Abstract
Takotsubo cardiomyopathy is a type of non-ischemic cardiomyopathy in which there is sudden temporary left ventricular dysfunction. High-degree AV block and takotsubo cardiomyopathy have been reported together rarely in medical literature. Here we discuss a case of takotsubo cardiomyopathy presenting with complete heart block. A 72-year-old female presented with retrosternal chest pain. Electrocardiogram showed complete heart block without any significant ST-T changes. Echocardiogram revealed regional wall motion abnormality not consistent with coronary artery disease and was suggestive of apical ballooning. Coronary angiogram showed no significant coronary artery lesion. LV angiogram showed apical ballooning and LV systolic dysfunction. Patient underwent temporary pacemaker implantation. Since the complete heart block did not revert even after 18 days, she underwent a permanent pacemaker implantation.
Keywords: Apical ballooning syndrome, Complete heart block, Temporary pacemaker implantation, Permanent pacemaker implantation
1. Introduction
Takotsubo cardiomyopathy (TC), also known as apical ballooning syndrome, stress-induced cardiomyopathy and broken heart syndrome is a type of non-ischemic cardiomyopathy in which there is sudden temporary left ventricular (LV) dysfunction following acute emotional stress or acute medical illness. There are six reported cases of atrioventricular block reported along with stress cardiomyopathy of which one case was documented to have narrow QRS escape, three cases had wide QRS escape rhythm and for two patients the nature escape rhythm is not clear. The exact association between AV block and TC is not clear. We present a case of takotsubo cardiomyopathy with complete heart block presented as acute coronary syndrome.
2. Case report
A 72-year-old female with previous history of acid peptic disease presented with retrosternal chest pain radiating to the left arm and presyncope after an episode of emotional stress. She was comfortable at rest. Clinically there was no evidence of heart failure. Heart rate was 40 /min and regular. Blood pressure was 110/70 mmHg. ECG showed complete heart block (CHB) with a narrow QRS escape rhythm without any significant ST/T changes (Fig. 1). Troponin T was 0.41 ng/ml. Renal parameters, serum electrolytes and thyroid function tests were within normal limits. 2D Echocardiography (ECHO) showed hyper contractile basal segments and akinetic mid, distal segments and apex which was not confined to a coronary artery territory (Fig. 2).
Fig. 1.
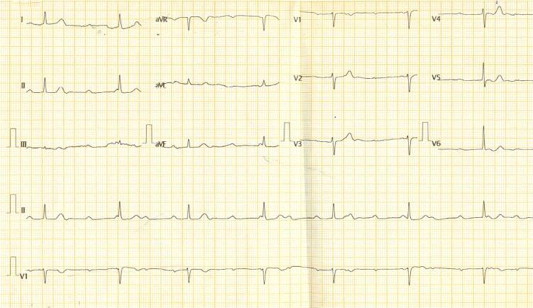
ECG showing complete heart block with narrow QRS escape rhythm.
Fig. 2.
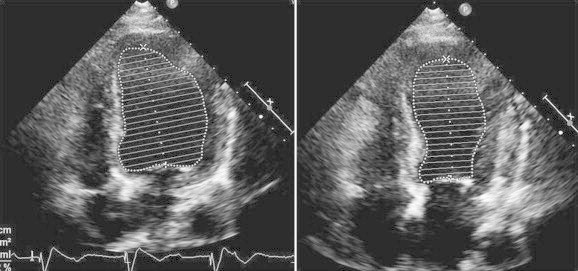
Echocardiographic image of the left ventricle in diastole (left) and in systole (right) shows basal hyper contractility, ballooning mid, distal and apical segments.
Coronary angiogram (CAG) was done in view of history of chest pain and elevated troponin levels did not reveal any hemodynamically significant lesions. LV angiogram showed basal hyper contractility, ballooning mid, distal and apical segments (Fig. 3). Patient also underwent temporary pacemaker implantation (TPI) in view of low ventricular rate. The clinical, ECHO and angiogram pictures were consistent with takotsubo cardiomyopathy.
Fig. 3.

Left ventricular angiogram in diastole (left) and in systole (right): shows basal hyper contractility, ballooning mid, distal and apical segments.
Patient was treated symptomatically with ACE inhibitors and diuretics. During the course of the hospital stay patient had transient prolongation of QT interval which could not be attributed to any dyselectrolytemia. PPI was postponed expecting recovery from CHB. Since there was no recovery even after 18 days, she underwent single chamber permanent pacemaker implantation (VVI). Post procedure ECHO after 24 days of admission showed normal LV function with no RWMA (Fig. 4). At discharge patient was hemodynamically stable and was in paced rhythm with good LV systolic function.
Fig. 4.

Echocardiographic image (after 24 days of admission) of left ventricle in diastole (left) and in systole (right) showing recovery of regional wall motion abnormality.
3. Discussion
Takotsubo cardiomyopathy (TC) is a reversible cardiomyopathy with a clinical presentation indistinguishable from myocardial ischemia. TC is estimated to represent 1%–2% of patients presenting with features suggestive of myocardial infarction.1 It most commonly occurs in postmenopausal women and is frequently precipitated by a stressful event. Chest pain and dyspnea are the typical presenting symptoms. Transient ST-segment elevation on ECG and a small rise in cardiac biomarkers are common. Regional wall motion abnormality which extends beyond the territory of a single epicardial coronary artery in the absence of obstructive coronary lesions is the characteristic finding. Supportive treatment leads to spontaneous rapid recovery in nearly all patients. The prognosis is excellent, and recurrence occurs in <10% of patients.1
Researchers at the Mayo Clinic proposed diagnostic criteria in 2004, which have been modified recently.2 All the following features should be present for the diagnosis of TC: (1) Transient hypokinesis, akinesis or dyskinesis in the left ventricular mid segments with or without apical involvement; regional wall motion abnormalities that extend beyond a single epicardial vascular distribution; and frequently, but not always, a stressful trigger; (2) The absence of obstructive coronary disease or angiographic evidence of acute plaque rupture; (3) New ECG abnormalities (ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin; (4) The absence of pheochromocytoma and myocarditis.
Complete heart block accompanying TC is a very rare presentation. The wall motion abnormality usually that accompanies Takotsubo cardiomyopathy recovers completely. But the AV block might persist inspite of complete clinical recovery.3 It is clearly evident that our patient has had CHB and TC. But it is not clear which of the conditions has triggered the other. Two scenarios might explain this clinical presentation. In the first one, the patient collapsed because of a CHB, and TC appeared because of stress secondary to immobility. In the second scenario, CHB and TC appeared together. Even though a preexisting complete heart block (congenital complete heart block) with new onset left ventricular dysfunction cannot be ruled out, the absence of left ventricular and left atrial dilatation and not noted to have a low heart rate for the past 72 years are in favor of new onset CHB.
There are few case reports in which TC had been reported following a cardiac pacemaker insertion for high-degree AVB, and some authors suggested that emotional distress following a cardiac pacemaker insertion might cause TC.4,5 ECHO and angiographic findings at admission were suggestive of TC prior to pacemaker insertion in our case. Hence, this scenario is probably irrelevant to our patient. In most case reports, high-degree AV Block and TC appeared together.3,6–8 Hence, most authors suggest that diffuse spasms in small branches of the coronary arteries consistent with TC might cause myocardial ischemia and atrioventricular conduction disorder. However, myocardial ischemia in TC is transient, and in most of these cases, high-degree AVB had continued although contractile dysfunction has resolved, necessitating a permanent cardiac pacemaker implantation. It is possible that contrary to the contractile system, the recovery of the cardiac conduction system is prolonged in TC. Indeed, Nault et al have demonstrated in an electrophysiological study non-resolution of a high-degree AV Block 1 year following TC, but eventually resolved 2 years later.9
4. Conclusion
Stress-induced cardiomyopathy remains an interesting but enigmatic entity. Although the apical ballooning syndrome has gained attention during the past few years, alternative presentations of stress cardiomyopathy as in our case are possibly under-recognized. Correctly identifying these patients within the large group of patients presenting as acute coronary syndrome is important for further management.
Financial support
Nil.
Conflicts of interest
All authors have none to declare.
References
- 1.Prasad A., Lerman A., Rihal C.S. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417. doi: 10.1016/j.ahj.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Akashi Yoshihiro J., Goldstein David S., Barbaro Giuseppe, Ueyama Takashi. Takotsubo cardiomyopathy – a new form of acute, reversible heart failure. Circulation. 2008;118:2754–2762. doi: 10.1161/CIRCULATIONAHA.108.767012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kodama S., Miyoshi K., Shiga Y. Takotsubo cardiomyopathy complicated by high-grade atrioventricular block: a report of two cases. Exp Clin Cardiol. 2009;14:e35–e38. [PMC free article] [PubMed] [Google Scholar]
- 4.Abu Sham'a R.A., Asher E., Luria D. Apical ballooning syndrome: a complication of dual chamber pacemaker implantation. Indian Pacing Electrophysiol J. 2009;9:229–232. [PMC free article] [PubMed] [Google Scholar]
- 5.Chun S.G., Kwok V., Pang D.K. Transient left ventricular apical ballooning syndrome (takotsubo cardiomyopathy) as a complication of permanent pacemaker implantation. Int J Cardiol. 2007;117:e27–e30. doi: 10.1016/j.ijcard.2006.11.125. [DOI] [PubMed] [Google Scholar]
- 6.Inoue M., Kanaya H., Matsubara T. Complete atrioventricular block associated with takotsubo cardiomyopathy. Circ J. 2009;73:589–592. doi: 10.1253/circj.cj-08-0219. [DOI] [PubMed] [Google Scholar]
- 7.Lee W.L., Miao L.F., Chan H.W. Takotsubo syndrome with transient complete atrioventricular block. Chin Med J. 2006;119:73–76. [PubMed] [Google Scholar]
- 8.Nef H.M., Möllmann H., Sperzel J. Temporary third-degree atrioventricular block in a case of apical ballooning syndrome. Int J Cardiol. 2006;113:e33–e35. doi: 10.1016/j.ijcard.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Nault M.A., Baranchuk A., Simpson C.S. Takotsubo cardiomyopathy: a novel “proarrhythmic” disease. Anadolu Kardiyol Derg. 2007;(suppl 1):101–103. [PubMed] [Google Scholar]


