Abstract
Gunshot wound (GSW) to the spine which was earlier common in the military population is now being increasingly noted in civilians due to easy availability of firearms of low velocity either licensed or illegal combined with an increased rate of violence in the society. Contributing to 13% to 17% of all spinal injuries, the management of complex injury to the spine produced by a GSW remains controversial. Surgery for spinal cord injuries resulting from low velocity GSWs is reserved for patients with progressive neurologic deterioration, persistent cerebrospinal fluid fistulae, and sometimes for incomplete spinal cord injuries. Surgery may also be indicated to relieve active neural compression from a bullet, bone, intervertebral disk, or a hematoma within the spinal canal. Spinal instability rarely results from a civilian GSW. Cauda equina injuries from low velocity GSWs have a better overall outcome after surgery. In general, the decision to perform surgery should be made on consideration of multiple patient factors that can vary over a period of time. Although there have been plenty of individual case reports regarding GSW to the spine, a thorough review of unique mechanical and biological factors that affect the final outcome has been lacking. We review the key concepts of pathogenesis and management of GSW to the spine and propose an algorithm to guide decision making in such cases.
Keywords: Gunshot spine, Gunshot wound spine, Bullet injury spine
Introduction
The incidence of firearm injury in the civilian population has remarkably increased in recent years, and among these, gunshot wound (GSW) to the spine is particularly devastating because the ideal management of GSW spine remains a matter of controversy. Various studies have been published in favour of conservative management, indicating surgical interventions do not have much effect on outcome. However, most of these studies are based on military populations in whom GSW is much more different from civilian GSW due to the difference in weapons. A proper concept of GSW spine pathophysiology, types, prognostic factors and management strategies should be in minds of neurosurgeons when dealing with such types of cases. Here we will try to develop a clear vision regarding the management of GSW spine by reviewing the literature to elucidate the key concepts regarding the pathogenesis of neuronal injury in GSW spine.
Epidemiology
GSW to the spine was once common only in the military population but is now increasingly prevalent in civilians in due to easy availability of firearms of low velocity that are either licensed or illegal. Contributing to 13% to 17% of all spinal injuries [1], GSW spine is the third most common cause of spine injuries after fall from height and road traffic accident [2].
Factors Unique to GSW
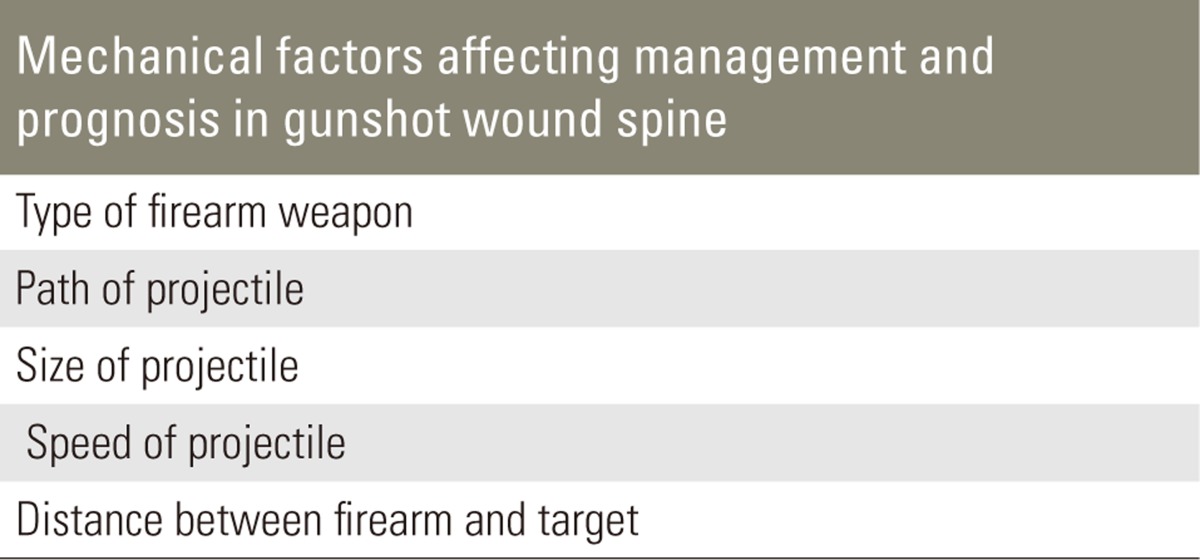
Although many features of GSW spine are similar to other forms of spinal injury, several unique features of GSW set it apart in terms of management and decision making. The factors involved can broadly be classified as mechanical and biological.
1. Mechanical factors
Mechanical factors determining the severity of GSW spine are related to the ballistics of the projectile which causes injury and can be enumerated as in Table 1.
Table 1.
Mechanical factors affecting management and prognosis in gunshot wound spine
Ballistics is defined as the scientific study of projectile motion and is divided into three categories: internal, external, and terminal ballistics. Internal ballistics is concerned with the projectile within the firearm. External ballistics is concerned with the projectile in the air. Terminal ballistics is concerned with what happens when the projectile hits its target. Wound ballistics is a subset of terminal ballistics, and is the most important aspect of ballistics that physicians need to understand [3-5].
1) Types of firearm weapons
First of all, we must know the types of firearms used, as it determines the severity and pattern of damage. There is a major difference between military and civilian population GSW spines as firearms used in these two population groups are categorized according to energy and velocity [6]. The type of projectile also varies with the type of firearm varying from multiple pellets of a shotgun to a single bullet from a rifle.
2) Speed of projectile
(1) Low energy/velocity weapons
Muzzle velocity is less than 1,000 to 2,000 ft/sec (305.4 to 609.6 m/sec).
Examples are pistols and handguns which has calibre 6.35 mm, 722-787 ft/sec velocity, 50 grains in weight and a carry energy of 85 J.
These firearms mainly cause direct injury (bullet nucleus, broken metallic or bone particles and disc material) as there is no hydrodynamic strike effect (blast wave or cavitation wave) on target.
(2) High energy/velocity weapons
Velocity more than 2,000 to 3,000 ft/sec (609.6 to 914.4 m/sec).
Examples are military assault rifles, M-6, Remington bullets and AK-47 with bullet weight 123 grains (8 g) having velocity 2,362 ft/sec and energy 2,074 J. These carry so much energy that they cause both direct and indirect injuries (injury distant to projectile trajectory) due to shock wave or the cavitation wave effect.
3) Path of projectile
Path of the bullet is also a determining factor of the severity of injury and zone of destruction. In general, the longer the terminal ballistics, the more severe the injury. Yaw refers to tumbling of the bullet along its long axis, indicating that a long bullet produces an increased yaw and a larger zone of destruction [7].
4) Size of projectile
The size of the projectile also matters in the amount of kinetic energy and momentum that it is carrying and in the degree of tissue loss it can produce at the target site.
5) Distance between firearm and target
If a shot is fired close to the target, then gun powder residue can give an accurate determination of the distance between the firearm and the target. A contact shot to the target produces tearing, a large amount of burning, and unburned gun powder particles deposited in the bullet tract. A near contact shot will cause burning around the bullet hole and a tight pattern of unburned gun powder particles. As the firearm moves farther away from the target, there will be little to no burning around the bullet hole, and the pattern of unburned gun powder particles will generally get wider. As the firearm is moved even farther away from the target, no unburned gun powder will be seen around the bullet hole.
2. Biological factors
Biological factors are related to the degree of actual damage produced in spinal cord tissues, which affect prognosis and management plan are enumerated in Table 2.
Table 2.
Biological factors affecting management and prognosis in gunshot wound spine
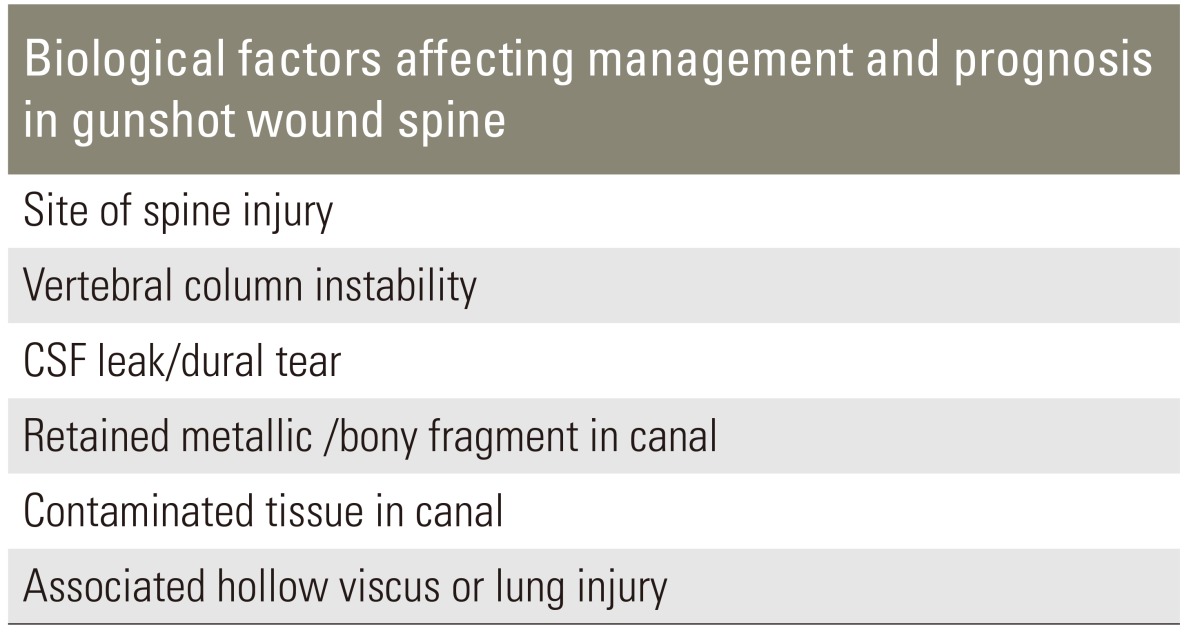
CSF, cerebrospinal fluid.
1) Site of injury
The most common site is the thoracic spine (66%), followed by lumbar spine (17%) and cervical spine1 (6%) [8]. The thoracic canal/thoracic cord ratio is less than that of the lumbar and cervical region, so a retained projectile is more devastating at thoracic region than at other levels of spine [9]. Retained canal fragments if located below the T12 level have a risk of migration [10-12]. The consequences of gunshot entry into the upper cervical spine in addition to being frequently disastrous can also include vertebral artery injury and even death due to airway dysfunction [13-16].
2) Vertebral column instability
Firearm injuries in the spinal zone are generally biomechanically stable [5]. If a bullet in the lumbar zone breaks the pedicle or facet while traversing, it can cause an acute or chronic instability [6]. If the pedicle or facet is intact, no spinal instability is observed. The thoracic vertebrae have a stable biomechanical structure maintained by means of costo-vertebral joints and the thoracic cage. However, the cervical and lumbar spine are more prone to biomechanical instability.
3) Cerebrospinal fluid (CSF) leak/dural tear
Dural leak and the impending risk of meningitis are some of the important biological factors that determine the prognosis and indications for surgery.
4) Retained metallic/bony fragment in canal
Retained intra-spinal bullets can present with delayed neurological findings secondary to reactive changes around the bullet. After a gunshot injury, spinal cord defect occurs as a result of direct damage by the bullet nucleus or metallic particles or as a result of compression by the broken bone particles. Although less commonly observed, disc material can cause neural defects by compressing the canal when the bullet nucleus damages the annulus [17]. This results in an increase in the pressure of the nucleus pulposus after the bullet nucleus settles at an inter-vertebral locus. The possibility of long-term copper and lead toxicity due to a retained metallic foreign body can become an indication for surgery [18-20].
5) Contaminated tissue in canal
Acute infective complications of GSW spine due to contamination are empyema, spinal abscess, intra-abdominal sepsis, psoas muscle abscess, subcutaneous abscess and bullet tract infection [21]. Arachnoiditis, a pain syndromein the lower extremities, and reappearance of neurological deficits are chronic complications seen in GSW spine.
6) Associated hollow viscus and lung injury
Septic complications are most common in the lumbar spine followed by the thoracic and cervical spines [22]. The incidence of septic complications in lumbar spine injuries is highest because bullets often pass through the gastrointestinal tract [23]. Such contaminated bullets increase the risk of osteomyelitis in the associated spinal lesions. Romanick et al. [24], in a study of 20 patients, urged early removal of the bullet to prevent septic complications, particularly if the abdomen had been penetrated. In contrast, Yashon et al. [25] failed to detect an increased incidence of septic complications when reviewing 65 patients with retained missile fragments in the spinal cord. These findings were supported by Stauffer et al. [26]. Similar results were reported by Waters et al. [27] and by Kihtir et al. [28]. Venger et al. [29] stated that despite potential contamination from a perforated bronchus or hollow viscus, neurosurgical intervention to remove bullet fragments led to a higher complication rate than that of patients with retained bullets.
Management
The initial management of a patient with a GSW must include the following standard trauma protocols, with the maintenance of airway, breathing, and circulation taking precedence. Evaluation should be guided by the area of injury. After the patient is stabilized, the spinal injury should be thoroughly evaluated. Important history may include information about the type of weapon used, number of shots fired, and proximity of shot(s). This information provides important clues regarding the extent of injury and will guide in making treatment decisions. Physical examination is equally important in assessing gunshot patients. A complete neurologic examination must be performed to document motor function, reflexes, and sensation at the time of injury. Periodic examination is needed to assess any deterioration in neurologic function, because it may affect treatment decisions. A rectal examination should also be performed. Tetanus prophylaxis is required, especially if immunization status is unknown. Moreover, broad-spectrum antibiotics should be started immediately, regardless of injury location and the results of wound culture which has limited utility in this setting [20,30]. Given the lack of efficacy, steroids should not be included in the treatment regimen for patients with GSW spine [20,31]. Entrance and exit wounds should be inspected and radio-opaque markers should be placed over all wounds to help identify the gunshot path in radiographic studies. At first, 2 orthogonal plain radiographic views of the spine must be obtained to locate the fragments of the bullet and to detect fractures. This should be followed by computed tomography (CT), which is the study of choice, as it allows for more precise localization of bullet fragments within the spinal canal or vertebral segments [20].
If instability is suspected, flexion and extension radiographs or CT follow-up is needed. The use of magnetic resonance imaging in assessing GSWs to the spine is debated upon because of the potential for bullet fragments to migrate and cause additional neural injury. Numerous investigators have demonstrated that MRI can be used safely in the appropriate clinical context [20]. CT myelogram is a good option to use in diagnosing CSF leak trajectory.
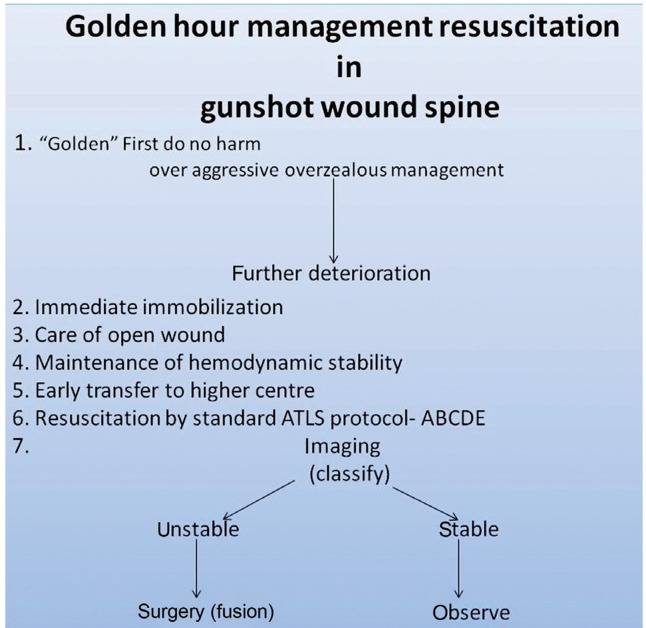
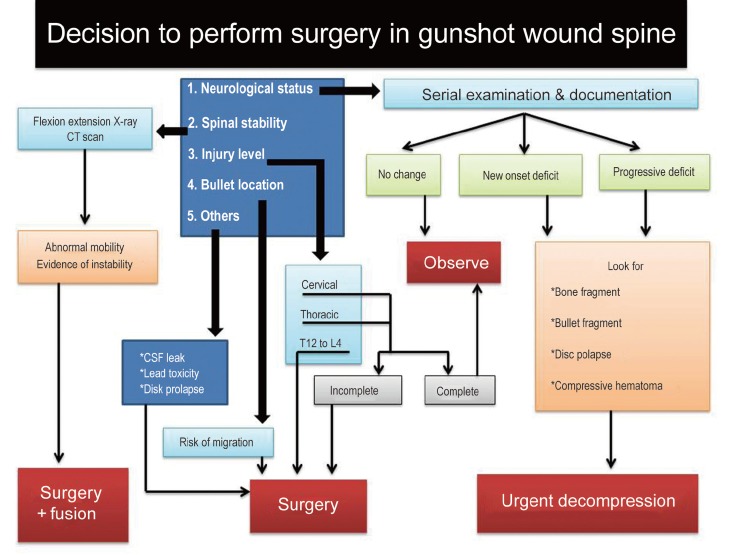
Moreover, early versus delayed surgery or no surgical treatment at all may not significantly affect the overall rate of complications or the length of hospital stay. However, the decision to perform surgery depends on 4 main variables: neurologic status, spinal stability, bullet location, and injury level along with some others. Algorithm for deciding to perform surgery in GSW spine after primary resuscitation was attempted, as shown in Figs. 1, 2.
Fig. 1.
Golden hour management resuscitation in gunshot wound spine. ATLS, advanced trauma life support.
Fig. 2.
Algorithm for decision to perform surgery in gunshot wound spine. CT, computed tomography; CSF, cerebrospinal fluid.
Conclusions
A GSW to the spine is a complex injury, and its treatment remains controversial. Treatment depends on the neurosurgeon's understanding of the mechanism of injury, various prognostic mechanical and biological factors, principle of management, diagnostic imaging, and surgical options. Decompression and removal of intracanal bullets at T12 and below may improve motor function. In select cases of cervical injuries, removal of intracanal bullet fragments may be justified, particularly with incomplete lesions. Regardless of injury level, new-onset or progressive neurologic deterioration is an indication for urgent decompression. Intrathecal migratory missiles represent a very rare subset of GSWs to the spine, and their treatment should be individualized. There is a continued need for well studied protocols that are specific to spinal GSWs to simplify treatment decisions and further improve the standard of care.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Farmer JC, Vaccaro AR, Balderston RA, Albert TJ, Cotler J. The changing nature of admissions to a spinal cord injury center: violence on the rise. J Spinal Disord. 1998;11:400–403. [PubMed] [Google Scholar]
- 2.Miller CA. Penetrating wounds of the spine. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. Vol. 2. San Francisco: McGraw-Hill Book Co.; 1985. pp. 1746–1748. [Google Scholar]
- 3.DeMuth WE., Jr Bullet velocity as applied to military rifle wounding capacity. J Trauma. 1969;9:27–38. doi: 10.1097/00005373-196901000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Robertson DP, Simpson RK, Narayan RK. Lumbar disc herniation from a gunshot wound to the spine: a report of two cases. Spine (Phila Pa 1976) 1991;16:994–995. doi: 10.1097/00007632-199108000-00026. [DOI] [PubMed] [Google Scholar]
- 5.Meyer PR, Apple DF, Bohlman HH, Ferguson RL, Stauffer ES. Symposium: management of fractures of the thoracolumbar spine. Contemp Orthop. 1988;16:57–86. [Google Scholar]
- 6.Yoshida GM, Garland D, Waters RL. Gunshot wounds to the spine. Orthop Clin North Am. 1995;26:109–116. [PubMed] [Google Scholar]
- 7.Waters RL, Sie IH. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;(408):120–125. doi: 10.1097/00003086-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Heiden JS, Weiss MH, Rosenberg AW, Kurze T, Apuzzo ML. Penetrating gunshot wounds of the cervical spine in civilians: review of 38 cases. J Neurosurg. 1975;42:575–579. doi: 10.3171/jns.1975.42.5.0575. [DOI] [PubMed] [Google Scholar]
- 9.Koizumi M, Ueda Y, Iida J, et al. Upper thoracic spinal cord injury without vertebral bony lesion: a report of two cases. Spine (Phila Pa 1976) 2002;27:E467–E470. doi: 10.1097/00007632-200211010-00020. [DOI] [PubMed] [Google Scholar]
- 10.Kafadar AM, Kemerdere R, Isler C, Hanci M. Intradural migration of a bullet following spinal gunshot injury. Spinal Cord. 2006;44:326–329. doi: 10.1038/sj.sc.3101808. [DOI] [PubMed] [Google Scholar]
- 11.Gupta S, Senger RL. Wandering intraspinal bullet. Br J Neurosurg. 1999;13:606–607. doi: 10.1080/02688699943169. [DOI] [PubMed] [Google Scholar]
- 12.Oktem IS, Selcuklu A, Kurtsoy A, Kavuncu IA, Pasaoglu A. Migration of bullet in the spinal canal: a case report. Surg Neurol. 1995;44:548–550. doi: 10.1016/0090-3019(95)00212-x. [DOI] [PubMed] [Google Scholar]
- 13.Hopla DM, Mazur JM, Bass RM. Cervical vertebrae subluxation. Laryngoscope. 1983;93:1155–1159. doi: 10.1288/00005537-198309000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Kahraman S, Gonul E, Kayali H, et al. Retrospective analysis of spinal missile injuries. Neurosurg Rev. 2004;27:42–45. doi: 10.1007/s10143-003-0274-9. [DOI] [PubMed] [Google Scholar]
- 15.Medzon R, Rothenhaus T, Bono CM, Grindlinger G, Rathlev NK. Stability of cervical spine fractures after gunshot wounds to the head and neck. Spine (Phila Pa 1976) 2005;30:2274–2279. [PubMed] [Google Scholar]
- 16.Kupcha PC, An HS, Cotler JM. Gunshot wounds to the cervical spine. Spine (Phila Pa 1976) 1990;15:1058–1063. doi: 10.1097/00007632-199015100-00014. [DOI] [PubMed] [Google Scholar]
- 17.Mirovsky Y, Shalmon E, Blankstein A, Halperin N. Complete paraplegia following gunshot injury without direct trauma to the cord. Spine (Phila Pa 1976) 2005;30:2436–2438. doi: 10.1097/01.brs.0000184588.54710.61. [DOI] [PubMed] [Google Scholar]
- 18.Linden MA, Manton WI, Stewart RM, Thal ER, Feit H. Lead poisoning from retained bullets. Pathogenesis, diagnosis, and management. Ann Surg. 1982;195:305–313. doi: 10.1097/00000658-198203000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tindel NL, Marcillo AE, Tay BK, Bunge RP, Eismont FJ. The effect of surgically implanted bullet fragments on the spinal cord in a rabbit model. J Bone Joint Surg Am. 2001;83:884–890. doi: 10.2106/00004623-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Bono CM, Heary RF. Gunshot wounds to the spine. Spine J. 2004;4:230–240. doi: 10.1016/S1529-9430(03)00178-5. [DOI] [PubMed] [Google Scholar]
- 21.Benzel EC, Hadden TA, Coleman JE. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20:281–285. doi: 10.1227/00006123-198702000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Velmahos G, Demetriades D. Gunshot wounds of the spine: should retained bullets be removed to prevent infection? Ann R Coll Surg Engl. 1994;76:85–87. [PMC free article] [PubMed] [Google Scholar]
- 23.Miller BR, Schiller WR. Pyogenic vertebral osteomyelitis after transcolonic gunshot wound. Mil Med. 1989;154:64–66. [PubMed] [Google Scholar]
- 24.Romanick PC, Smith TK, Kopaniky DR, Oldfield D. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am. 1985;67:1195–1201. [PubMed] [Google Scholar]
- 25.Yashon D, Jane JA, White RJ. Prognosis and management of spinal cord and cauda equina bullet injuries in sixty-five civilians. J Neurosurg. 1970;32:163–170. doi: 10.3171/jns.1970.32.2.0163. [DOI] [PubMed] [Google Scholar]
- 26.Stauffer ES, Wood RW, Kelly EG. Gunshot wounds of the spine: the effects of laminectomy. J Bone Joint Surg Am. 1979;61:389–392. [PubMed] [Google Scholar]
- 27.Waters RL, Adkins RH, Yakura J, Sie I. Profiles of spinal cord injury and recovery after gunshot injury. Clin Orthop Relat Res. 1991;(267):14–21. [PubMed] [Google Scholar]
- 28.Kihtir T, Ivatury RR, Simon R, Stahl WM. Management of transperitoneal gunshot wounds of the spine. J Trauma. 1991;31:1579–1583. doi: 10.1097/00005373-199112000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Venger BH, Simpson RK, Narayan RK. Neurosurgical intervention in penetrating spinal trauma with associated visceral injury. J Neurosurg. 1989;70:514–518. doi: 10.3171/jns.1989.70.4.0514. [DOI] [PubMed] [Google Scholar]
- 30.Gustilo RB. Current concepts in the management of open fractures. Instr Course Lect. 1987;36:359–366. [PubMed] [Google Scholar]
- 31.Heary RF, Vaccaro AR, Mesa JJ, et al. Steroids and gunshot wounds to the spine. Neurosurgery. 1997;41:576–583. doi: 10.1097/00006123-199709000-00013. [DOI] [PubMed] [Google Scholar]