Abstract
Acute pancreatitis complicated by acute myocardial infarction has been reported very rarely. The exact mechanism of the cause of myocardial injury is not known. We report a case of 36 year old male presenting with acute pancreatitis complicated by ST elevation acute myocardial infarction (AMI). The administration of thrombolytic therapy in such patients can have deleterious effects. We report successful performance of primary angioplasty in this complicated patient.
Keywords: Acute pancreatitis, Acute myocardial infarction, Primary angioplasty
1. Introduction
Acute pancreatitis is an inflammatory disease of pancreas clinically characterized by epigastric pain and elevated pancreatic enzymes with multisystem involvement as a complication. The cardiovascular complications include shock, hypovolemia, pericardial effusions and non specific ST segment changes.
We report a case of 36-year-old male who developed an acute anterior wall myocardial infarction as a complication of acute pancreatitis. He underwent emergency coronary angiography and primary angioplasty successfully and survived the complication. To the best of our knowledge this is the first case reported in the medical literature.
2. Case report
A 36-year-old male patient was admitted to hospital with epigastric pain suggestive of pancreatitis,12 h after alcohol ingestion, in the middle of the night. He developed retrosternal chest pain, radiating to left arm (suggestive of ACS), 7 h after the onset of abdominal pain. The patient was treated for pancreatitis 2 months prior to this admission.
At admission, pulse rate was 110/minute and blood pressure was 180/120 mmHg. Physical examination revealed, epigastric tenderness with bilateral basal crepitations. ECG showed (Figs. 1 and 2), ST elevation in leads V1 to V4 and 2DEcho showed regional wall motion abnormality in LAD territory with LV dysfunction. Biochemical investigations showed, serum CKNAC 826U/L, CKMB 50U/L, serum amylase 584 U/L and serum lipase 370 U/L. Ultrasound abdomen and CT scan abdomen (Fig. 3a and b) showed signs of acute pancreatitis.
Fig. 1.
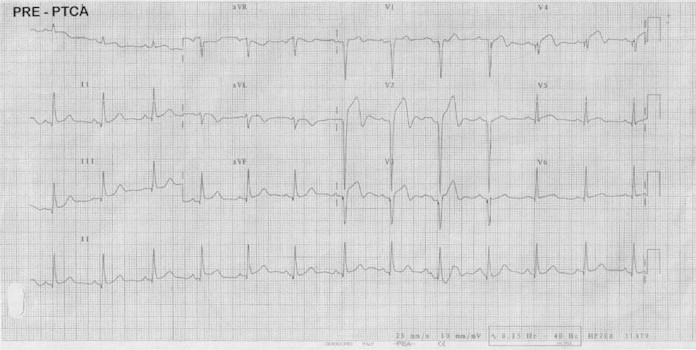
ECG showing acute anterior MI.
Fig. 2.
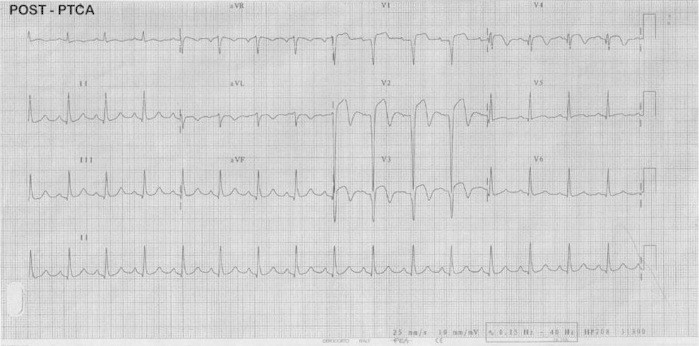
ECG immediately after PTCA.
Fig. 3.
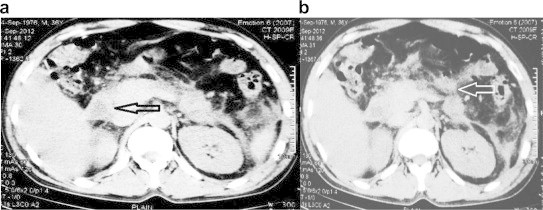
a and b: CT scan of the abdomen showing evidence of acute pancreatitis.
Coronary angiography showed, total occlusion of mid LAD (Fig. 4a) with left circumflex and right coronary arteries being normal. Patient had persistent chest pain not relieved by nitroglycerine. He received Inj pethidine for analgesia. As the patient continued to have chest pain, primary angioplasty with stenting was contemplated with heparin alone. This patient received 600 mg of Clopidogrel with Disprin 350 mg loading dose, to be followed by Clopidogrel 75 mg and enteric coated Aspirin 325 mg per day. The lesion was crossed with 0.014″ × 180 cm guidewire and Bare metal stent (BMS) of 3.5 × 24 mm was implanted in the mid LAD (Fig. 4b). The coronary flow was TIMI grade II after implantation. He did not receive any GPIIb/IIIa inhibitors. Post stenting, he received intracoronary nicorandil, nitroglycerine to improve flow, followed by continuous intravenous administration. The patient had prompt relief of the chest discomfort after PTCA and did not have any recurrence. Post PTCA, patient had hematemesis following vomiting and did not receive any heparin subsequent to PTCA. Pancreatitis was managed with IV fluids and empirical antibiotics. The pancreatitis pain subsided within 48 h. The paralytic ileus improved within 72 h, and he was discharged after 6 days.
Fig. 4.
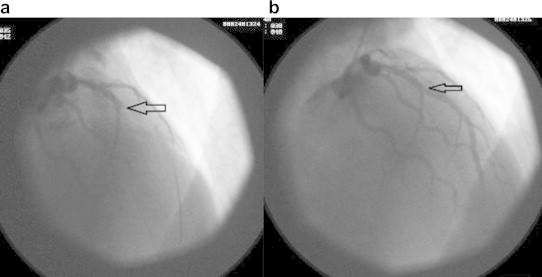
a: Angiogram showing total occlusion of LAD. b: Angiogram showing fully opened up LAD.
3. Discussion
Systemic complications of acute pancreatitis involve pulmonary, cardiovascular and nervous system. ST elevation in acute pancreatitis is a rare phenomenon, but other electrocardiographic changes are relatively common, including arrhythmia, conduction abnormalities and changes in the T wave and QT period.1 Several hypotheses have been proposed to explain these ST changes. Vagal reflexes commonly associated with acute pancreatitis can cause cardiac damage by acting directly on the myocardium, indirectly altering coronary blood flow, or through the increased secretion of pancreatic proteolytic enzymes2,3. Electrolytic abnormalities such as hypokalemia, hypocalcemia and hyponatremia are common in acute pancreatitis and can modify the repolarization phase on the ECG, but ST elevation in such cases is rarely seen.
Severe hemodynamic disturbances such as profound hypotension may diminish coronary perfusion and cause ischemia leading to ECG changes, especially in patients with coronary artery disease.
Pancreatic proteolytic enzymes including trypsin may directly damage the membrane of the myocyte with subsequent changes of cell permeability and possible cellular necrosis, as well as secondary electrical disturbance. These enzymes may change platelet adhesiveness and influence the coagulation system, thus leading to coronary thrombosis4,5 Some studies revealed higher frequency of cardiovascular lesions in individuals with acute or chronic pancreatitis without relation to the common cardiovascular risk factors. There is also the possibility of exacerbation of these lesions during the pancreatic event.6 Although angiographic or morphologic analysis of patients with ST elevation in pancreatitis revealed normal coronary arteries in a high percentage of cases,7 a cardiovascular investigation is recommended in such cases.
Acute pancreatitis complicated with true myocardial infarction is very rare. In 2005, Korantzo Poulos et al8 reported a case which was claimed to be the third case of MI with pancreatitis. In 2010 Sheng-Hsiung Sheu9 reported a similar case where coronary angiography and elective PTCA was done after the recovery from pancreatitis.
Our patient represents a true case of MI based on changes in the cardiac enzyme levels, ECG, echocardiographic and coronary angiographic findings.
The initial differential diagnosis of pseudo or true myocardial infarction is important because their treatment strategies differ markedly. Erroneously administered thrombolytic agents in pseudo MI cases may result in disastrous outcome. Cafri et al10 reported a 54-year-old male, who underwent thrombolytic therapy after being misdiagnosed with myocardial infarction. Mann et al11 reported a 47-year-old male with alcohol related acute pancreatitis, who died of severe retroperitoneal hematoma apparently related to the thrombolytic therapy. A report by Qazi et al12 showed that immediate thrombolysis in acute pancreatitis when followed by coronary angiography showed 90% stenosis of right coronary artery.
A standard management protocol has not been defined because of paucity of reports of cases of pancreatitis complicated with AMI. Coronary angioplasty is preferable to avoid the potentially lethal consequences of thrombolytic therapy in patients of acute MI. Coronary angiography procedure can be done with minimal or no heparin. Anti thrombotics can be given after identification of the culprit vessel. Thrombus aspiration by a catheter, is a good option as an initial treatment. Plain old balloon angioplasty (POBA) can be done after thrombus suction, if the angiographic result is good, we can avoid stenting and dual antiplatelet therapy. The antiplatelet therapy may give problems, if pancreatitis requires surgical management in near future. The role of intracoronary or systemic administration of GPIIb/IIIa inhibitors during angioplasty in this setting is not known. The slow flow phenomenon after angioplasty may require administration of nitroglycerine, nicorandil, nitroprusside.
Conflicts of interest
All authors have none to declare.
References
- 1.Faintuch J.J., Abrahao M.M., Glacaglia L.R. Electrocardiographic changes in pancreatitis. Arq Bras Cardiol. 1989;52:259–260. [Ill] [PubMed] [Google Scholar]
- 2.Manning G.W., Hall G.E., Banting E. Vagus stimulation and the production of myocardial damage. Camad MAJ. 1937;37:314–318. [PMC free article] [PubMed] [Google Scholar]
- 3.Morrison L.M., Swulim W.A. Role of the gastrointestinal tract in production of cardiac symptoms. Experimental and clinical observation. J Am Med Assoc. 1940;114:217. [Google Scholar]
- 4.Lieberman J.S., Taylor A., Wright I.S. The effect of intravenous trypsin administration on the electrocardiogram of the rabbit. Circulation. 1954;10:338–342. doi: 10.1161/01.cir.10.3.338. [DOI] [PubMed] [Google Scholar]
- 5.Kellner A., Robertston T. Selective necrosis of cardiac and skeletal muscle induced experimentally by means of proteolytic enzymes solution given intravenously. J Exp Med. 1954;99:387–404. doi: 10.1084/jem.99.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gulio L., Stella A., Labo G. Cardiovascular lesions in chronic pancreatitis. Dig Dis Sci. 1982;27:716–722. doi: 10.1007/BF01393767. [DOI] [PubMed] [Google Scholar]
- 7.Spritzer H.W., Peterson C.R., Jones C.R. Electrocardiographic abnormalities in acute pancreatitis: two patients studied by selective coronary arteriography. Milit Med. 1969;134:687–693. [PubMed] [Google Scholar]
- 8.Korantzo Poulos P., Pappa E., Dimitroula V. ST segment elevation pattern and myocardial injury induced by acute pancreatitis. Cardiology. 2005;103:128–130. doi: 10.1159/000083438. [DOI] [PubMed] [Google Scholar]
- 9.Hsu Po Chao, Liw Tsung Hsien, Su Ho Ming, Liw Zu Yau, Lai Wew Ter, Sheu Sheng-Hsiung. Acute necrotizing pancreatitis complicated with ST elevation acute myocardial infarction: a case report and literature review. Kaohsiung J Med Sci. 2010;26:200–205. doi: 10.1016/S1607-551X(10)70029-2. [DOI] [PubMed] [Google Scholar]
- 10.Cafri C., Basok A., Katz A. Thrombolytic therapy in acute pancreatitis presenting as acute myocardial infarction. Int J Cardiol. 1995;49:279–281. doi: 10.1016/0167-5273(95)02312-k. [DOI] [PubMed] [Google Scholar]
- 11.Mann G., Heeth D., Candilsh W. Dangers of thrombolysis. BMJ. 1990;300:811. [Google Scholar]
- 12.Qazi Y.A., Sekovski B., Qazi K.J. Is thrombolytic therapy an option in myocardial infarction with acute pancreatitis? Am J Med. 2000;108:178. doi: 10.1016/s0002-9343(99)00325-3. [DOI] [PubMed] [Google Scholar]


