Abstract
Aims:
To study the outcome of endoscopic hyaluronic acid/dextranomer injection in patients with vesico-ureteric reflux (VUR).
Materials and Methods:
Sixty-three children were evaluated with a median follow up of 18 months (12-55 months) before injecting hyaluronic acid/dextranomer in a total of 99 ureteric moieties. Median age at presentation was 24 months (6-72 months). Primary VUR was the main presenting diagnosis in 60%. Patients were monitored for urinary tract infection (UTI), glomerular filtration rate (GFR), renal scarring, persistence, or appearance of contra-lateral reflux.
Results:
Grade III VUR was the most common (38%) followed by Grade IV (24%), Grade V (17%), Grade II (14%), and Grade I (7%). Most common cause for VUR was Primary (60%), followed by posterior urethral valve (PUV) (19%), bladder exstrophy (5%), anorectal malformation (ARM), epispadias, and duplex system. Analysis of patients characteristics at presentation revealed renal scarring (40%), split renal functions <35% (35%), recurrent UTI (15%), GFR <50 ml/min/1.73 m2 (15%), serum creatinine >1.4 mg/dL (10%). Complete resolution (100%) of Grade I and Grade II VUR was achieved after single injection. For Grade III VUR, single injection resolved reflux in 85.5% ureters, 100% resolution was seen after 2nd injection. In Grade IV VUR, 1st injection resolved VUR in 83.3% ureters, 95.8% ureters were reflux free after 2nd injection, and 100% resolution was seen after 3rd injection. In Grade V VUR, 94% ureters showed absent reflux after three injections.
Conclusion:
Hyaluronic acid/dextranomer injection holds promise even in higher grades of VUR.
KEY WORDS: Deflux, hyaluronic acid/dextranomer injection, outcome, vesico-ureteric reflux
INTRODUCTION
Vesico-ureteric reflux (VUR) is a urinary tract anomaly that affects approximately 1% of children and has a risk of long term renal damage.[1,2] It is commonly associated with recurrent urinary tract infection (UTI), which can lead to renal scarring and, in long term, renal insufficiency and hypertension. Purpose of treating VUR in these patients is to prevent recurrent UTI, pyelonephritis and their long term consequences. VUR is graded according to the international classification of vesico-ureteral reflux, with severity ranging from Grade I (mild) to Grade V (severe).[3] A micturating cystourethrogram (MCU) is used for diagnosing reflux and grading its severity.
Treatment of VUR can be attempted either by medical, surgical or endoscopic procedures. Long term antibiotic prophylaxis is a usual medical management, requiring close follow up. Mild cases of VUR (I and II) are likely to resolve spontaneously with increasing age but as continuing VUR has the potential to cause long-term renal damage, early diagnosis, and prevention of pyelonephritis by prophylactic antibiotic treatment are very important.[2,3,4] However, in higher grades of VUR (III, IV, and V), there is no definite advantage of medical management over surgery.[5] Since the introduction of hyaluronic acid/dextranomer in 2001, pediatric urologists have begun to change their perspective on the use of chronic antibiotics, repetitive invasive catheterization for MCU, and the invasiveness of open surgical correction of VUR. As a result, there has been a clear paradigm shift with regard to the treatment of VUR. Prior to Food and Drug Administration approval of hyaluronic acid/dextranomer for the treatment of VUR, surgical intervention was reserved for those with high-grade VUR, breakthrough infections on antibiotic prophylaxis, evidence of renal scarring, or parental preference.[6]
MATERIALS AND METHODS
This study was a retrospective single-center study done between January 2004 and November 2012. Total 63 patients (15 females and 48 males) were evaluated in our pediatric urology clinic with median follow up of 18 months (12-55 months) before injecting hyaluronic acid/dextranomer in a total of 99 ureteric moieties. Median age at presentation was 24 months (6-72 months). Out of 63 patients, 36 had bilateral disease and 27 had unilateral disease. Patients were monitored for UTI, glomerular filtration rate (GFR), renal scaring, persistence or appearance of contra-lateral reflux. VUR was diagnosed by micturating cystourethrogram (MCU) and presence of scars was documented by Tc-99-Dimercaptosuccinic acid (DMSA) scan. Split renal function (SRF) was measured by Diethylene Triamine Pentaacetic Acid (DTPA) scan. All patients were put on antibiotic prophylaxis (co-trimoxazole) for at least 6 weeks and monitored for UTI and other renal parameters. All patients were treated with endoscopic hyaluronic acid/dextranomer using sub ureteric transurethral injection (STING)[7] procedure or hydrodistention-implantation technique (HIT)[8] after counseling and informed consent. Variation of HIT, i.e., Double HIT,[6] was used in selected moieties.
Statistical analysis
We analyzed our data using the Stata software version 11.0 (Stata Corp. College Station, TX). Results were calculated as median and inter-quartile range or proportions accordingly. A 2-sided P value of 0.05 or less was considered statistically significant. Institutes ethical review board's approval was taken.
RESULTS
Most common cause for VUR was Primary (n = 38, 60%), followed by posterior urethral valve (PUV) (n = 12, 19%), bladder exstrophy (n = 5, 8%), anorectal malformat (ARM) (n = 2, 3%), epispadias (n = 1, 2%), multi cystic dysplastic kidney (n = 2, 3%), and duplex system (n = 1, 2%). Analysis of patients characteristics at presentation revealed renal scarring (40%), split renal functions <35% (35%), recurrent UTI (15%), GFR <50 ml/min/1.73 m2 (15%), serum creatinine >1.4 mg/dL (10%). In our series of patients, Grade III VUR was the most common (37, 38%) followed by Grade IV (24, 24%), Grade V (17, 17%), Grade II (14, 14%), and grade I (7, 7%). Distribution according to side of VUR was Grade I (right:left:4:3), Grade II (right:left:7:7), Grade III (right:left:17:20), Grade IV (right:left:14:10), and Grade V (right:left:9:8). There was complete resolution (100%) of VUR in Grade I and II ureters after single injection. For Grade III VUR, single injection resolved reflux in 85.5% ureters, 100% resolution was seen after 2nd injection. In Grade IV VUR, 1st injections resolved VUR in 83.3% ureters, 95.8% ureters were reflux free after 2nd injection, and 100% resolution was seen after 3rd injection. In Grade V VUR, 94% ureters showed absent reflux after three injections [Figure 1]. Resolution of VUR was documented by at least two MCU done at 3 months and 6 months after injection. Amount of hyaluronic acid/dextranomer utilized in each ureteric moiety was 0.5-8 ml (median = 2.5 ml). There was no statistical difference (P = 0.08) in amount of hyaluronic acid/dextranomer in various Grades of VUR. None of our patients had an episode of febrile UTI in due course of follow-up.
Figure 1.
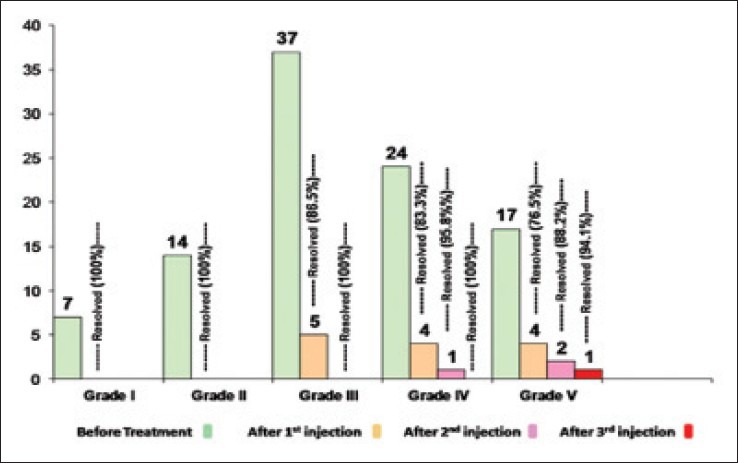
Changes in VUR grades after successful Hyaluronic acid/dextranomer injection
DISCUSSION
Diagnosis and successful management of VUR has always been prime concern of pediatric urologists, especially in children presenting with febrile UTI. The cessation of reflux and hence, febrile UTI is the final goal of management. Endoscopic management of reflux in form of injecting bulking agent in sub ureteric space preventing reflux has revolutionized the treatment protocol. The benefits of endoscopy entails visual diagnosis of any ureteric ectopia, features of bladder outlet obstruction such as diverticula and trabeculations, and presence of any other bladder anomaly which might interfere with final result of hyaluronic acid/dextranomer injection.
Endoscopic hyaluronic acid/dextranomer injection is minimally invasive procedure, requires short general anesthesia and can be done as day care procedure. The results are comparable in higher grades of VUR (94% resolution rate after three sessions of injection hyaluronic acid/dextranomer) to the open ureteric reimplantation (95% resolution rate).[4] In lower Grades of VUR, it is far more effective in cessation of reflux and prevention of febrile UTI. Garge and colleagues have reported improved health related quality of life after treatment with endoscopic injection of hyaluronic acid/dextranomer.[9]
CONCLUSION
Hyaluronic acid/dextranomer can be used safely in patients with various grades of VUR, although patient selection and close monitoring of response to treatment is required. Resolution rate of VUR by hyaluronic acid/dextranomer using various techniques is quite high.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jacobson SH, Hansson S, Jakobsson B. Vesico-ureteric reflux: Occurrence and long-term risks. Acta Paediatr Suppl. 1999;88:22–30. doi: 10.1111/j.1651-2227.1999.tb01315.x. [DOI] [PubMed] [Google Scholar]
- 2.Riccabona M. Management of recurrent urinary tract infection and vesicoureteral reflux in children. Curr Opin Urol. 2000;10:25–8. doi: 10.1097/00042307-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Medical versus surgical treatment of primary vesicoureteral reflux: Report of the International Reflux Study Committee. Pediatrics. 1981;67:392–400. [PubMed] [Google Scholar]
- 4.Elder JS, Peters CA, Arant BS, Jr, Ewalt DH, Hawtrey CE, Hurwitz RS, et al. Pediatric vesicoureteral reflux guidelines panel summary report on the management of primary vesicoureteral reflux in children. J Urol. 1997;157:1846–51. [PubMed] [Google Scholar]
- 5.Smellie JM, Barratt TM, Chantler C, Gordon I, Prescod NP, Ransley PG, et al. Medical versus surgical treatment with severe bilateral vesicouretric reflux and bilateral nephropathy: A randomised trial. Lancet. 2001;357:1329–33. doi: 10.1016/S0140-6736(00)04520-7. [DOI] [PubMed] [Google Scholar]
- 6.Molitierno JA, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux using dextranomer hyaluronic acid copolymer. J Pediatr Urol. 2008;4:221–8. doi: 10.1016/j.jpurol.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Puri P. Ten year experience with subureteric Teflon (polytetrafluoroethylene) injection (STING) in the treatment of vesico-ureteric reflux. Br J Urol. 1995;75:126–31. doi: 10.1111/j.1464-410x.1995.tb07296.x. [DOI] [PubMed] [Google Scholar]
- 8.Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: Improved results with submucosal implantation within the intramural ureter. J Urol. 2004;171:2413–6. doi: 10.1097/01.ju.0000127754.79866.7f. [DOI] [PubMed] [Google Scholar]
- 9.Garge S, Menon P, Narasimha Rao KL, Bhattacharya A, Abrar L, Bawa M, et al. Vesicoureteral reflux: Endoscopic therapy and impact on health related quality of life. J Indian Assoc Pediatr Surg. 2013;18:11–5. doi: 10.4103/0971-9261.107009. [DOI] [PMC free article] [PubMed] [Google Scholar]


