Abstract
Background
We sought to compare direct costs and clinical and radiographic outcomes for distal radius fractures (DRF) treated with open reduction internal fixation with volar locking plates (VLP) versus closed reduction and percutaneous pinning (CRPP).
Methods
We identified patients with AO-type A and C1 DRFs from a prospective database. Outcomes were assessed at 6 weeks and at 3, 6 and 12 months, and surgical care costs were estimated.
Results
Twenty patients were treated with CRPP and 24 with VLP. There were no significant differences in patient-rated wrist evaluation (PRWE) scores between the 2 groups at any time point (mean 16.2 ± 23.1 in the CRPP group v. 21.5 ± 23.6 in the VLP group, p = 0.91). Overall alignment was maintained in both groups; however, there was a greater loss of radial height over time with CRPP than VLP (0.97 mm v. 0.25 mm, p = 0.018). The mean duration of surgery was longer for VLP than CRPP (113.9 ± 39.5 min v. 86.5 ± 7.8 min, p = 0.029), but there were fewer clinic visits (5.2 ± 1.4 v. 7.8 ± 1.3, p < 0.001) and fewer radiographs (7.4 ± 2.7 v. 9 ± 2.4, p = 0.031). The total cost per case was greater for VLP than CRPP ($1637.27 v. $733.91).
Conclusion
Based on PRWE scores, VLPs did not offer any significant advantage over CRPP in patients with simple fracture types between 3 and 12 months, but they were much more costly. Whether VLP offers any functional advantage earlier in recovery, thereby justifying their expense, requires further investigation in the form of a prospective randomized trial with a detailed cost analysis.
Abstract
Contexte
Nous avons voulu comparer les coûts directs et l’issue clinique et radiographique du traitement des fractures du radius distal (FRD) au moyen d’une technique de réduction ouverte avec fixation interne par plaques palmaires de stabilisation (PPS) par rapport à la méthode par réduction fermée et enclouage percutané (RFEP).
Méthodes
Nous avons recensé les patients victimes d’une FRD de type AO et de type C1 à partir d’une base de données prospectives. L’issue de ces fractures a été évaluée après 6 semaines, puis après 3, 6 et 12 mois et nous avons estimé les coûts des soins chirurgicaux.
Résultats
Vingt patients ont été traités par RFEP et 24 par PPS. On n’a noté aucune différence significative entre les 2 groupes quant aux scores d’évaluation des poignets par les patients eux-mêmes, peu importe le moment de l’évaluation (moyenne 16,2 ± 23,1 dans le groupe traité par RFEP c. 21,5 ± 23,6 dans le groupe traités par PPS, p = 0,91). L’alignement global a été maintenu dans les 2 groupes; toutefois, on a observé une diminution plus marquée de la longueur du radius avec le temps dans les cas de RFEP que dans les cas de PPS (0,97 mm c. 0,25 mm, p = 0,018). La durée moyenne de la chirurgie a été plus longue avec la PPS qu’avec la RFEP (113,9 ± 39,5 min c. 86,5 ± 7,8 min, p = 0,029), mais les visites à la clinique et les radiographies ont été moins nombreuses (respectivement, 5,2 ± 1,4 c. 7,8 ± 1,3, p < 0,001 et 7,4 ± 2,7 c. 9 ± 2,4, p = 0,031). Le coût total par cas a été plus élevé avec la PPS qu’avec la RFEP (1637,27 $ c. 733,91 $).
Conclusion
Compte tenu des scores d’évaluation du poignet par les patients eux-mêmes, la PPS n’a pas sembler offrir d’avantages significatifs par rapport à la RFEP après 3 et 12 mois chez les patients présentant des types de fractures simples, mais elle s’est révélée beaucoup plus coûteuse. Il reste encore à vérifier, au moyen d’un essai prospectif randomisé assorti d’une analyse de coûts détaillée, si la PPS offre des avantages fonctionnels plus tôt lors du rétablissement, ce qui en justifierait le coût.
The introduction of locking plate technology has greatly influenced treatment of distal radius fractures (DRFs) in recent years. In the last decade, there has been an exponential increase in the number of DRFs treated with locking plates. In 1999, trainees in the United States preparing for board certification treated 58% of DRFs with closed reduction and percutaneous pinning (CRPP), whereas in 2007 only 19% of these injuries were treated with CRPP.1 Even in older patients in whom the use of internal fixation has generally been less frequent, the use of internal fixation has increased in recent years. In 2005, 16% of all DRFs were treated with internal fixation compared with 3% in 1997.2 In 2007, United States Medicare payments were $170 million for the management of DRFs. It has been estimated that if the use of internal fixation to treat DRFs increases to 50%, DRF-attributable payments could be nearly $240 million.2
Many surgeons assume that volar locking plates (VLPs) are associated with fewer complications, better function and improved patient satisfaction than other treatment methods. Kreder and colleagues3 studied displaced intra-articular fractures and found that patients who underwent indirect reduction and percutaneous fixation had a more rapid return of function and a better functional outcome than those who underwent open reduction and internal fixation (ORIF; although the authors did not study locking plate technology). They recommended that ORIF be preceded by an attempt at minimally invasive percutaneous reduction.3 This finding contrasts with those of Rozental and colleagues,4 who studied unstable extra-articular or simple intra-articular fractures treated with ORIF or CRPP. They concluded that both are effective methods for treatment of these injuries; however, they reported that better functional results could be expected in the early postoperative period with ORIF.4 McFayden and colleagues5 also reported improved clinical outcomes in the early postoperative course when comparing VLPs with percutaneous fixation for unstable extra-articular fractures. They concluded their follow up at 6 months, so it is difficult to determine if any long-term differences exist. Leung and colleagues6 found that at 24 months, results for plate fixation were significantly better than percutaneous pin fixation for intra-articular fractures.
Studies on the treatment of DRFs are difficult to compare, as different outcome tools are used, different plates are used for fixation and the complexity of included fractures varies widely. Because complex fractures are also included, many patients treated with percutaneous pinning also required supplementation with external fixation. For these reasons, despite the vast amount of literature available, clear recommendations cannot be made for simple fracture types based on validated patient-rated outcomes. The most recent review by the American Academy of Orthopaedic Surgeons (AAOS) lists several recommendations with respect to treatment of these injuries, but does not recommend the type of fixation to use for specific fracture types.7
In most of the studies mentioned previously, the cost of the different treatment modalities is ignored. Given the widespread problem of rapidly escalating health care costs, the cost of these interventions must be considered, particularly when outcomes are similar between 2 choices. Shauver and colleagues8 stated that despite the increased price of these implants, cost–utility calculations have shown that from a societal perspective, ORIF is considered a worthwhile alternative to casting.8 They concluded that there was a slight preference for ORIF compared with casting for faster return to minimally restricted activity. For patients treated surgically, cost and long-term outcomes were similar regardless of fixation type, and as a result the study found that patients showed little preference for one treatment type over the other.8 Looking at VLP more specifically, to our knowledge, only 1 study has compared the cost of VLP to CRPP. Shyamalan and colleagues9 reported that treatment of a DRF with VLP cost 3 times more than treatment with Kirschner wire fixation (k-wires) and casting (£2212 v. £662).9 Unfortunately, their study had a small sample size (n = 20), was retrospective and did not include any clinical or radiographic outcomes, making it difficult to put the cost comparison into context.
Although VLP likely offers an advantage over CRPP in patients with fractures that are comminuted or complex, we questioned whether VLPs are being overused in patients with simple fracture types that would have been traditionally treated with percutaneous pins and plaster, thus contributing to escalating health care costs. The purpose of this study was to compare clinical and radiographic outcomes in a prospective cohort of patients wtih extra-articular or simple intra-articular DRFs treated with VLP or CRPP and to compare the costs of these 2 techniques.
Methods
We identified patients with DRFs treated at a tertiary care centre between 1997 and 2009 from an existing prospective database. Surgeon preference dictated the type of surgery these patients received; the patients were not involved in other studies and therefore were not randomized. Our inclusion criteria were AO type A extra-articular or type C1 simple intra-articular DRFs treated with either percutaneous k-wire fixation or VLP in skeletally mature individuals. One year of follow-up data was also required. We excluded patients with any complex or comminuted intra-articular fracture types (AO type C2 or more complex). We also excluded patients who underwent methods of fixation other than CRPP or VLP.
The primary outcome was the patient-rated wrist evaluation (PRWE) score. The PRWE is a reliable, valid measure of patient-rated pain and disability.9 Secondary outcomes included range of motion and grip strength. Patients were evaluated prospectively at 6 weeks and at 3, 6 and 12 months postoperatively. Radiographs were reviewed by at least 2 individuals: a fellowship trained orthopaedic surgeon (R.G.) and a senior level orthopaedic resident (I.D.). We assessed change in ulnar variance, radial inclination and volar tilt by comparing the earliest posttreatment radiograph with radiographs taken at the 1-year follow-up. Complications associated with each treatment were also identified.
We estimated the cost of each treatment arm retrospectively. To estimate surgical costs, we reviewed patients’ health care records to determine the length of time each patient spent in the operating room (OR). We estimated the OR cost at $121/h (i.e., 2.5 registered nurses at $40/h, and 1 attendant at $21/h). In addition, we estimated the cost of hardware based on current institutional costs of VLP ($750: cost of plate + 5 locking screws + 1 cortical screw) and k-wires ($40: cost of 4 k-wires). We estimated other direct health care costs by evaluating the number of clinic visits and radiographs taken throughout the duration of treatment. Nursing cost at the first postoperative visit was estimated at $9 (chart review, filling in radiography requisitions, set-up of patient, suture removal and pin site care for a total estimated time of 20 minutes). Subsequent visits were estimated to cost $5 each with an estimated time of 10 minutes per patient. Estimated costs for each radiograph taken included $21.05, billed to the Ontario Health Insurance Plan (OHIP), for a standard wrist radiograph with 2 views and $7 for technician time (average of 4–7 minutes) for a total cost of $28.05 for each radiograph taken. According to the Ontario Ministry of Health and Long-Term Care Schedule of Benefits, the surgeon fee for open reduction (F030) is $420, and the surgeon fee for closed reduction (F046) plus 50% for percutaneous pinning is $224.02.
Statistical analysis
We analyzed categorical variables using the χ2 test, and continuous variables were compared using a 2-tailed Student t test.
Results
Participants
Forty-four patients satisfied the inclusion criteria. A total of 20 patients (90% of them having intra-articular DRFs) were treated with CRPP, and 24 (87.5% of them having intra-articular DRFs) were treated with ORIF using a VLP. We compared the 2 groups on the basis of age, sex, handedness and workers’ compensation benefits (Table 1). The only significant difference between the groups was age (mean 40.3 ± 12.4 yr for patients in the CRPP group v. 50.3 ± 14.7 yr for patients in the VLP group, p = 0.009).
Table 1.
Demographic and clinical characteristics of patients who underwent closed reduction with percutaneous pinning or open reduction and internal fixation with volar locking plates to treat distal radius fractures
| Variable | Group; no. (%)* | p value | |
|---|---|---|---|
| CRPP, n = 20 | VLP, n = 24 | ||
| Age, yr; mean ± SD | 40.3 ± 12.4 | 50.3 ± 14.7 | 0.009 |
| Sex, female | 15 (75) | 17 (70.8) | 0.76 |
| Fracture distribution (% intra-articular) | 18 (90) | 21 (87.5) | 0.72 |
| Dominant hand involved | 9 (45) | 11 (47.8) | 0.96 |
| WSIB involvement | 1 (5) | 2 (8.3) | 0.66 |
CRPP = closed reduction and percutaneous pinning; SD = standard deviation; VLP = volar locking plates; WSIB = Workplace Safety and Insurance Board.
Unless otherwise indicated.
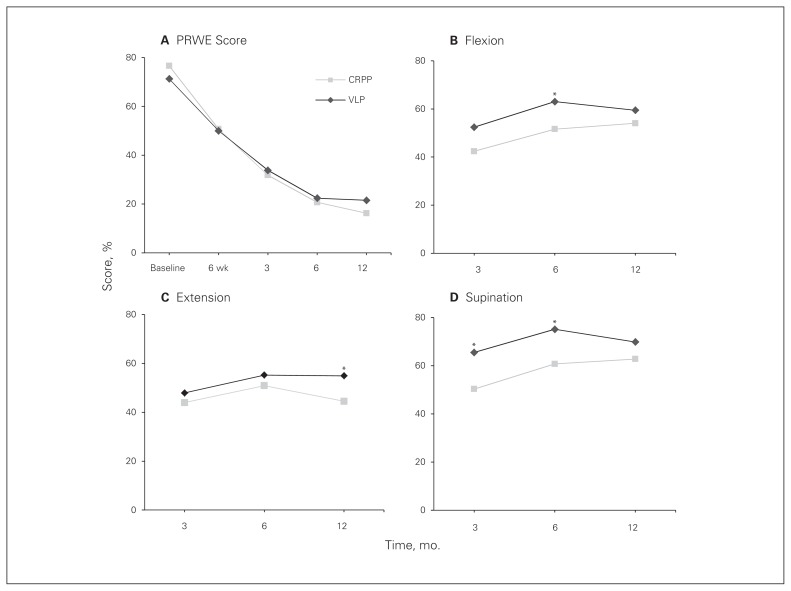
Patient-reported outcomes
Comparing the PRWE scores between the 2 groups yielded no significant difference at any time point between 6 weeks and 1 year (p = 0.91, mean difference 3.0 out of a total possible score of 100 for PRWE; Fig. 1A).
Fig. 1.
Comparison of (A) patient-rated wrist evaluation (PRWE) scores, (B) flexion, (C) extension and (D) supination in patients who underwent closed reduction and percutaneous pinning (CRPP) or open reduction and internal fixation with volar locking plates (VLP) to treat distal radial fractures. *p < 0.05.
Objective outcomes
Grip strength and range of motion (specifically flexion, extension, supination, pronation, radial deviation and ulnar deviation) were assessed at 3, 6 and 12 months. The VLP group showed improved flexion at 6 months compared with the CRPP group (63° v. 51°, p = 0.022; Fig. 1B). The CRPP group showed improved extension at 1 year compared with the VLP groups (55° v. 44°, p = 0.008; Fig. 1C). Supination was greater in the VLP group than the CRPP group at 3 months (66° v. 50°, p = 0.021) and 6 months (75° v. 61°, p = 0.018; Fig. 1D). We found no significant differences between the groups for pronation, radial deviation, ulnar deviation or grip strength (Table 2).
Table 2.
Objective outcomes for radial deviation, ulnar deviation, pronation and grip strength
| Outcome; time | CRPP | VLP | p value |
|---|---|---|---|
| Radial deviation | |||
| 3 mo | 20.8 | 14.1 | 0.06 |
| 6 mo | 19.0 | 17.9 | 0.40 |
| 12 mo | 17.4 | 17.4 | 0.50 |
| Ulnar deviation | |||
| 3 mo | 24.5 | 22.2 | 0.33 |
| 6 mo | 24.1 | 25.3 | 0.35 |
| 12 mo | 27.4 | 22.6 | 0.07 |
| Pronation | |||
| 3 mo | 63.4 | 71.1 | 0.07 |
| 6 mo | 74.2 | 72.3 | 0.32 |
| 12 mo | 75.9 | 73.5 | 0.26 |
| Grip strength | |||
| 3 mo | 14.1 | 17.7 | 0.15 |
| 6 mo | 25.6 | 24.5 | 0.44 |
| 12 mo | 20.6 | 24.9 | 0.13 |
CRPP = closed reduction and percutaneous pinning; VLP = volar locking plates.
Radiographic outcomes
Both groups had similar fracture types and had excellent reductions with no significant loss of alignment over time. When comparing preoperative to postoperative images taken at 1 year, we found no significant differences between the groups for change in radial inclination (p = 0.09) or volar tilt (p = 0.29). The CRPP group experienced a greater loss of radial height over time than the VLP group (0.97 mm v. 0.25 mm, p = 0.018).
Complications
There was no significant difference in the complication rate between the 2 groups (p = 0.24). Three (15%) patients in the CRPP group and 1 (4.2%) patient in the VLP group experienced complications. In the CRPP group, 1 patient had mild, transient median nerve compression, which resolved without any specific treatment. Another patient had complex regional pain syndrome, which also resolved without any specific therapy. One patient had a superficial pin site infection that resolved with oral antibiotics. In the VLP group, 1 patient experienced mild, transient median nerve symptoms that resolved without any specific intervention.
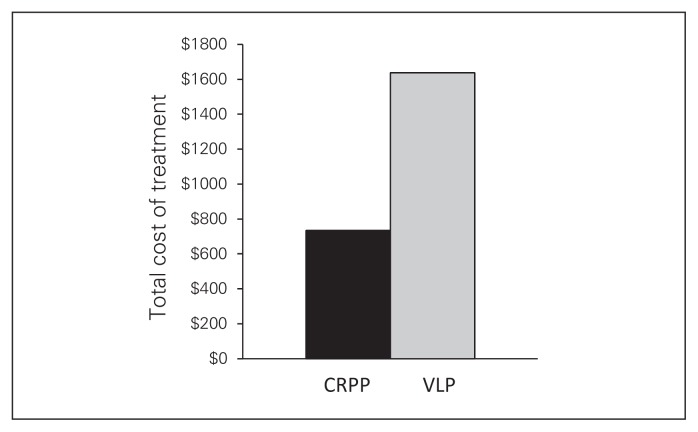
Cost estimation
Total cost was estimated based on OR cost, cost per clinic visit, cost for each radiograph taken, cost of the implant, and surgeon billing. The VLP group required 27 more minutes of operative time than the CRPP group (p = 0.029). The OR cost associated with CRPP was $174.44 compared with a VLP cost of $229.70 (Table 3).
Table 3.
Cost estimation of closed reduction with percutaneous pinning versus open reduction and internal fixation with volar locking plates to treat distal radius fractures
| Costs | Group; mean ± SD* | p value | |
|---|---|---|---|
| CRPP | VLP | ||
| OR | 0.029 | ||
| Time, min. | 86.5 ± 7.8 | 113.9 ± 39.5 | |
| Cost, $121/h | $174.44 | $229.70 | |
| Clinical | < 0.001 | ||
| No. visits | 7.8 ± 1.3 | 5.2 ± 1.4 | |
| Nursing costs, $9/first visit and $5/subsequent visits | $43 | $30 | |
| Radiographs | 0.031 | ||
| No. films ordered | 9 ± 2.4 | 7.4 ± 2.68 | |
| Cost, $28.05/film | $252.45 | $207.57 | |
| Implants | |||
| No. used per case | 4 k-wires | 5 hole VLP + screws (5 locking screws + 1 cortical screw) | |
| Cost | $40 | $750 | |
| Surgeon costs | $224.02 | $420 | |
| Total cost of treatment/case | $733.91 | $1637.27 | < 0.001 |
CRPP = closed reduction and percutaneous; OR = operating room; SD = standard deviation; VLP = volar locking plates.
Unless otherwise indicated.
We also estimated costs associated with clinic visits. The CRPP group had more clinic visits than the VLP group (7.8 v. 5.2, p < 0.001), for a greater cost ($43 v. $30). The CRPP group also had more radiographs taken than the VLP group (9 v. 7.4, p = 0.031), for a cost of $252.45 versus $207.57 (Table 3).
Implant costs for the VLP group were also substantially higher than those for the CRPP group. The estimated cost of a 5 hole locking plate with 5 locking screws and 1 cortical screw is approximately $750. This is in comparison to the estimated cost of an individual k-wire, which is approximately $10 (Table 3). According to the Ontario Ministry of Health and Long-Term Care Schedule of Benefits, the surgeon fee for open reduction (F030) is $420, whereas the fee for closed reduction (F046) plus 50% for percutaneous pinning is $224.02 Taking all the above components together, the overall cost estimation for treatment with CRPP was $733.91 versus a cost of $1637.27 for VLP (Fig. 2).
Fig. 2.
Estimated total cost of closed reduction and percutaneous pinning (CRPP) versus open reduction and internal fixation with volar locking plates (VLP) to treat distal radial fractures.
Discussion
Distal radius fractures are extremely common injuries. Many different treatment methods have been advocated, including CRPP, external fixation and ORIF. Recent advances in plate design have certainly impacted treatment of these injuries. With the introduction of locking plate technology, greater portions of patients with these injuries have been treated with ORIF in recent years.1 Even within our own institution, there has been an exponential increase in the use of VLPs leading to substantially higher costs. Despite the obvious shift in treatment modality, the literature suggests no long-term difference between the 2 treatment strategies and remains inconsistent in support of short-term advantages.
Studies suggest that differences between fixation types may be short-lived and that long-term outcomes are similar. Wei and colleagues10 compared results for unstable DRFs treated with external fixation, VLPs or radial column plates. At 6 months and 1 year, outcomes for each group were found to be excellent, with minimal differences in strength, motion and radiographic alignment.10 Similarly, Egol and colleagues11 compared external fixation with supplementary k-wire fixation to VLPs for unstable DRFs. Although the VLP group experienced a significant early improvement in range of motion, this advantage diminished over time.11 In our patient population, VLP fixation did not provide any clear advantage over CRPP for the clinical outcomes measured. Our study did not identify any significant difference in overall PRWE scores.
Similarly, the long-term radiographic parameters we assessed also were similar between the 2 groups. There was no significant difference in radial inclination or volar tilt. The CRPP group did, however, experience a greater loss in radial height than the VLP group (0.97 mm v. 0.25 mm), which we found to be statistically significant. Whether this small a difference has any clinical relevance is unknown. The similar outcomes in PRWE scores with a similar range of motion would indicate that this difference in radial height did not impact clinical outcomes. The complication rate for each group was also low and compared favourably with the rates reported in the literature.
Despite long-term results showing similar outcomes, some studies reported differences in short-term outcomes. Rozental and colleagues4 compared VLP fixation to percutaneous fixation and casting or external fixation and found better functional results in the early postoperative period with ORIF. This difference was particularly pronounced at 6 weeks and 9 weeks after the injury and then decreased over time. They recommended that this form of treatment be considered for patients requiring a faster return to function after injury.4 Kreder and colleagues3 compared internal fixation with indirect percutaneous reduction and external fixation for displaced intra-articular fractures and found that patients who underwent indirect reduction and percutaneous fixation had a more rapid return to function and a better functional outcome.3 Although they did not include a formal cost comparison, our estimation of cost of internal fixation would give added incentive to attempt percutaneous fixation according to the superior results of Kreder and colleagues.
With no long-term difference, selecting a particular method of fixation might be justified if improved results could be found early in the postoperative course. Improved results in the short term could be in the form of subjective symptom relief or they could be economic in nature. Economic analyses that include the patient perspective or that consider disability costs would improve our understanding of the overall economic benefit of fracture management. In a previous study,12 we demonstrated that 20% of patients were able to return to work immediately after fracture treatment and that median time off work was 8 weeks. Occupational demands and self-reported disability were predictive of the length of time patients were absent from work, whereas radiographic parameters were not. Thus, future studies would need to determine whether earlier recovery of motion equates to earlier return to work.
Given the economic constraints in health care, cost should be considered when deciding on a treatment strategy. None of the studies mentioned previously took into account the cost of the implants they used. To date, the only known cost analysis of treating DRFs is the one per-formed by Shyamalan and colleagues.9 They reported that treatment of a DRF with VLP cost 3 times more than treatment with CRPP and casting (£2212 v. £662).9 Similarly, our estimations demonstrate that treatment with VLP fixation more than doubles the cost associated with CRPP ($1217.27 v. $509.89). Shyamalan and colleagues focused on a cost analysis and did not include clinical or radiographic outcomes, an important weakness of their study. In the absence of any clear clinical benefit, cost should be considered in the decision on how to treat these common injuries.
Limitations
The present study had several limitations. Our sample size was small and may have been underpowered to detect treatment differences. A small sample size would not have affected the large difference we saw in our cost estimation, but may have played a role in identifying significant differences in clinical outcomes given that these differences were quite small. In addition, our cohort was not randomized and was therefore subject to potential biases. Although the data were collected prospectively, the study question was posed retrospectively. In performing a cost analysis, it would be ideal to include hospital, patient and societal costs; a limitation of our study was that we were unable to include societal (e.g., work disability) or patient costs (e.g., cost of therapy) in our estimation. Finally, the earliest outcome evaluations had already been prespecified at 3 months. Therefore, we are unable to determine whether there were any short-term benefits to patients in terms of pain and disability earlier in the postoperative period.
Strengths of our study included the fact that only patients with simple fracture types were included. By not combining populations with simple and complex fracture types, we were able to draw specific conclusions with respect to simple fracture types. In addition, to our knowledge, no other study published thus far has included both radiographic and clinical outcomes combined with a cost analysis.
A larger, more detailed economic analysis that considers the cost perspective of patients and society, including costs of lost productivity, in the early phases of recovery would be warranted given that there is no current long-term advantage demonstrated for VLP. If future studies were to report that patients could return to work safely and sooner with VLP than CRPP, the increased cost associated with VLPs could be justified.
Conclusion
Despite the substantially greater cost, no significant long-term advantages were identified in patients with simple DRFs treated with VLP versus CRPP. It is unknown whether treatment with VLP offers an advantage in the short term (< 3 mo). Until future studies can demonstrate a more clear advantage of using VLP, CRPP continues to provide a safe and cost-effective option for treating extra-articular or simple intra-articular DRFs.
Footnotes
Competing interests: None declared.
Contributors: I. Dzaja and R. Grewal designed the study. I Dzaja and J.C. MacDermid acquired the data, which I. Dzaja, J.H. Roth and R. Grewal analyzed. I. Dzaja, J.C. MacDermid and R. Grewal wrote the article, which all authors reviewed and approved for publication.
References
- 1.Koval KJ, Harrast JJ, Anglen JO, et al. Fractures of the distal part of the radius: the evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90:1855–61. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 2.Shauver MJ, Yin H, Banerjee M, et al. Current and future national costs to medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36:1282–7. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 3.Kreder HJ, Handel DP, Agel J, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomized, controlled trial. J Bone Joint Surg Br. 2005;87:829–36. doi: 10.1302/0301-620X.87B6.15539. [DOI] [PubMed] [Google Scholar]
- 4.Rozental TD, Blazar PE, Franko OI, et al. Functional outcomes for unstable distal radius fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. J Bone Joint Surg Am. 2009;91:1837–46. doi: 10.2106/JBJS.H.01478. [DOI] [PubMed] [Google Scholar]
- 5.McFadyen I, Field J, McCann P, et al. Should unstable extra-articular distal radius fractures be treated with fixed-angle volar-locked plates or percutaneous Kirschner wires? A prospective randomized controlled trial. Injury. 2011;42:162–6. doi: 10.1016/j.injury.2010.07.236. [DOI] [PubMed] [Google Scholar]
- 6.Leung F, Tu YK, Chew WY, et al. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radius fractures. A randomized study. J Bone Joint Surg Am. 2008;90:16–22. doi: 10.2106/JBJS.F.01581. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Orthopaedic Surgeons. The treatment of distal radius fractures: guideline and evidence report. 2009. [accessed 2013 Oct. 18]. Available: www.aaos.org/research/guidelines/drfguideline.pdf.
- 8.Shauver MJ, Clapman PJ, Chug KC. An economic analysis of outcomes and complications of treating distal radius fractures in the elderly. J Hand Surg Am. 2011;36:1912–8. doi: 10.1016/j.jhsa.2011.09.039. [DOI] [PubMed] [Google Scholar]
- 9.Shyamalan G, Theokli C, Pearse Y, et al. Volar locking plates versus Kirschner wires for distal radial fractures — a cost analysis study. Injury. 2009;40:1279–81. doi: 10.1016/j.injury.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Wei DH, Raizman NM, Bottino CJ, et al. Unstable distal radius fractures treated with external fixation, a radial column plate, or a volar plate. J Bone Joint Surg Am. 2009;91:1568–77. doi: 10.2106/JBJS.H.00722. [DOI] [PubMed] [Google Scholar]
- 11.Egol K, Walsh M, Tejwani N, et al. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomized, prospective trial. J Bone Joint Surg Br. 2008;90:1214–21. doi: 10.1302/0301-620X.90B9.20521. [DOI] [PubMed] [Google Scholar]
- 12.MacDermid JC, Roth JH, McMurtry R. Predictors of time lost from work following a distal radius fracture. J Occup Rehabil. 2007;17:47–62. doi: 10.1007/s10926-007-9069-0. [DOI] [PubMed] [Google Scholar]