprehensively characterize the effects of the design enhancements of these two implants.
Keywords: Intertrochanteric fracture, InterTAN, PFNA, Biomechanical test, Fractured neck of femur, Hip fracture
Introduction
Intertrochanteric fracture resulting from osteoporosis or muscle weakness has become a common injury with the rapid increase in the number of elderly people [1, 2]. Intramedullary fixation is the primary surgical treatment for unstable intertrochanteric fracture, although there are limitations to this approach. Internal surgical fixations mainly include extramedullary fixation and placement of a proximal femoral nail (e.g., Gamma nail, proximal femoral nail—InterTAN, and proximal femoral nail antirotation—PFNA), along with a dynamic hip screw. Each surgical fixation has advantages and disadvantages, depending on the type of fracture. Intertrochanteric fractures occur between the neck fundus and lesser trochanter. PFNA was developed and put into clinical use to solve these problems especially for elderly patients. One of the important features of the device’s design was the use of a helical neck blade with a large surface area, which is important in osteoporotic bone, and provides rotational and angular stability [3]. InterTAN to treat trochanteric fractures was introduced and has had a good clinical outcome and a low number of complications. This implant uses two cephalocervical screws in an integrated mechanism, which allow linear intra-operative compression and rotational stability of the head or neck fragment. This device is being used more frequently in clinics, particularly to treat intertrochanteric fractures. InterTAN attempts to overcome the limitations, and the unique nail design clinically improves the recovery rate from intertrochanteric fractures, especially unstable intertrochanteric fractures [4].
To our knowledge, there has been no research on the mechanical performance comparison between InterTAN and PFNA of the intertrochanteric fractures. In the present study, biomechanical testing was used to systematically analyze and compare intertrochanteric fracture fixation samples, treated with a PFNA or InterTAN intramedullary nail, to provide a reliable scientific basis for choosing the better internal fixation method in clinical practice.
Materials and methods
All specimens were prepared in identical fashion.
Specimen Handling
We collected 16 fresh cadaveric femurs from 11 Chinese males and five Chinese females with an average age and weight of 64 years and 63.25 kg, respectively (Table 1). Before testing, the soft tissue was separated from the femoral head, and the bone mineral density (BMD; g/cm2) of each femur was tested with dual energy X-ray absorptiometry (model XR-36; Norland, USA) to examine the quality of the femurs and eliminate femurs with fractures. The femur was cut proximally to a length of 28 cm. The distal part of the femur was fixed with bone cement and was then preserved in an ice-box at -30 °C. The samples were randomly divided into two groups (Table 2) to fix the femoral intertrochanteric fractures: an InterTAN intramedullary nail or a PFNA intramedullary nail. Each group included a simulation of a Type I (stable) and IIA (unstable) fracture model according to the Evans-Jensen femoral intertrochanteric fracture type classifications. After the internal fixation was performed, similar to a clinical operation, each sample was examined with radiography to ensure that the position of the internal fixator was correct.
Table 1.
Characteristics of subjects from which the fresh cadaveric femurs were obtained
| Subject | Sex | Age (years) | Height (m) | Weight (kg) | Radiography findings | Freshness | BMD |
|---|---|---|---|---|---|---|---|
| 1 | M | 54 | 1.75 | 63 | Normal | Fresh | 0.804 |
| 2 | M | 75 | 1.68 | 70 | Normal | Fresh | 0.884 |
| 3 | M | 66 | 1.70 | 55 | Normal | Fresh | 0.593 |
| 4 | F | 58 | 1.64 | 52 | Normal | Fresh | 0.80 |
| 5 | M | 69 | 1.74 | 65 | Normal | Fresh | 0.432 |
| 6 | M | 70 | 1.68 | 60 | Normal | Fresh | 0.891 |
| 7 | F | 58 | 1.60 | 63 | Normal | Fresh | 0.473 |
| 8 | M | 62 | 1.62 | 64 | Normal | Fresh | 0.896 |
| 9 | M | 66 | 1.71 | 69 | Normal | Fresh | 0.811 |
| 10 | F | 62 | 1.58 | 61 | Normal | Fresh | 0.57 |
| 11 | F | 72 | 1.55 | 58 | Normal | Fresh | 0.603 |
| 12 | M | 68 | 1.72 | 69 | Normal | Fresh | 0.683 |
| 13 | M | 60 | 1.69 | 67 | Normal | Fresh | 0.763 |
| 14 | M | 56 | 1.74 | 66 | Normal | Fresh | 0.799 |
| 15 | F | 68 | 1.59 | 56 | Normal | Fresh | 0.51 |
| 16 | M | 60 | 1.72 | 74 | Normal | Fresh | 0.792 |
Table 2.
Model groups of specimens. Fixation InterTAN PFNA
| Evans-Jensen type | |
|---|---|
| I (stable type) 4 | IIa (unstable type) 4 |
| I (stable type) 4 | IIa (unstable type) 4 |
Experimental Mechanics Modeling
To evaluate the biomechanical properties and efficiency of the InterTAN and PFNA internal fixations, biomechanics experiments were performed, including axial compression, cutting of the femoral head and neck, anti-torsion strength, and load limit testing. To improve the precision of detection, all mechanical experimental specimens were prepared in accordance with the structure simulation, load, material property, fixation method, and height. Before the test, six high-precision and small-scale resistance strain gauges were arranged at a standard distance on the internal and external femurs of all samples. The femurs were fixed in a position to stimulate standing on one foot, with consideration for the abductor muscles participating in the work. The mechanical properties of the femur materials were measured before the experiment (Table 3). When performing the experiment, the femurs were pre-loaded three times with 100 N to eliminate the influence of time effects produced by femur relaxation, creep, and multiple measurements. To keep the femurs fresh, they were routinely soaked with saline.
Table 3.
Mechanical properties of the femur materials
| E (Mpa) | μ | ( ± S) ± S) |
σb (MPa) |
|---|---|---|---|
| Stretch | 72.92 | 10050 | 0.30 |
| Compression | 94.60 | 10180 | 0.30 |
| Curve | 106.42 | 9640 | 0.29 |
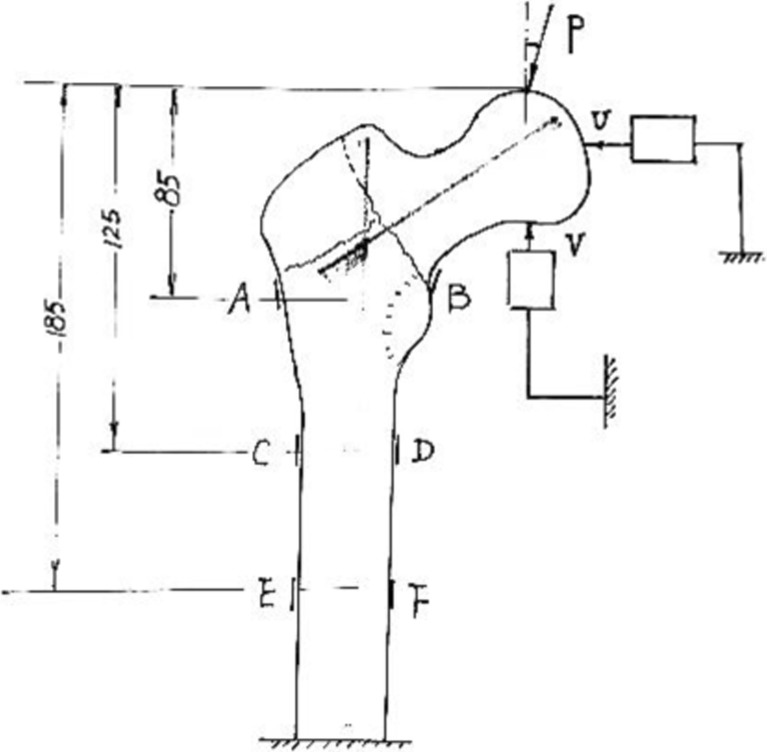
The samples were placed on WDW Equipment (Microcomputer Control Electronic Universal Testing Machine, Changchun Kexin Company, China) and step-loaded from 0 to 1,200 N at a rate of 1.5 mm/s. Horizontal displacement (U) and vertical displacement (V) of femurs were measured using KG-101 (Electrical and Mechanical Factory, Shanghai University, China). The biomechanics experimental set-up is shown in Fig. 1.
Fig. 1.
Schematic diagram of the experimental set-up for the two internal fixation femoral intertrochanteric fracture models. P load; U horizontal displacement sensor; V vertical displacement sensor; A, B, C, D, E, F resistance chip measurement locations
Statistical Analysis
SPSS 13.0 statistical software was used for statistical analysis. Mechanical parameters were compared using an independent sample t-test. Mechanical parameters of each group are presented as mean ± standard deviation ( ± S). A value of P < 0.05 was considered statistically significant. Statistical analysis involved linear regression, calculation of correlation factor according to mathematical statistics, the comparison of mechanical parameters, such as strength, rigidity, and the shifting of femoral head and so on, using two independent sample materials (t) to check, and then analyzing the differences between them.
± S). A value of P < 0.05 was considered statistically significant. Statistical analysis involved linear regression, calculation of correlation factor according to mathematical statistics, the comparison of mechanical parameters, such as strength, rigidity, and the shifting of femoral head and so on, using two independent sample materials (t) to check, and then analyzing the differences between them.
Results
Load-strain relationship of the femur
The load-strain relationships of the two internal fixation approaches for femoral intertrochanteric fractures were measured at six points along the femur (A–F; Fig. 1). The results (Table 4) indicate that: (1) the load-strain relationship is a linear relationship in the elastic range; (2) the maximum strain occurs when the intertrochanteric area is under load (P); (3) the lateral strain on the femur (OS) is converted into tensile strain, while the medial strain (IS) is converted into compressive strain; (4) an Evan’s type II fracture is unstable and exhibits greater strain than that in an Evan’s type I fracture; and (5) the strain in the InterTAN internal fixation is less than that in PFNA. Importantly, the lower strain suggests a stronger internal fixation.
Table 4.
Strain measurements at six points along the femur (A-F) for the two internal fixations methods of femoral intertrochanteric fracture ( ± S)
± S)
| Fixation type | Fracture type | (N) | Strain gauge placement | |||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |||
| InterTAN | Evan’s I | 600 | 56 ± 4 | −57 ± 5 | 90 ± 8 | −92 ± 9 | 80 ± 6 | −101 ± 9 |
| 1200 | 112 ± 9 | −114 ± 10 | 180 ± 15 | −193 ± 17 | 160 ± 13 | −202 ± 18 | ||
| Evan’s IIa | 600 | 96 ± 8 | −90 ± 7 | 88 ± 7 | −86 ± 8 | 92 ± 8 | −102 ± 9 | |
| 1200 | 192 ± 16 | −180 ± 15 | 196 ± 15 | −172 ± 16 | 184 ± 17 | −204 ± 18 | ||
| PFNA | Evan’s I | 600 | 60 ± 4 | −63 ± 4 | 96 ± 7 | −98 ± 8 | 90 ± 7 | −111 ± 9 |
| 1200 | 120 ± 8 | −125 ± 9 | 192 ± 15 | −197 ± 16 | 180 ± 14 | −223 ± 19 | ||
| Evan’s IIa | 600 | 102 ± 9 | −99 ± 8 | 95 ± 7 | −103 ± 8 | 100 ± 9 | −101 ± 9 | |
| 1200 | 204 ± 17 | −199 ± 16 | 190 ± 15 | −206 ± 17 | 200 ± 18 | −202 ± 19 | ||
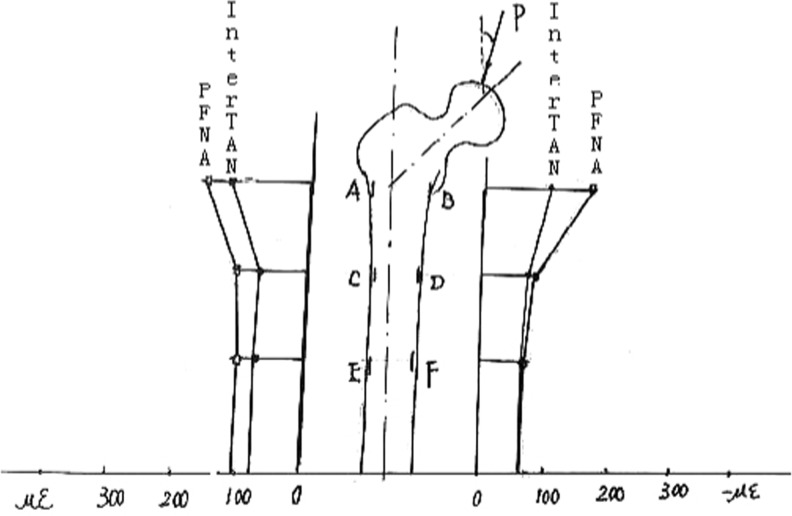
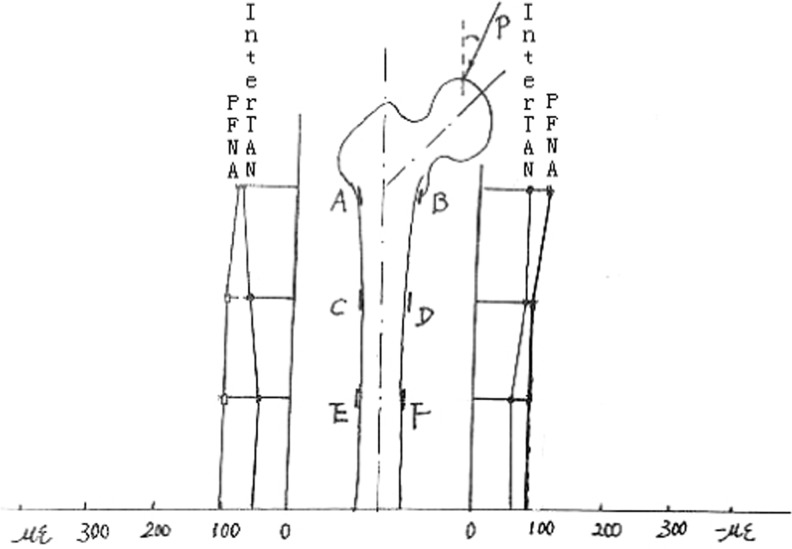
Table 5 illustrates the average strain in the two groups. The lateral and medial strain measurements for Evan’s type I and IIa fractures both demonstrated an 8 % quantitative difference between the InterTAN and PFNA fixations. Despite not being statistically different (t = 1.464, P > 0.05), these findings illustrate that the strain of InterTAN may be better than that of PFNA intramedullary nail fixation. The load-strain relationships for the two groups are shown in Figs. 2 and 3 and demonstrate that the two groups were similar.
Table 5.
The femoral lateral stain (OS) and medial strain (IS) at 1,200 N for the two internal fixations methods of femoral intertrochanteric fracture ( ± S)
± S)
| Fracture type | OS | IS | ||
|---|---|---|---|---|
| InterTan | PFNA | InterTAN | PFNA | |
| Evan’s I | 151 ± 14 | 164 ± 15 | 167 ± 16 | 181 ± 17 |
| Evan’s IIa | 184 ± 17 | 198 ± 18 | 185 ± 17 | 202 ± 19 |
Fig. 2.
The strain curve for the two internal fixations methods of Evan’s Type I femoral intertrochanteric fracture
Fig. 3.
The strain curve for the two internal fixations methods of Evan’s Type IIa femoral intertrochanteric fracture
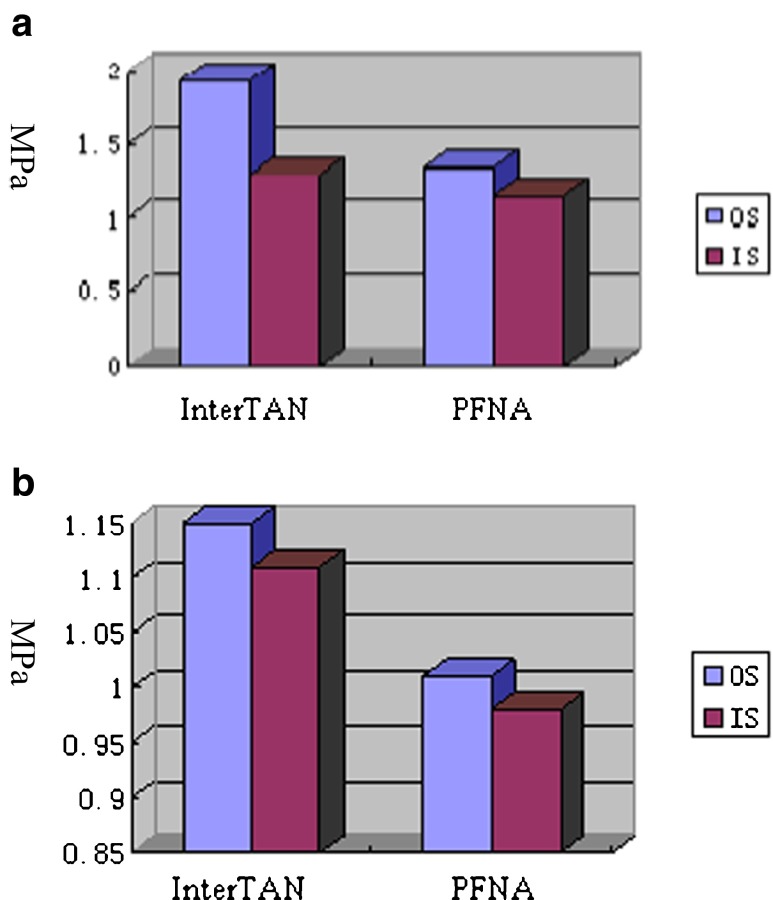
Strength of the femoral head
Strength is a mechanical index that can be used to measure the destruction-resisting ability of the femur. Table 6 and Fig. 4a,b show the results of strength measurements on both sides of the femur for the 2 different intramedullary nails for a femoral intertrochanteric fracture, under a load of 1,200 N of the hip. The results indicate that for an Evan’s Type I fracture, the difference between InterTAN and PFNA for lateral strength is 30 % and 11 % for medial strength. Furthermore, for an Evan’s Type II fracture, the differences in lateral and medial strength are 12 % and 11 %, (t = 2.688, P < 0.05). These findings show that the newly designed InterTAN nail improves and enhances femoral strength, especially for lateral fixation.
Table 6.
The strength for the two internal fixations methods of femoral intertrochanteric fracture, under a load of 1,200 N (MPa, ± S)
± S)
| Fracture type | InterTAN | PFNA | ||
|---|---|---|---|---|
| OS | IS | OS | IS | |
| Evan’s I | 1.93 ± 0.18 | 1.30 ± .12 | 1.35 ± .12 | 1.15 ± .10 |
| Evan’s IIa | 1.15 ± 0.11 | 1.11 ± 0.10 | 1.01 ± 0.10 | 0.98 ± 0.10 |
Fig. 4.
a The strength for the two internal fixations methods for femoral intertrochanteric fracture of Evan’s Type I, under a load of 12,00 N. b The strength for the two internal fixations methods for femoral intertrochanteric fracture of Evan’s Type IIa, under a load of 1,200 N
Load-displacement relationship of the femur
The femoral head will exhibit a horizontal (U) and vertical settlement displacement (V) under hip loading. The measured displacement values for the two different internal fixation methods with a load of 600 N and 1,200 N is shown in Table 7.
Table 7.
The horizontal (U) and vertical (V) displacement (mm) for the two internal fixation methods of femoral intertrochanteric fracture ( ± S)
± S)
| Fracture type | Fixation | 600 N | 1200 N | ||
|---|---|---|---|---|---|
| U | V | U | V | ||
| Evan’s I | InterTAN | 0.36 ± 0.04 | 0.48 ± 0.05 | 0.72 ± 0.06 | 0.96 ± 0.08 |
| PFNA | 0.38 ± 0.04 | 0.56 ± 0.05 | 0.76 ± 0.07 | 1.12 ± 0.11 | |
| Evan’s IIa | InterTAN | 0.40 ± 0.03 | 0.55 ± 0.04 | 0.78 ± 0.07 | 1.09 ± 0.11 |
| PFNA | 0.42 ± 0.03 | 0.59 ± 0.04 | 0.84 ± 0.07 | 1.28 ± 0.14 | |
U horizontal displacement, V vertical displacement
These results show that: (1) Under a physiological load, the displacement turns into a linear variation; (2) The displacement for the InterTAN fixation is less than PFNA intramedullary nail fixation; (3) For an Evan’s Type I fracture, the vertical settlement displacement for InterTAN is 14 %, significantly less than PFNA (t = 2.512, P < 0.05); (4) The horizontal displacement was not statistically significant between groups (t = 1.766, P > 0.05); and (5) For an Evan’s Type II fracture, the vertical displacement was 15 % lower with InterTAN, while the horizontal displacement was not different between the two fixation methods.
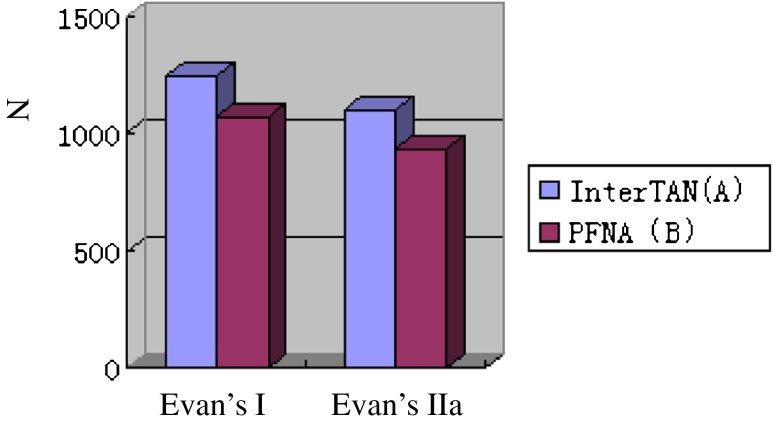
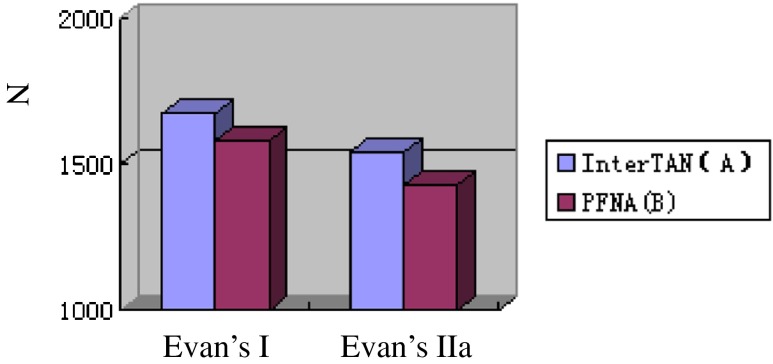
Rigidity of the femoral head
The rigidity of the femoral head refers to the capability of the femoral head to resist deformation. The measurements of axial rigidity and horizontal shear stiffness of the femoral head are shown in Table 8. The data show that for an Evan’s Type I and IIa fracture, the axial rigidity of the femoral head was 14 % and 15 % greater with InterTAN than with PFNA, respectively; the results were statistically significant (t = 2.712, P < 0.05). Thus, an InterTAN intramedullary nail is superior to a PFNA nail in resisting deformation. The horizontal shear stiffness of the femoral head with InterTan was 5 % and 7 % greater for an Evan’s Type I and Type IIa fracture, respectively, although the results were not significantly different between the two groups (t = 1.898, P > 0.05). These findings illustrate that the two fixation methods have a similar horizontal distortion-resisting capability and that InterTan is slightly better than PFNA. Figure 5 shows clear group differences in axial rigidity of the femoral head, while Fig. 6 shows the lower differences in horizontal shear stiffness between the two groups.
Table 8.
The axial rigidity (EF) and horizontal shear stiffness (GF) for the two internal fixation methods of femoral intertrochanteric fracture (N/mm; ± S)
± S)
| Measure | Evan’s I | Evan’s IIa | ||
|---|---|---|---|---|
| InterTAN(A) | PFNA(B) | InterTAN(A) | PFNA(B) | |
| EF | 1250 ± 118 | 1071 ± 105 | 1101 ± 109 | 938 ± 91 |
| GF | 1667 ± 158 | 1579 ± 141 | 1539 ± 136 | 1429 ± 129 |
EF axial rigidity, GF horizontal shear stiffness
Fig. 5.
Axial rigidity for the two internal fixation methods for Evan’s I or IIa femoral intertrochanteric fracture
Fig. 6.
Horizontal shear stiffness for the two internal fixation methods for Evan’s I or IIa femoral intertrochanteric fracture
Shear strain and strength of the femoral head
Under a strong hip load, internal fixation of intertrochanteric femoral fractures can cause the femoral neck to break, which will produce slip and coxa vara. Considering this fact, the shear strain and strength values under 1,200 N of load were measured and are presented in Table 9. The findings demonstrate that the shear strength was 3.76 ± 0.38 MPa when InterTan was used to fix femoral intertrochanteric fractures and 2.82 ± 0.30 MPa when using PFNA. This 26 % difference in shear strength between the groups was statistically significant (t = 2.868, P < 0.05). However, the shear strain of the InterTAN group was less than that of the PFNA group. These results demonstrate that using the InterTAN intramedullary nail, which has a stepwise shape, enhances the femoral head/neck and shear capability, while also improving the incidence of hip varus.
Table 9.
The shear strain and strength of the femoral head for the two internal fixation methods for a femoral intertrochanteric fracture ( ± S)
± S)
| Fixation type | Shear strain | Shear strength |
|---|---|---|
| InterTAN | 45 ± 4.42 | 3.76 ± 0.38 |
| PFNA | 62 ± 5.30 | 2.82 ± 0.30 |
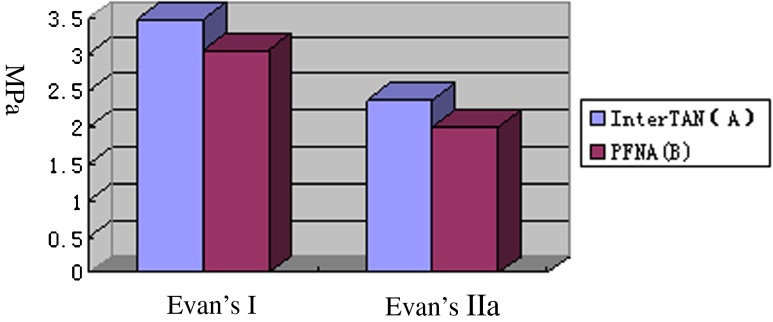
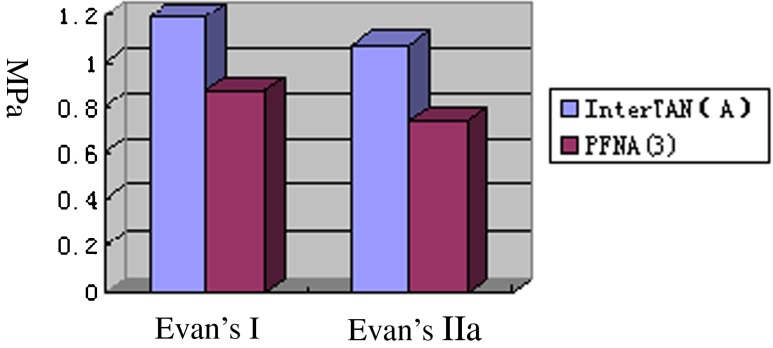
Torsional property of the femoral head
The torsional strength of the femur was measured after fixing the specimen, by rotating at a clockwise speed of 0.0320/s, and the torque, torsional angle and other torsional biomechanical properties were also evaluated. The results shown in Table 10 demonstrate that the torque with InterTAN is 12 % and 16 % lower, for an Evan’s Type 1 and Type IIa fracture, respectively, when compared to PFNA (t = 2.545, P < 0.05). The torsional rigidity was significantly higher with InterTan, compared to PFNA, for both Evan’s Type I (27 %) and IIa (31 %) fractures (t = 4.213, P < 0.05). These findings are graphically depicted in Figs. 7 and 8 and indicate that the InterTAN intramedullary nail is superior to the PFNA nail in regards to the torsional properties of a femoral intertrochanteric fracture. It is likely that these enhanced torsional characteristics are closely linked to the unique structure, ladder cross section, and tail bifurcation design of the nail, which efficiently improves the torsional properties.
Table 10.
Torsional properties of the femoral head for the two internal fixation methods for Evan’s I or IIa femoral intertrochanteric fracture ( ± S)
± S)
| Torsional property | Evan’s I | Evan’s IIa | ||
|---|---|---|---|---|
| InterTAN | PFNA | InterTAN | PFNA | |
| Torque | 3.48 ± 0.30 | 3.06 ± 0.28 | 2.38 ± 0.18 | 2.01 ± 0.17 |
| Torsional rigidity | 1.19 ± 0.08 | 0.87 ± 0.07 | 1.07 ± 0.06 | 0.74 ± 0.04 |
Fig. 7.
Torque for the two internal fixation methods of Evan’s I or IIa femoral intertrochanteric fracture
Fig. 8.
Torsion rigidity for the two internal fixation methods of Evan’s I or IIa femoral intertrochanteric fracture
Limit load of the femoral head
The strength test (limit load) of the femoral head was performed last. The standard for measuring the ultimate strength (failure in fixation) of the femoral head is when the displacement between the two points of the intertrochanteric fracture section is ≥5 mm, or the main nail screws are removed from the femoral head. Comparison of the limit load (Table 11) showed that for Evan’s Type I and IIa fractures, the load of the InterTAN nail was significantly greater (by 13 % and 12 %, respectively) than that of the PFNA nail (t = 2.366, P < 0.05). When examining the failure of the fixation methods, 60 % of the fixations failed because of a large opening in the fracture surface (≥5 mm), and 30 % of the femurs experienced a recurrent femoral intertrochanteric fracture and lose effectiveness because of the constant blasting sound and the greater downward transposition. However, the majority of the two internal fixations did not fracture or bend and only the main nail experienced a large strain.
Table 11.
Limit load for the two internal fixation methods for Evan’s Type I or IIa femoral intertrochanteric fracture (RN,  ±S)
±S)
| Measure | Evan’s I | Evan’s IIa | ||
|---|---|---|---|---|
| InterTAN | PFNA | InterTAN | PFNA | |
| Ps (KN) | 3.314 ± 0.292 | 2.880 ± 0.273 | 2.994 ± 0.214 | 2.644 ± 0.226 |
| △ (mm) | 7.82 ± 0.64 | 6.34 ± 0.57 | 8.16 ± 0.70 | 7.13 ± 0.66 |
Discussion
With the increasing age of the population and the incidence of osteoporosis, hip fractures are becoming more common. The conservative treatment of hip fractures includes bed stay, which reduces the metabolic level and bone density of the patient. Therefore, prolonged bed stay can lead to muscle atrophy and worsening of pre-existing medical conditions, and is associated with a high malformation rate and mortality. However, surgical treatment can help the patient ambulate earlier and recover joint function [5]. Although there is a general consensus regarding the operative therapy of displaced femoral intertrochanteric fractures, the management of unstable and dislocated fractures remains controversial, particularly in the elderly [6]. Hemi- or total hip arthroplasty are preferred by the majority of surgeons when treating older persons. A randomized study by Johansson et al. found that these replacement strategies are associated with fewer specific, but more general complications [7]. Because of the need for less aggressive treatment, reduced peri-operative blood loss, and conservation of the natural hip joint, in general, there is a need for new treatment concepts and osteosynthetic implants [8].
PFNA was developed and put into clinical use to solve these problems especially for elderly patients. One of the important features of the device’s design was the use of a helical neck blade with a large surface area, which is important in osteoporotic bone, and to provide rotational and angular stability [9]. Published data has stated that PFNA was a very effective method in the treatment of different types of femoral fractures [10, 11]. The new implant was aimed at the stabilization of femoral fractures in the intertrochanteric area, subtrochanteric area and pathological as well as complex complication fractures [12]. The top of the PFNA main nail has six radians, allowing the main nail to be placed smoothly in people with a wide hip, while reducing damage to the blood supply in the intra-bone marrow. In addition, PFNA uses a spiral blade to replace the two screws of PFN, which simplifies the operation and reduces the fluoroscopy and operation time. For patients with a narrow femoral neck, this approach also avoids the necessity of using two screws. The core diameter of the spiral blade increases gradually, which allows for ideal maximum bone pressure and the resultant anchor force on the cancellous bone, reducing the loss of bone mass [3]. The shape of the screw head also increases the contact between the bone and internal fixation nail, which avoids the “Z” effect of operation and prevents or delays the cutting of the femoral head caused by rotation [12]. The long tip and groove design used in PFNA also prevents concentration of local stress, which effectively reduces the morbidity of a femoral shaft fracture [13, 14]. However, it has been well demonstrated that the PFNA with a bending angle of 6° and a proximal diameter of 17 mm would cause a fracture of the proximal femur during insertion of the nail. Otherwise, a larger femoral channel should be prepared to benefit the nail insert more smoothly [15, 16]. Although the PFNA was implanted into an appropriate position, with blade being placed along the axis of the femoral neck, it was observed that the proximal part of the PFNA protruded outside the greater trochanter. About 10 % of patients presented with thigh pain due to the redundant proximal end of the nail. This was caused by the mismatch of the PFNA to the geometry of the Chinese femur [17]. After fixation of these trochanteric fractures with the locking bolt, there is a transitory ischaemia, and if the revascularization is not enough to provide a strong support for the lag screw, it may result in late mechanical failure in these fractures. All these biomechanical aspects would explain thigh pain and the possibility of postoperative fractures [18, 19]. While the PFNA was retained after healing, the higher strains were produced through the nail to the adjacent contact bone in the area of the distal locking bolt, but there was a lower strain at the neck region slightly. When comparing the risks of fracture associated between normal walking and stair climbing, it has been shown that strain and SED (strain energy density) were higher during stair climbing [20]. In addition, there were 8 % postoperative complications in patients with some implant specific complication after healing their fractures (e.g., bending, breaking of the implant, cutout of the PFNA blade, femoral head penetration of the blade or ipsilateral fractures of the femoral shaft at the tip of the implant). The possible reason may be that high stress results in a cyclic fatigue failure at the distal locking bolt hole if it is retained for a long period of times after the surgery [11, 20, 21].
In 2005, InterTAN to treat trochanteric fractures was introduced and has had a good clinical outcome and a low number of complications. This implant uses two cephalocervical screws in an integrated mechanism, which allow linear intra-operative compression and rotational stability of the head or neck fragment. InterTAN has become an increasingly popular option for treating intertrochanteric fractures [4]. The InterTAN intramedullary nail is a new generation proximal femoral nail launched by Smith-Nephew (USA). The main design features of InterTAN are as follows: (1) the proximal nail of InterTAN adopts a square cross-sectional design, which avoids the pressure on the femoral lateral wall; (2) the main nail with a 4° valgus angle is suitable for the anatomic features of the Asian femur, and is minimally invasive for the greater trochanter; (3) the original combined nail theoretically overcomes the “Z” effect; (4) it has lag screw with a diameter of 11 mm and a compression screw with a diameter of 7 mm, and when the two screws lock tightly, they can produce an alignment pressor effect within the fracture [22]; (5) the unique design can effectively disperse far-end stress and reduce the morbidity of femoral shaft fractures [23].
Several intramedullary products are currently available to the orthopaedic surgeon; however, to the best of our knowledge, there has been no research on the biomechanical performance characteristics of InterTAN and PFNA for intertrochanteric fractures healing. This is the first study to analyze the biomechanical performance of the InterTAN and PFNA for stabilizing intertrochanteric fractures. It is necessary to analyze the femoral biomechanical characteristics, such as strength, stiffness, stability, and bearing capacity of InterTAN and PFNA for further intertrochanteric fractures healing evidence.
The results of this series of biomechanical tests show that the treatment of intertrochanteric fractures should provide a strong and effective fixation, especially for elderly patients with osteoporosis. Indeed, the elderly with osteoporosis are more prone to moving of the screw or cutting of the femoral head, which can lead to failure of the fixation [24]. Therefore, implants should be chosen based on further scientific evidence.
There are several major findings from our present biomechanical testing. First, in regards to strength, the InterTAN intramedullary nail is 30 % stronger than the PFNA nail in the proximal region, which is likely related to the proximal square cross-section, and the strengthening rotational stability in the marrow cavity that allows it to compete with lateral stress and improve the supporting function of the lateral wall. Rigid fixation and ample implant stiffness are critical for minimizing interfragmentary motion and maintaining fracture reduction under load [25]. In this study, the InterTAN nail constructs had higher stiffness of the two implants. The addition of the interlocking compression screw in the InterTAN implant appears to primarily increase the stiffness of the device. The distribution of stress and strain is more homogenous for the InterTAN and we also found that the anti-deformation ability (rigidity) of the InterTAN intramedullary nail is 14–15 % stronger than the PFNA nail, although there were no significant differences between the two groups in the distal region. Overall, these findings show that for fixing the femoral head, InterTAN is more effective than PFNA fixation in resisting vertical and longitudinal displacement. Furthermore, the anti-torsion force of InterTAN intramedullary nail, compared to that of the PFNA nail, is also superior, and the torsional rigidity is enhanced by 27–30 %. The full potential of the InterTan nail is revealed when considering the unique interlocking characteristics, which improved anti-cutting out by 26 %. The unique linearity compression and stable holding force of the InterTAN also enhanced the carrying capacity by 1–13 %, compared to the PFNA nail, especially for unstable intertrochanteric fracture (i.e., Evan’s Type IIa). The InterTAN intramedullary nail is superior to the PFNA nail in regards to the torsional properties of a femoral intertrochanteric fracture. It is likely that these enhanced torsional characteristics are closely linked to the unique structure, ladder cross section, and tail bifurcation design of the nail, which efficiently improves the torsional properties.
In this study, the stabilization of intertrochanteric fractures with the InterTAN nail had substantial biomechanical advantages. The InterTAN constructs had significantly less femoral head displacement compared with specimens stabilized with PFNA. This might be because the InterTAN screws transferred the bending moments from the femoral head and neck to the cortical bone of the femoral shaft. The results of previous study also suggested that the Intertan nail could bear a patient’s full weight immediately postoperatively. Fixation with the Intertan nail provided sufficient postoperative mechanical stiffness, similar femoral head displacement, and similar tolerance of physiological loads in comminuted Pauwels III fractures compared to fractures without comminution defects [26]. Based on these biomechanical tests, we consider that the InterTAN intramedullary nail has advantages for fixation of stable and unstable intertrochanteric fractures. This in vitro study of fixation of intertrochanteric fractures revealed some biomechanical benefits possessed by the InterTAN compared with PFNA. According to our results, more biomechanical experiments investigating fixation of fractures with a posterior comminution defect are necessary. To explore the risk of construct failure with associated complicated endoprosthetic replacements, in vivo studies are required to analyze clinical outcomes after fixation of intertrochanteric fractures with the InterTAN and PFNA devices; few reports [27] were found and there is no consensus, and surgical preference may play a role [28–30]. Preclinical discovery of potential harmful qualities of orthopaedic devices should impede clinical use. Positive experimental findings should lead to further clinical testing [31].
Acknowledgment
This project was supported by “The Jinshan District Health Bureau Science Research Foundation (No. 2011-13)”.
Footnotes
Yanfeng Huang, Chunlin Zhang, Yi Luo are all co-first authors.
References
- 1.Eberle S, Gerber C, von Oldenburg G, et al. A biomechanical evaluation of orthopaedic implants for hip fractures by finite element analysis and in-vitro tests. Proc Inst Mech Eng H. 2010;224:1141–1152. doi: 10.1243/09544119JEIM799. [DOI] [PubMed] [Google Scholar]
- 2.Magu NK, Tater R, Rohilla R, et al. Functional outcome of modified Pauwels’ intertrochanteric osteotomy and total hip arthroplasty in femoral neck fractures in elderly patients. Indian J Orthop. 2008;42:49–55. doi: 10.4103/0019-5413.38581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strauss E, Frank J, Lee J, et al. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006;37:984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Ruecker AH, Rupprecht M, Gruber M, et al. The treatment of intertrochanteric fractures: results using an intramedullary nail with integrated cephalocervical screws and linear compression. J Orthop Trauma. 2009;23:22–30. doi: 10.1097/BOT.0b013e31819211b2. [DOI] [PubMed] [Google Scholar]
- 5.Fox KM, Magaziner J, Hawkes WG, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11:31–35. doi: 10.1007/s001980050003. [DOI] [PubMed] [Google Scholar]
- 6.Laursen JO. Treatment of intracapsular fractures of the femoral neck in Denmark: trends in indications over the past decade. Acta Orthop Belg. 1999;65:478–484. [PubMed] [Google Scholar]
- 7.Johansson T, Jacobsson SA, Ivarsson I, et al. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand. 2000;71:597–602. doi: 10.1080/000164700317362235. [DOI] [PubMed] [Google Scholar]
- 8.Rupprecht M, Grossterlinden L, Ruecker AH, et al. A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: the Intertan versus cannulated screws or a dynamic hip screw. J Trauma. 2011;71:625–634. doi: 10.1097/TA.0b013e31820e86e6. [DOI] [PubMed] [Google Scholar]
- 9.Kristek D, Lovrić I, Kristek J, et al. The proximal femoral nail antirotation (PFNA) in the treatment of proximal femoral fractures. Coll Antropol. 2010;34:937–940. [PubMed] [Google Scholar]
- 10.Liu Y, Tao R, Liu F, et al. Mid-term outcomes after intramedullary fixation of peritrochanteric femoral fractures using the new proximal femoral nail antirotation (PFNA) Injury. 2010;41:810–817. doi: 10.1016/j.injury.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 11.Sahin S, Ertürer E, Oztürk I, et al. Radiographic and functional results of osteosynthesis using the proximal femoral nail antirotation (PFNA) in the treatment of unstable intertrochanteric femoral fractures. Acta Orthop Traumatol Turc. 2010;44:127–134. doi: 10.3944/AOTT.2010.2237. [DOI] [PubMed] [Google Scholar]
- 12.Joseph TN, Al C, Kummer FJ, et al. The effect of posterior say on the fixation stability of intertrochantic hip fractures. J Trauma. 2002;52:544–547. doi: 10.1097/00005373-200203000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Mellano D, Grosso E, Tarello M, et al. Hip fractures: our experience in surgical treatment. Minerva Ortop Traumatol. 2006;57:361–365. [Google Scholar]
- 14.Banan H, Al-Sabti A, Jimulia T, et al. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN)–our first 60 cases. Injury. 2002;33:401–405. doi: 10.1016/S0020-1383(02)00054-2. [DOI] [PubMed] [Google Scholar]
- 15.Hwang JH, Oh JK, Han SH, Shon WY, et al. Mismatch between PFNa and medullary canal causing difficulty in nailing of the pertrochanteric fractures. Arch Orthop Trauma Surg. 2008;128:1443–1446. doi: 10.1007/s00402-008-0736-1. [DOI] [PubMed] [Google Scholar]
- 16.Simmermacher RKJ, Ljungqvist J, Bail H, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008;39:932–939. doi: 10.1016/j.injury.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Pu JS, Liu L, Wang GL et al (2009) Results of the proximal femoral nail anti-rotation (PFNA) in elderly Chinese patients. Int Orthop 33:1441–1444 [DOI] [PMC free article] [PubMed]
- 18.Vicario C, Marco F, Ortega L, et al. Necrosis of the femoral head after fixation of trochanteric fractures with gamma locking nail. A cause of late mechanical failure. Injury. 2003;34:129–134. doi: 10.1016/S0020-1383(02)00171-7. [DOI] [PubMed] [Google Scholar]
- 19.Seral B, Garcia JM, Cegonino J, et al. Finite element study of intramedullary osteosynthesis in the treatment of trochanteric fractures of the hip: Gamma and PFN. Injury. 2004;35:130–135. doi: 10.1016/S0020-1383(03)00076-7. [DOI] [PubMed] [Google Scholar]
- 20.Lizhen W, Feng Z, Jingyun H. Biomechanical study on proximal femoral nail antirotation(PFNA) for intertrochanteric fracture. J Mech Med Biol. 2012;12:1250075. doi: 10.1142/S0219519412005125. [DOI] [Google Scholar]
- 21.Sitthiseripratip K, Van Oosterwyck H, Vander Sloten J, et al. Finite element study of trochanteric gamma nail for trochanteric fracture. Med Eng Phys. 2003;25:99–106. doi: 10.1016/S1350-4533(02)00185-6. [DOI] [PubMed] [Google Scholar]
- 22.Kouvidis GK, Sommers MB, Giannoudis PV, et al. Comparison of migration behavior between single and dual lag screw implants for intertrochanteric fracture fixation. J Orthop Surg Res. 2009;4:16. doi: 10.1186/1749-799X-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Utrilla AL, Reig JS, Muñoz FM, et al. Trochanteric gamma nail and compression hip screw for trochanteric fractures: a randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005;19:229–233. doi: 10.1097/01.bot.0000151819.95075.ad. [DOI] [PubMed] [Google Scholar]
- 24.Lee PC, Hsieh PH, Chou YC, et al. Dynamic hip screws for unstable intertrochanteric fractures in elderly patients—encouraging results with a cement augmentation technique. J Trauma. 2010;68:954–964. doi: 10.1097/TA.0b013e3181c995ec. [DOI] [PubMed] [Google Scholar]
- 25.Kraemer WJ, Hearn TC, Powell JN, et al. Fixation of segmental subtrochanteric fractures. A biomechanical study. Clin Orthop Relat Res. 1996;332:71–79. doi: 10.1097/00003086-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Rupprecht M, Grossterlinden L, Sellenschloh K, et al. Internal fixation of femoral neck fractures with posterior comminution: a biomechanical comparison of DHS® and Intertan nail®. Int Orthop. 2011;35:1695–1701. doi: 10.1007/s00264-010-1199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang S, Zhang K, Jia Y, et al. InterTan nail versus Proximal Femoral Nail Antirotation-Asia in the treatment of unstable trochanteric fractures. Orthopedics. 2013;36:e288–e294. doi: 10.3928/01477447-20130222-16. [DOI] [PubMed] [Google Scholar]
- 28.Zielinski SM, Meeuwis MA, Heetveld MJ, et al. Adherence to a femoral neck fracture treatment guideline. Int Orthop. 2013;37:1327–1334. doi: 10.1007/s00264-013-1888-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneppendahl J, Grassmann JP, Petrov V, et al. Decreasing mortality after femoral neck fracture treated with bipolar hemiarthroplasty during the last twenty years. Int Orthop. 2012;36:2021–2026. doi: 10.1007/s00264-012-1600-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kannan A, Kancherla R, McMahon S, et al. Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop. 2012;36:1–8. doi: 10.1007/s00264-011-1354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Basso T, Klaksvik J, Syversen U, et al. Biomechanical femoral neck fracture experiments—a narrative review. Injury. 2012;43:1633–1639. doi: 10.1016/j.injury.2012.03.032. [DOI] [PubMed] [Google Scholar]