Abstract
PURPOSE
The purpose of this study was to compare the effect of a diode laser and traditional irrigants on the bond strength of self-adhesive cement.
MATERIALS AND METHODS
Fifty-five incisors extracted due to periodontal problems were used. All teeth were instrumented using a set of rotary root canal instruments. The post spaces were enlarged for a No.14 (diameter, 1.4 mm) Snowlight (Abrasive technology, OH, USA) glass fiber reinforced composite post with matching drill. The teeth were randomly divided into 5 experimental groups of 11 teeth each. The post spaces were treated with the followings: Group 1: 5 mL 0.9% physiological saline; Group 2: 5 mL 5.25% sodium hypochlorite; Group 3: 5 mL 17% ethylene diamine tetra acetic acid (EDTA), Group 4: 37% orthophosphoric acid and Group 5: Photodynamic diode laser irradiation for 1 minute after application of light-active dye solution. Snowlight posts were luted with self-adhesive resin cement. Each root was sectioned perpendicular to its long axis to create 1 mm thick specimens. The push-out bond strength test method was used to measure bond strength. One tooth from each group was processed for scanning electron microscopic analysis.
RESULTS
Bond strength values were as follow: Group 1 = 4.15 MPa; Group 2 = 3.00 MPa; Group 3 = 4.45 MPa; Group 4 = 6.96 MPa; and Group 5 = 8.93 MPa. These values were analysed using one-way ANOVA and Tukey honestly significant difference test (P<.05). Significantly higher bond strength values were obtained with the diode laser and orthophosphoric acid (P<.05). There were no differences found between the other groups (P>.05).
CONCLUSION
Orthophosphoric acid and EDTA were more effective methods for removing the smear layer than the diode laser. However, the diode laser and orthophosphoric acid were more effective at the cement dentin interface than the EDTA, Therefore, modifying the smear layer may be more effective when a self-adhesive system is used.
Keywords: Bond strength, Diode laser, Fiber post, Smear layer
INTRODUCTION
Fiber-reinforced posts have superior advantages as compared with cast posts, generally regarding their esthetics, physical properties and their modulus of elasticity, which is similar to root dentin.1 Posts are generally cemented with resin cements. Proper selection of resin cements influence the retention of posts and the success of restoration.2,3 The studies indicate that failure of glass fiber-reinforced post-and-core restorations often occurs because of debonding at the post-resin interface and/or resin-dentin interface as a result of bond deficiencies.4,5
Self-adhesive resin cements are the least investigated group among the resin cements. Application steps are reduced by removing the pre-treatment procedures of the dentin.6 The organic matrix consists of newly developed phosphoric acid methacrylate. The adhesive mechanism is based on the chemical reaction between the hydroxyapatite crystals of the tooth and phosphoric acid monomers.7 Self-adhesive cements are also resistant to moisture and able to release fluoride comparable to glass ionomer cements.8 Also, they have satisfactory esthetic and mechanical properties.9 Because of these positive features, they are used for the adhesive cementation of fixed prostheses and posts.
Removing the smear layer that contains gutta-percha remnants, microorganisms, and infectious dentin is necessary for the penetration of the adhesive system and resin cement into the dentin tubules.10,11 Self-adhesive resin cements cannot completely remove the smear layer.12,13 This remaining smear layer could cause a lower bond strength for self-adhesive resin cements as compared with an etch and rinse adhesive system.14
Several chemical substances that are used as irrigants during the biomechanical preparation can remove the smear layer and alter the characteristics of the dentin substrate. Sodium hypochlorite (NaOCl) has the capacity to dissolve organic tissues and neutralize toxic products and also has an antimicrobial action15 whereas ethylene diamine tetra acetic acid (EDTA) chelates calcium ions and promotes dentin demineralization and smear layer removal.16
Sodium hypochlorite, ethylene diamine tetra acetic acid, orthophosphoric acid (H3PO4)10,17 and different laser systems18 are used to increase the micromechanical retention of the cement by removing the smear layer. No study has been conducted on comparing traditional irrigation systems and photodynamic diode laser performance on the bond strength of self-adhesive cements using fiber posts.
Lasers can be used to vaporize tissues, remove and modify the smear layer and eliminate residual tissue in the main canal.19,30 Diode lasers can make alterations on dentin and may increase the bond strength to root canal dentin.20 Alfredo et al.20 found increased bond strength using with 980 nm diode laser and attributed to the alterations caused by the laser on dentin surface, such as fissures and topographic changes. Laser treatment can be a valuable instrument for the removal or modify of the smear layer in root dentin, as a debridement device during post space preparation.
The aim of this study was to compare the effect of the photodynamic diode laser and other smear layer removal methods on bond strength of the self-adhesive cement. The null hypothesis was that no significant differences would be found among push-out bond strength values after different root canal surface treatments.
MATERIALS AND METHODS
In this study, 55 maxillary central incisors, which were extracted due to periodontal problems, were used. Teeth with distinctly oval root canals were not included. The teeth were cleaned of both calculus and soft tissues and stored in physiological saline before proceeding. The crowns of each tooth were removed at the level of the cemento-enamel junction with a high-speed diamond bur (ZR Diamonds, Brasseler GmbH, Lemgo, Germany) under water spray. The working length of each root canal was established 1 mm short of the apical foramen with a size 15 K-type file (Mani Inc., Japan). The canals were prepared with a rotary system (X-Smart, Dentsply, Maillefer, Ballaigues, Switzerland). All teeth were instrumented using a set of rotary instruments (Pro Taper, Dentsply, Switzerland) to the size of F3 (multi tapered #30; finishing file) by the same operator. The canals were irrigated at every change of instrument with 2 mL 5% hypochlorite solution and 5 mL for the final irrigation. The canals were dried with matching paper points. The prepared canals were filled with matching tapered gutta percha points (Dentsply, Maillefer, France) and a resin sealer (AH Plus, Dentsply, Konstanz, Germany). The coronal aspect of the gutta percha was removed with a heated probe (Gutta Cut, VDW GmbH, Munich, Germany).
After storing the teeth in a humid medium for 1 week at 37℃, the post spaces were enlarged for a No. 14 (diameter 1.4 mm) glass fiber reinforced composite post (Snowlight Post, Abrasive technology, OH, USA) with matching drill. Four millimeters of root canal filling were left in the apical aspect. After the post space preparations, the teeth were randomly divided into 5 experimental groups of 11 teeth each.
The post spaces were treated with the following:
Group 1: 5-mL 0.9% physiological saline (NaCl), with a disposable syringe for 1 minute
Group 2: 5-mL 5.25% sodium hypochlorite (NaOCl), with a disposable syringe for 1 minute
Group 3: 5-mL 17% EDTA with a disposable syringe for 1 minute
Group 4: etching with 37% orthophosphoric acid for 30 seconds
Group 5: Photodynamic diode laser (HELBO TheraLite Laser, HELBO Photodynamic Systems GmbH & Co., Germany).
Bacteria-sensitive, light-active dye solution HELBO Endo Blue (phenothiazine-5-ium, 3, 7-bis (dimethylamino)-, chloride) (HELBO Photodynamic Systems GmbH & Co., Germany) photosensitizer was applied for 1 minute into the post spaces and rinsed with water in Group 5. After rinsing in Group 5, post spaces were dried with paper points. A laser probe (HELBO 3D Endo Probe, Helbo Photo-dynamic Systems GmbH & Co., Germany) was placed near the apex and irradiated for 1 minute with HELBO TheraLite Laser with a wavelength of 660 nm, an output power of 75 mW. The laser was delivered through a flexible fiber optic tip curved at an angle of 60°. The fiber design permits a 3-dimensional exposure of the area, emitting light at the tip and from the lateral sides, thus leading to even light distribution both vertically and horizontally.
Size No. 14 (R = 1.4 mm) Snowlight posts were luted with self-adhesive resin cement (Clearfil SA Cement, Kuraray Medical Inc., Japan). Excess cement was removed with a scaler. Specimens were stored in distilled water at 37℃ between phases of the experiment.
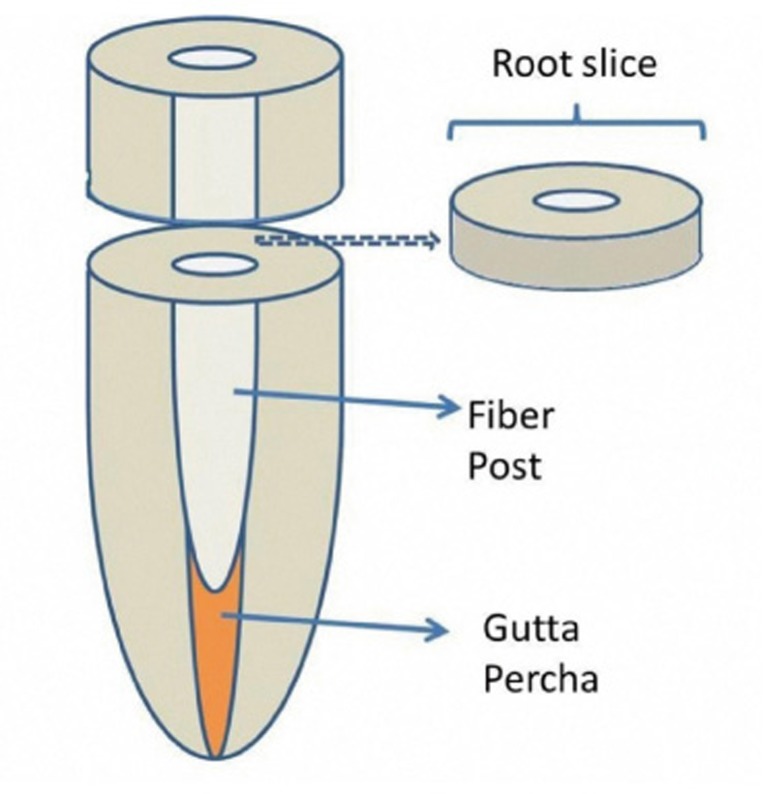
Each root was sectioned perpendicular to its long axis to create 1 mm thick specimens with a 0.3 mm thickness slow-speed diamond saw (Buehler, USA) at the coronal third of the root. One section of the 1 mm thick specimen was prepared from each tooth (Fig. 1). Ten specimens were prepared for each group.
Fig. 1.
Schematic view of the root and dentin disc specimens.
Push-out bond strength was tested using a universal testing machine (AGS-X, Schimadzu Co., Kyoto, Japan) at a crosshead speed of 1 mm/min until post debonding occurred. The specimens were loaded with a 1 mm diameter cylindrical tip in an apical-coronal direction to push-out the post toward the wider part of the root slice to avoid the taper limitation. The cylindrical tip was positioned to touch only the post. The loads at failure were recorded as N and the bond strengths were expressed in MPa; N was divided by the area of the bonded interface, which was calculated using the following formula:
A = 2πrh (where A is the area of the bonded interface, π = 3.14, r is the post radius, and h is the thickness of the specimen in mm).
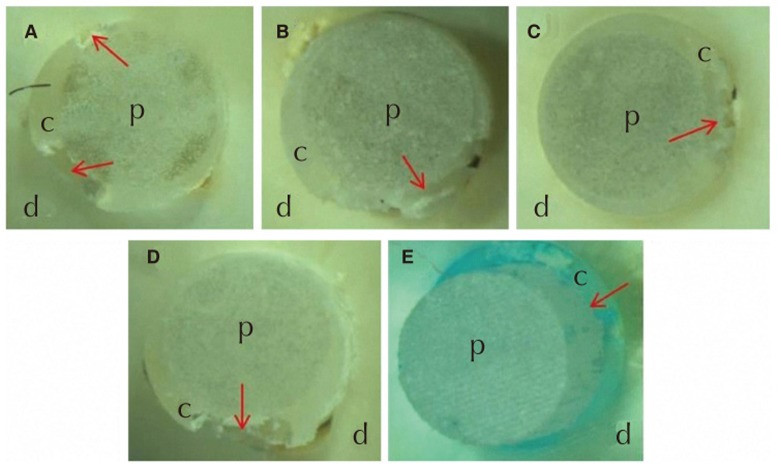
The debonded specimens investigated under the stereomicroscope at original magnification ×40 for the failure interface as between dentin-cement, post-cement and both dentin-cement and post-cement (Fig. 3 and Fig. 4).
Fig. 3.
Cross-sectional image of the debonded dentin discs. (A) Mixed failure (cement debonded both dentin and post) in NaCI group, (B) Mixed failure (cement debonded both dentin and post) in NaOCl group, (C) Mixed failure (cement debonded both dentin and post) in EDTA group, (D) Mixed failure (cement debonded both dentin and post) in orthophosphoric acid group, (E) Post-cement failure (cement debonded only post) in HELBO TheraLite Laser group. c: Cement, d: Dentin, p: Post. Red arrows show the debonding failure (Original magnification, ×40).
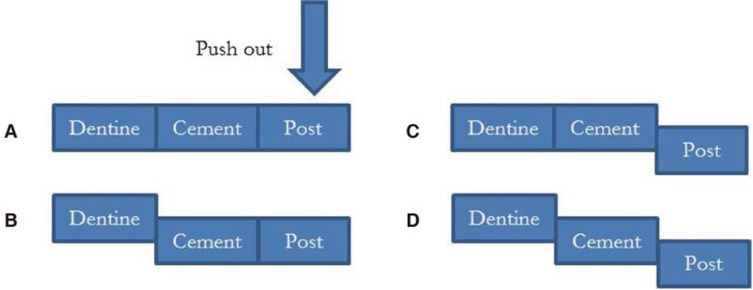
Fig. 4.
Schematic view of the debonded interfaces: (A) before push out, (B) dentin-cement failure, (C) post-cement failure, (D) both dentin-cement and post-cement failure (mixed failure).
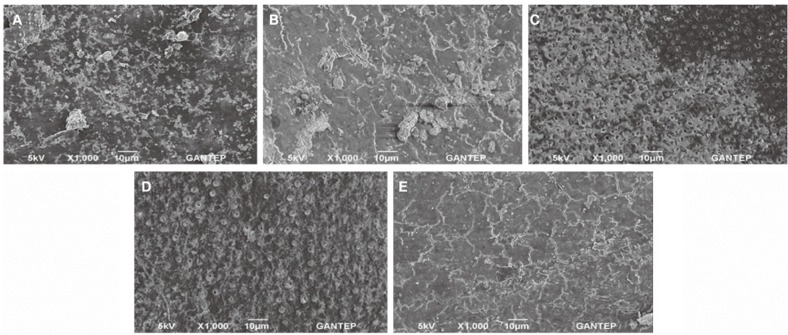
One tooth from each group was processed for SEM analysis to observe the changes on root canal surfaces after the post space treatments. The teeth were split longitudinally in the buccolingual plane. The two halves of the tooth were dehydrated and coated with gold for SEM analysis. The specimens were analyzed in 5 kV and original magnification ×1,000 (Fig. 2).
Fig. 2.
SEM images of the post spaces treated with (A) NaCI (0.9%) shows the smear layer covering root canal dentin surface, (B) NaOCl (5.25%) shows the smear layer covering root canal dentin surface, (C) EDTA (17%) shows the open dentinal tubule and (D) 37% H3PO4 shows the open dentinal tubules and erosion of the tubule orifices (E) HELBO TheraLite Laser shows the smear layer covering the root canal dentin surface (Original magnification, ×1000).
All calculated bond strengths were analyzed using one-way analysis of variance (ANOVA) and Tukey honestly significant differences (HSD) tests with SPSS 16.0 (SPSS, Inc., Chicago, IL, USA) (α=.05).
RESULTS
The mean values and standard deviations of the test groups are presented in Table 1. Bond strength values showed that the higher results were obtained for the HELBO TheraLite Laser and 37% orthophosphoric acid groups. There were no differences between the other groups.
Table 1.
Mean push-out bond strengths of the post surface treatment methods
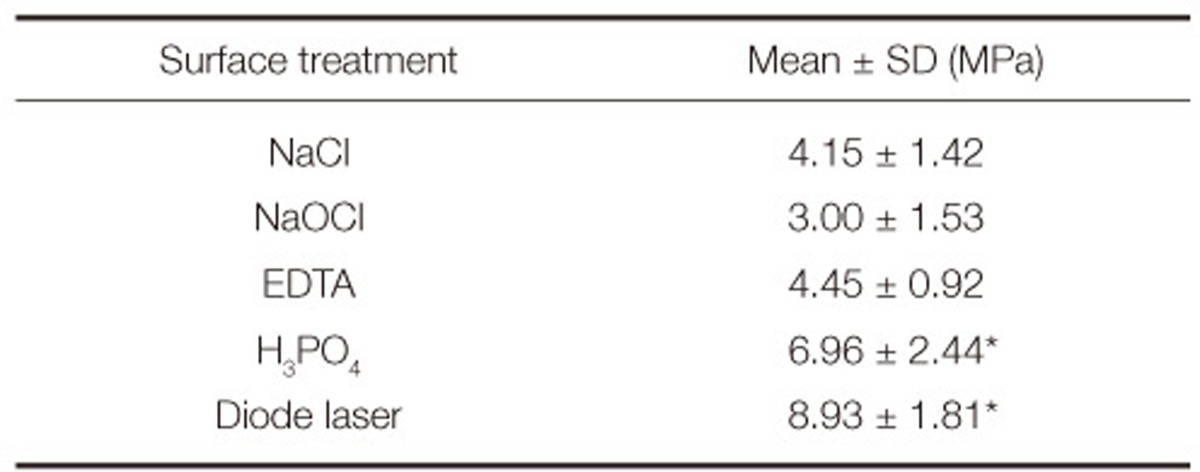
*(P<.05).
Although NaCl, NaOCl, EDTA, and H3PO4 groups showed post-cement and cement-dentin failure both (mixed failure); HELBO TheraLite Laser showed post-cement failure at the cross sectional image of the dentin discs (Fig. 3).
DISCUSSION
The null hypothesis was rejected because the results of this study revealed that different smear layer removal methods from root canal dentin affect the bond strength of a fiber post cemented with adhesive resin to dentin (P<.05).
The smear layer produced by post space preparation should be removed according to some authors owing to the increase of antibacterial effects21,22 and also adhesive effectiveness23 as it becomes porous and the authors insisted that the smear layer causes a weak adherent interface between cement and dentin. On the other hand, other authors insist upon retaining smear layer for adaptation of the materials to root surface.24,25
Interestingly, in photodynamic diode laser group, bond strength was higher than the other groups except H3PO4 group without the removal of smear layer. It may arise from the fact that collagen fibrils structure does not change after lasing. By conserving most of their intrafibrillar mineral, they are more stable and less affected by dehydration, which improves the infiltration of the luting agent.
Sodium hypochlorite increases the penetration of the monomers into the dentinal tubules by removing organic components, and breaks down to sodium chloride and oxygen. This is because broken down oxygen inhibits interfacial polymerization of resin bonding materials.24,26 On the other hand, 5% NaOCl alone did not remove the smear layer as effectively as found in other studies.27,11 Also the residual NaOCl solution affect the change in redox potential of the bonding agent.11 Others have found NaOCl and NaCl could not remove the smear layer, which can act as a diffusion barrier on the dentin and reduce dentin permeability for bonding agents.2,28 Results from another study with 5.25% NaOCl and 0.9% saline did not increase bond strength of luting cement,29 as shown in this study.
EDTA is a popular chelating agent for root canal instrumentation. A study conducted by Takeda et al.30 mentioned that 17% EDTA alone was not effective in removing smear remnants as it did in this study; in the same study, authors used 6% orthophosphoric acid to remove the smear layer, but in contrast to this study, it was not useful. This may be due to difference in the acid concentration. For the recent study, 37% orthophosphoric acid was used. Conforming to this study, other authors showed that 37% orthophosphoric acid improved retention by eliminating dentin mineral content.31
Dual irrigation methods, such as a combination of 17% EDTA and 5.25% NaOCl are effective methods for removing the smear layer,32 but this method results in sporadic erosion and dissolution of the dentin.33,34 Moreover, it was shown that these solutions did not have a good ability in preparing complicated root canals.35-37 Therefore, dual irrigation methods were not used for this study.
When the push-out tests were examined, generally, failures of bonding were observed between resin and dentin.38,39 In the present study, only the diode laser group showed post-cement failure, the other groups showed mixed failures (Fig. 3 and Fig. 4). It was shown that using the photodynamic diode laser in post space increased the bond strength of resin cement to dentin interface, as compared with other surface treatment methods. It is important to improve the bonding effectiveness of the resin and dentin for post restoration success with removal of the smear layer and formation of the resin-dentin interdiffusion zone.2,40 On the contrary, Demiryürek et al.27 used acetone based agent, which could not remove the smear layer and sealer remnants effectively on radicular dentin surfaces, to treat post space treatment and found to be more effective compared with EDTA, citric acid and orthophosphoric acid. It was concluded that removal of the smear layer and opening of dentinal tubules are not recommended when a self-etching/self-priming adhesive system is used.27
Laser devices have been used in root canal treatment since the early 1970s,41 but their acceptance has been very slow. General causes of dissatisfaction have included thermal damage caused by the laser photonic energy.42 Therefore, the photonic energy should be at its lowest possible level to eliminate thermal damage.
It has been reported that as the diode-laser treatment (λ = 810 nm) partially opened dentinal tubules, signs of fusions and temperature increase at the root surfaces were observed.43 On the other hand, a study conducted by Altundasar et al.42 after irradiation with a 980-nm diode laser (GaAlAs) (with 2 times more power) had opposite results and two-fold increase in temperature at the root surface was observed. To avoid the temperature rise, lower irradiation power was used for this study (λ = 660 nm), and it was enough to improve bonding effectiveness at the cement-dentin interface.
CONCLUSION
The results of this study suggest the following:
(1) NaOCl (5.25%) and NaCI (0.9%) were not effective in removing the smear layer when used as a final irrigation.
(2) According to the SEM evaluation, orthophosphoric acid (37%) and EDTA (17%) were more effective methods in removing the smear layer than NaOCl, NaCI irrigants, and HELBO TheraLite Laser. However, HELBO TheraLite Laser and orthophosphoric acid were more effective at cement-dentin interface than EDTA for bond strength of self-adhesive cements. Therefore, it may be more effective to modify the smear layer when a self-adhesive system is used.
Footnotes
This study was supported by Mustafa Kemal University Scientific Research Section.
References
- 1.Qualtrough AJ, Mannocci F. Tooth-colored post systems: a review. Oper Dent. 2003;28:86–91. [PubMed] [Google Scholar]
- 2.Ferrari M, Mannocci F. A 'one-bottle' adhesive system for bonding a fibre post into a root canal: an SEM evaluation of the post-resin interface. Int Endod J. 2000;33:397–400. doi: 10.1046/j.1365-2591.2000.00310.x. [DOI] [PubMed] [Google Scholar]
- 3.Mannocci F, Bertelli E, Watson TF, Ford TP. Resin-dentin interfaces of endodontically-treated restored teeth. Am J Dent. 2003;16:28–32. [PubMed] [Google Scholar]
- 4.Monticelli F, Toledano M, Tay FR, Cury AH, Goracci C, Ferrari M. Post-surface conditioning improves interfacial adhesion in post/core restorations. Dent Mater. 2006;22:602–609. doi: 10.1016/j.dental.2005.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Goracci C, Raffaelli O, Monticelli F, Balleri B, Bertelli E, Ferrari M. The adhesion between prefabricated FRC posts and composite resin cores: microtensile bond strength with and without post-silanization. Dent Mater. 2005;21:437–444. doi: 10.1016/j.dental.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 6.Mumcu E, Erdemir U, Topcu FT. Comparison of micro push-out bond strengths of two fiber posts luted using simplified adhesive approaches. Dent Mater J. 2010;29:286–296. doi: 10.4012/dmj.2009-089. [DOI] [PubMed] [Google Scholar]
- 7.Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T, Lambrechts P, Peumans M. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23:71–80. doi: 10.1016/j.dental.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Gerth HU, Dammaschke T, Züchner H, Schäfer E. Chemical analysis and bonding reaction of RelyX Unicem and Bifix composites-a comparative study. Dent Mater. 2006;22:934–941. doi: 10.1016/j.dental.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Radovic I, Monticelli F, Goracci C, Vulicevic ZR, Ferrari M. Self-adhesive resin cements: a literature review. J Adhes Dent. 2008;10:251–258. [PubMed] [Google Scholar]
- 10.Serafino C, Gallina G, Cumbo E, Ferrari M. Surface debris of canal walls after post space preparation in endodontically treated teeth: a scanning electron microscopic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:381–387. doi: 10.1016/j.tripleo.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Hayashi M, Takahashi Y, Hirai M, Iwami Y, Imazato S, Ebisu S. Effect of endodontic irrigation on bonding of resin cement to radicular dentin. Eur J Oral Sci. 2005;113:70–76. doi: 10.1111/j.1600-0722.2004.00186.x. [DOI] [PubMed] [Google Scholar]
- 12.Bitter K, Paris S, Pfuertner C, Neumann K, Kielbassa AM. Morphological and bond strength evaluation of different resin cements to root dentin. Eur J Oral Sci. 2009;117:326–333. doi: 10.1111/j.1600-0722.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 13.Monticelli F, Ferrari M, Toledano M. Cement system and surface treatment selection for fiber post luting. Med Oral Patol Oral Cir Bucal. 2008;13:E214–E221. [PubMed] [Google Scholar]
- 14.Piwowarczyk A, Bender R, Ottl P, Lauer HC. Long-term bond between dual-polymerizing cementing agents and human hard dental tissue. Dent Mater. 2007;23:211–217. doi: 10.1016/j.dental.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Zehnder M. Root canal irrigants. J Endod. 2006;32:389–398. doi: 10.1016/j.joen.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 16.Hülsmann M, Heckendorff M, Lennon A. Chelating agents in root canal treatment: mode of action and indications for their use. Int Endod J. 2003;36:810–830. doi: 10.1111/j.1365-2591.2003.00754.x. [DOI] [PubMed] [Google Scholar]
- 17.Erdemir A, Ari H, Güngüneş H, Belli S. Effect of medications for root canal treatment on bonding to root canal dentin. J Endod. 2004;30:113–116. doi: 10.1097/00004770-200402000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Pecora JD, Brugnera-Júnior A, Cussioli AL, Zanin F, Silva R. Evaluation of dentin root canal permeability after instrumentation and Er:YAG laser application. Lasers Surg Med. 2000;26:277–281. doi: 10.1002/(sici)1096-9101(2000)26:3<277::aid-lsm5>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 19.Dederich DN, Zakariasen KL, Tulip J. Scanning electron microscopic analysis of canal wall dentin following neodymium-yttrium-aluminum-garnet laser irradiation. J Endod. 1984;10:428–431. doi: 10.1016/S0099-2399(84)80264-2. [DOI] [PubMed] [Google Scholar]
- 20.Alfredo E, Silva SR, Ozório JE, Sousa-Neto MD, Brugnera-Júnior A, Silva-Sousa YT. Bond strength of AH Plus and Epiphany sealers on root dentine irradiated with 980 nm diode laser. Int Endod J. 2008;41:733–740. doi: 10.1111/j.1365-2591.2008.01418.x. [DOI] [PubMed] [Google Scholar]
- 21.Bystrom A, Claesson R, Sundqvist G. The antibacterial effect of camphorated paramonochlorophenol, camphorated phenol and calcium hydroxide in the treatment of infected root canals. Endod Dent Traumatol. 1985;1:170–175. doi: 10.1111/j.1600-9657.1985.tb00652.x. [DOI] [PubMed] [Google Scholar]
- 22.Perez F, Calas P, de Falguerolles A, Maurette A. Migration of a Streptococcus sanguis strain through the root dentinal tubules. J Endod. 1993;19:297–301. doi: 10.1016/s0099-2399(06)80460-7. [DOI] [PubMed] [Google Scholar]
- 23.Kennedy WA, Walker WA, 3rd, Gough RW. Smear layer removal effects on apical leakage. J Endod. 1986;12:21–27. doi: 10.1016/S0099-2399(86)80277-1. [DOI] [PubMed] [Google Scholar]
- 24.Gençoğlu N, Samani S, Günday M. Dentinal wall adaptation of thermoplasticized gutta-percha in the absence or presence of smear layer: a scanning electron microscopic study. J Endod. 1993;19:558–562. doi: 10.1016/S0099-2399(06)81286-0. [DOI] [PubMed] [Google Scholar]
- 25.Gutmann JL. Adaptation of injected thermoplasticized guttapercha in the absence of the dentinal smear layer. Int Endod J. 1993;26:87–92. doi: 10.1111/j.1365-2591.1993.tb00548.x. [DOI] [PubMed] [Google Scholar]
- 26.Ari H, Yaşar E, Belli S. Effects of NaOCl on bond strengths of resin cements to root canal dentin. J Endod. 2003;29:248–251. doi: 10.1097/00004770-200304000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Demiryürek EO, Külünk S, Saraç D, Yüksel G, Bulucu B. Effect of different surface treatments on the push-out bond strength of fiber post to root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e74–e80. doi: 10.1016/j.tripleo.2009.03.047. [DOI] [PubMed] [Google Scholar]
- 28.Kenshima S, Francci C, Reis A, Loguercio AD, Filho LE. Conditioning effect on dentin, resin tags and hybrid layer of different acidity self-etch adhesives applied to thick and thin smear layer. J Dent. 2006;34:775–783. doi: 10.1016/j.jdent.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Mayhew JT, Windchy AM, Goldsmith LJ, Gettleman L. Effect of root canal sealers and irrigation agents on retention of preformed posts luted with a resin cement. J Endod. 2000;26:341–344. doi: 10.1097/00004770-200006000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Takeda FH, Harashima T, Kimura Y, Matsumoto K. A comparative study of the removal of smear layer by three endodontic irrigants and two types of laser. Int Endod J. 1999;32:32–39. doi: 10.1046/j.1365-2591.1999.00182.x. [DOI] [PubMed] [Google Scholar]
- 31.Rosales-Leal JI, Osorio R, Toledano M, Cabrerizo-Vílchez MA, Millstein PL. Influence of eugenol contamination on the wetting of ground and etched dentin. Oper Dent. 2003;28:695–699. [PubMed] [Google Scholar]
- 32.Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod. 2004;30:559–567. doi: 10.1097/01.don.0000129039.59003.9d. [DOI] [PubMed] [Google Scholar]
- 33.Hülsmann M, Peters OA, Dummer PMH. Mechanical preparation of root canals: shaping goals, techniques and means. Endodc Topics. 2005;10:30–76. [Google Scholar]
- 34.Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009;35:791–804. doi: 10.1016/j.joen.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 35.Wu MK, Wesselink PR. A primary observation on the preparation and obturation of oval canals. Int Endod J. 2001;34:137–141. doi: 10.1046/j.1365-2591.2001.00361.x. [DOI] [PubMed] [Google Scholar]
- 36.De-Deus G, Gurgel-Filho ED, Magalhães KM, Coutinho-Filho T. A laboratory analysis of gutta-percha-filled area obtained using Thermafil, System B and lateral condensation. Int Endod J. 2006;39:378–383. doi: 10.1111/j.1365-2591.2006.01082.x. [DOI] [PubMed] [Google Scholar]
- 37.Berutti E, Marini R, Angeretti A. Penetration ability of different irrigants into dentinal tubules. J Endod. 1997;23:725–727. doi: 10.1016/S0099-2399(97)80342-1. [DOI] [PubMed] [Google Scholar]
- 38.Zicari F, Couthino E, De Munck J, Poitevin A, Scotti R, Naert I, van Meerbeek B. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater. 2008;24:967–977. doi: 10.1016/j.dental.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 39.Ferrari M, Cagidiaco MC, Grandini S, De Sanctis M, Goracci C. Post placement affects survival of endodontically treated premolars. J Dent Res. 2007;86:729–734. doi: 10.1177/154405910708600808. [DOI] [PubMed] [Google Scholar]
- 40.Vichi A, Grandini S, Ferrari M. Comparison between two clinical procedures for bonding fiber posts into a root canal: a microscopic investigation. J Endod. 2002;28:355–360. doi: 10.1097/00004770-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Weichman JA, Johnson FM. Laser use in endodontics. A preliminary investigation. Oral Surg Oral Med Oral Pathol. 1971;31:416–420. doi: 10.1016/0030-4220(71)90164-2. [DOI] [PubMed] [Google Scholar]
- 42.Altundasar E, Ozçelik B, Cehreli ZC, Matsumoto K. Ultramorphological and histochemical changes after ER, CR:YSGG laser irradiation and two different irrigation regimes. J Endod. 2006;32:465–468. doi: 10.1016/j.joen.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 43.Esteves-Oliveira M, de Guglielmi CA, Ramalho KM, Arana-Chavez VE, de Eduardo CP. Comparison of dentin root canal permeability and morphology after irradiation with Nd:YAG, Er:YAG, and diode lasers. Lasers Med Sci. 2010;25:755–760. doi: 10.1007/s10103-010-0775-z. [DOI] [PubMed] [Google Scholar]