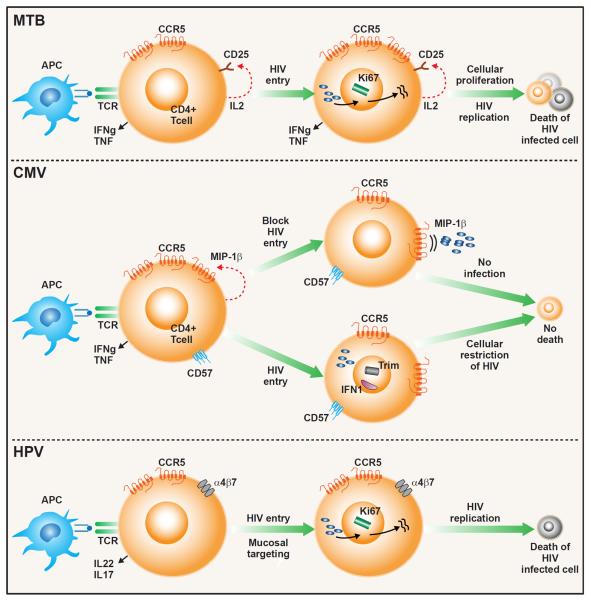
Figure 2. Proposed model for HIV-associated depletion of pathogen-specific CD4 T cells.
(Top panel) Mtb-specific CD4 T cell is activated upon binding to its cognate antigen on an HIV infected antigen-presenting cell (APC). T cell activation induces secretion of IL-2 and up-regulation of CD25 (IL-2 receptor) and CCR5 (HIV co-receptor). Binding of IL-2 to CD25 induces cellular proliferation (expression of proliferation marker Ki67) and promotes viral replication leading to productive HIV infection and cell death. (Middle Panel). Upon activation, CMV-specific CD4 T cells produce MIP-1β, which binds to its ligand, CCR5, an HIV co-receptor, blocking HIV entry into the cell. Binding of MIP-1β to CCR5 may also down-regulate CCR5 further impeding HIV entry. CMV-specific CD4 T cells express CD57, a marker to replicative senescence, and do not enter the cell cycle, limiting HIV viral replication. Expression of TRIM and Type I IFN may further restrict HIV replication. These cells are less susceptible to productive HIV infection and targeted depletion. (Bottom Panel). Activation of cervical CD4 cells leads to increased expression of both CCR5 and the mucosal homing receptor, integrin α4β7, which binds to HIV gp120. Co-expression of these receptors increases susceptibility to HIV infection. These cells are also highly activated (express Ki67), promoting HIV replication, leading to productive infection and cell death.