Figure 5.
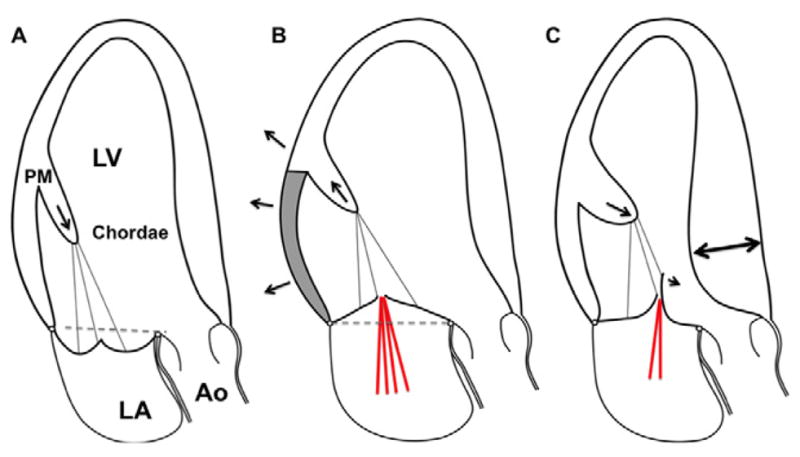
A. Mitral valve prolapse: The schematic shows bileaflet mitral valve prolapse, with superior displacement of the papillary muscle tip, “tugged” by the leaflets, and excessive leaflet and chordal tissue and mobility. Leaflet coaptation is displaced into the left atrium superior to the annular plane (dashed line). B. Functional/ischemic mitral regurgitation: The papillary muscle (medial in inferior myocardial infarction) is displaced posteriorly, laterally and, to the extent allowed by the chords, apically (arrow) due to left ventricular local dilatation & remodeling (arrows) caused by MI (shaded area). The LV wall-PM displacement tethers the mitral leaflets apically and limits coaptation. There is 20 often not enough leaflet tissue to compensate for leaflet tenting (area apical to the dashed line), resulting in mitral regurgitation (red lines). C. Hypertrophic cardiomyopathy: The geometry of the left ventricle and papillary muscles is altered by myocardial hypertrophy (interventricular septum, double arrow). The papillary muscles are enlarged and displaced anteriorly (arrow) and closer to each other (not shown). This decreases intercommissural leaflet tension and moves the coaptation point and distal leaflets toward the left ventricular outflow tract. Like a sail catching a breeze, the distal anterior leaflet and/or posterior leaflet if elongated, is at risk of being displaced into the LV outflow tract by blood-flow drag. If anterior leaflet displacement is severe enough and posterior leaflet apposition restricted, mitral regurgitation will occur (red lines). (Ao, aorta; LA, left atrium; LV, left ventricle; PM, papillary muscle).
