Abstract
Objective
To determine whether a complex community intervention in rural Zambia improved understanding of maternal health and increased use of maternal health-care services.
Methods
The intervention took place in six rural districts selected by the Zambian Ministry of Health. It involved community discussions on safe pregnancy and delivery led by trained volunteers and the provision of emergency transport. Volunteers worked through existing government-established Safe Motherhood Action Groups. Maternal health indicators at baseline were obtained from women in intervention (n = 1775) and control districts (n = 1630). The intervention’s effect on these indicators was assessed using a quasi-experimental difference-in-difference approach that involved propensity score matching and adjustment for confounders such as education, wealth, parity, age and distance to a health-care facility.
Findings
The difference-in-difference comparison showed the intervention to be associated with significant increases in maternal health indicators: 14–16% in the number of women who knew when to seek antenatal care; 10–15% in the number who knew three obstetric danger signs; 12–19% in those who used emergency transport; 22–24% in deliveries involving a skilled birth attendant; and 16–21% in deliveries in a health-care facility. The volunteer drop-out rate was low. The estimated incremental cost per additional delivery involving a skilled birth attendant was around 54 United States dollars, comparable to that of other demand-side interventions in developing countries.
Conclusion
The community intervention was associated with significant improvements in women’s knowledge of antenatal care and obstetric danger signs, use of emergency transport and deliveries involving skilled birth attendants.
Résumé
Objectif
Déterminer si une intervention communautaire complexe dans les zones rurales de la Zambie a amélioré la compréhension de la santé maternelle et augmenté l'utilisation des services de soins de santé maternelle.
Méthodes
L'intervention a eu lieu dans six districts ruraux choisis par le ministère de la Santé zambien. Cela impliquait des discussions communautaires sur le thème de la grossesse et de l'accouchement sans danger, dirigées par des bénévoles formés, ainsi que la fourniture de transports d'urgence. Les bénévoles ont travaillé par le biais des groupes d'action pour une maternité sans risque existants, créés par le gouvernement. Les indicateurs de santé maternelle de référence ont été obtenus auprès de femmes dans les districts de l'intervention (n = 1 775) et dans les districts témoins (n = 1 630). Les effets de l'intervention sur ces indicateurs ont été évalués à l'aide d'une approche de la différence du deuxième degré quasi expérimentale, qui implique l'appariement et l'ajustement des coefficients de propension, tels que le niveau d'étude, la richesse, la parité, l'âge et la distance pour se rendre à un établissement de soins de santé.
Résultats
La comparaison de la différence du deuxième degré a montré l'intervention à associer aux augmentations significatives des indicateurs de santé maternelle: 14–16% du nombre des femmes qui savaient quand demander des soins prénatals; 10–15% du nombre des femmes qui connaissaient trois signes de dangers obstétricaux; 12–19% du nombre des femmes qui ont utilisé un transport d'urgence; 22–24% des accouchements impliquant un accoucheur qualifié; et 16–21% des accouchements dans un établissement de soins de santé. Le taux d'abandon des bénévoles était faible. Le coût marginal estimé par accouchement supplémentaire impliquant une sage-femme était d'environ 54 dollars, ce qui est comparable aux autres interventions côté demande dans les pays en voie de développement.
Conclusion
L'intervention communautaire était associée à des améliorations significatives des connaissances des femmes sur les soins prénatals et des signes de dangers obstétricaux, l'utilisation des transports d'urgence et les accouchements impliquant des accoucheurs qualifiés.
Resumen
Objetivo
Verificar si una intervención comunitaria compleja en las zonas rurales de Zambia mejoró la comprensión sobre salud materna e incrementó el uso de los servicios de salud maternos.
Métodos
La intervención, dirigida por voluntarios capacitados y la provisión de transporte de emergencia, tuvo lugar en seis distritos rurales seleccionados por el Ministerio de Salud de Zambia y consistió en debates comunitarios sobre un embarazo y parto seguros. Los voluntarios trabajaron a través de grupos de acción para una maternidad sin riesgo existentes establecidos por el gobierno. Los indicadores de salud materna en la base de referencia se obtuvieron de las mujeres de los distritos de intervención (n = 1775) y control (n = 1630). Se evaluó el efecto de la intervención en estos indicadores mediante un enfoque de diferencias en diferencias cuasi-experimental que incluyó un emparejamiento por puntaje de propensión y el ajuste por factores de confusión como la educación, la riqueza, la paridad, la edad y la distancia a un centro de atención de salud.
Resultados
La comparación de diferencias en diferencias mostró que la intervención se asocia a un aumento significativo en los indicadores de salud materna: 14-16 % en el número de mujeres que sabían cuándo debían buscar atención prenatal; 10-15 % en las mujeres que conocían tres señales de peligro obstétricas; 12-19 % en las que utilizaron el transporte de emergencia; 22-24 % en los partos que necesitaron un matrón capacitado, y 16-21 % en los partos en un centro de atención de salud. La tasa de abandono voluntario fue baja. El coste incremental estimado por parto adicional con un matrón capacitado fue de unos 54 dólares de los Estados Unidos, similar al de otras intervenciones relativas a la demanda en los países en desarrollo.
Conclusión
La intervención comunitaria se asocia con mejoras significativas en el conocimiento de las mujeres sobre la atención prenatal y las señales de peligro obstétricas, el uso del transporte de emergencia y los partos con matrones capacitados.
ملخص
الغرض
تحديد ما إذا كان التدخل المجتمعي المعقد في المناطق الريفية في زامبيا قد أسفر عن تحسين فهم صحة الأمومة وزيادة استخدام خدمات رعاية صحة الأمومة.
الطريقة
تم إجراء التدخل في ست مناطق ريفية اختارتها وزارة الصحة الزامبية. واشتمل على نقاشات مجتمعية حول الحمل المأمون والولادة ترأسها متطوعون مدربون وتوفير النقل في حالات الطوارئ. وعمل المتطوعون من خلال فرق عمل الأمومة المأمونة الحالية التي أنشأتها الحكومة. وتم الحصول على مؤشرات صحة الأمومة عند القيمة القاعدية من النساء لدى التدخل ( العدد = 1775) والمناطق الضابطة ( العدد = 1630). وتم تقييم أثر التدخل على هذه المؤشرات باستخدام نهج الفرق في الاختلاف شبه التجريبي الذي اشتمل على مطابقة نتيجة الميل وتعديل المحددات كالتعليم والثروة والتكافؤ والسن والمسافة إلى مرفق الرعاية الصحية.
النتائج
أظهرت مقارنة الفرق في الاختلاف ارتباط التدخل بزيادات كبيرة في مؤشرات صحة الأمومة: من 14 إلى 16 % في عدد النساء اللاتي عرفن أوقات طلب الحصول على خدمات الرعاية السابقة للولادة؛ ومن 10 إلى 15 % في عدد اللاتي عرفن ثلاث علامات من علامات الخطر ذات الصلة بالولادة؛ ومن 12 إلى 19 % في اللاتي استخدمن النقل في حالات الطوارئ؛ ومن 22 إلى 24 % في الولادات التي اشتملت على قابلة ماهرة؛ ومن 16 إلى 21 % في الولادات التي أجريت في مرفق الرعاية الصحية. وانخفض معدل تسرب المتطوعين. وكانت التكلفة التكميلية لكل ولادة إضافية اشتملت على قابلة ماهرة وفق التقديرات حوالي 54 دولاراً أمريكياً، مقارنة بتلك الخاصة بغيرها من تدخلات جانب الطلب في البلدان النامية.
الاستنتاج
كان التدخل المجتمعي مرتبطاً بتحسينات كبيرة في معرفة النساء بخدمات الرعاية السابقة للولادة وعلامات الخطر ذات الصلة بالولادة واستخدام النقل في حالات الطوارئ والولادات التي تشتمل على قابلات ماهرات.
摘要
目的
确定在赞比亚农村实施的一项综合的社区干预措施是否改善对孕产妇健康的理解并增加对孕产妇保健服务的使用。
方法
在赞比亚卫生部选择的六个农村地区实施干预措施。其中涉及由经过培训志愿者引导的安全怀孕和分娩社区讨论,还涉及提供急救转运。志愿者通过现有由政府建立的母亲安全行动组工作。从干预(n = 1775)和对照区域(n = 1630)的女性获取基线孕产妇健康指标。采用准实验倍差的方法评估干预对这些指标的影响,方法涉及针对教育、财富、平价、年龄以及与医疗设施距离等混杂因素的倾向评分匹配和调整。
结果
倍差比较显示干预与孕产妇健康指标显著增加具有相关性:14-16%的女性知道何时寻求产前护理;10-15%的女性知道三种产科危险信号;12-19%的女性使用了急救转运;22-24%的分娩有熟练接生员参与;16-21%的分娩在健康医疗设施中进行。志愿者退出率比较低。每次使用熟练接生员的额外分娩的估计增量成本约为54 美元,与发展中国家其他需求方面的干预措施的成本相当。
结论
社区干预与妇女产前保健和产科危险信号知识、使用急救转运和使用熟练接生员的分娩等状况显著改善具有相关性。
Резюме
Цель
Определить, помогло ли проведение комплексных мероприятий в местных сообществах сельских регионов Замбии улучшить понимание в вопросах охраны здоровья матерей и более активному использованию услуг здравоохранения для матерей.
Методы
Мероприятия проводились в шести сельских регионах, выбранных Министерством здравоохранения Замбии. В программу мероприятий входили обсуждения с представителями сообщества вопросов о безопасной беременности и родах, проводимые подготовленными волонтерами, а также предоставление автомобилей скорой медицинской помощи. Волонтеры осуществляли свою деятельность путем взаимодействия с организованными правительством Инициативными группами по обеспечению безопасного материнства. Исходные показатели охраны здоровья матерей были получены от участвующих в мероприятиях женщин (n = 1775), а также из контрольных регионов (n = 1630). Влияние мероприятий на эти показатели оценивалось с помощью квазиэкспериментального подхода с оценкой разницы в различиях, что включало в себя непараметрический метод отбора подобного по коэффициенту склонности и внесение поправок для факторов, влияющих на результаты, таких как образование, благосостояние, размер потомства, возраст и расстояние до учреждения здравоохранения.
Результаты
Сравнение методом оценки разницы в различиях показало, что проведенные мероприятия значительно улучшили показатели охраны здоровья матерей: на 14–16% увеличилось количество женщин, которые знали, где можно пройти дородовое наблюдение; на 10–15% увеличилось количество людей, знающих три индикатора опасности при родовспоможении; на12–19% увеличилось количество тех, кто воспользовался автомобилями скорой помощи; на 22–24% увеличилось количество родов с участием опытного акушера; и на 16–21% увеличилось количество родов, принятых в учреждениях здравоохранения. Процент отсеявшихся волонтеров был достаточно низким. Расчетное увеличение расходов на роды с участием опытного акушера составило около 54 долларов США, что сравнимо с другими мероприятиями, проводимыми в развивающихся странах по стимулированию спроса на услуги здравоохранения.
Вывод
Проведение мероприятий среди местных сообществ привело к значительному повышению уровня знаний женщин о дородовом наблюдении и индикаторах опасности при родовспоможении, как и уровня использования автомобилей скорой помощи и проведения родов с участием опытных акушеров.
Introduction
In Zambia, as in other low-income countries, maternal health indicators have remained stubbornly resistant to improvement: for example, the presence of skilled birth attendants at deliveries has hardly increased in the past 20 years and the maternal mortality ratio remains over 500 deaths per 100 000 live births.1 Two contributing factors have been consistently identified: (i) a lack of knowledge about when to access health-care services, which leads to delays in care seeking; and (ii) difficulties with transportation, which lead to delays in reaching health-care facilities.2–4 The problem of stagnating maternal health indicators has probably been exacerbated by a counter-urbanization trend, with people moving to more remote areas.5 Although most of the rural population of Zambia lives less than 8 km from a health centre, the average distance to a health-care facility equipped for safe delivery is more than 15 km.2 The 2007 Demographic and Health Survey (DHS) in the country reported that 57% of women in rural areas regarded distance as a barrier to accessing health care when sick.1
In 2003, Safe Motherhood Action Groups were established in Zambia as part of a national safe motherhood programme. Initially, they were supported by the United Nations Population Fund in North-West Province before being adopted by the Government of Zambia in a national programme. Each group serves a cluster of villages and is encouraged to meet regularly in a communal area. The aim was to mobilize communities to improve the health of women, men and children and reduce the number of human immunodeficiency virus infections. However, a lack of central coordination has meant that communities often found it difficult to know how to use these groups and, as a result, many of these remain dormant.
Our intervention involved revitalizing Safe Motherhood Action Groups to raise awareness of the need to prepare for pregnancy complications and delivery. The main aim was to improve both understanding of maternal health and access to maternal health-care services. Our approach was predicated on the assumption that women require not only knowledge about when they should seek skilled help but also their husbands’ approval for care seeking, which can be encouraged by community leaders. There is growing evidence that better utilization of maternal health-care services depends on mobilizing the entire community.6,7 For example, in a programme for improving birth preparedness in Nepal that focused only on women, knowledge of obstetric danger signs increased but there was little change in the proportion of deliveries involving a skilled birth attendant.8 It was suggested that the lack of progress occurred because education was provided only for women and not for the whole community and because other barriers to health care, such as the cost of getting to a facility, persisted. Our intervention involved the whole community.
Methods
We adopted a quasi-experimental approach to evaluating the effect of a complex community-based intervention that was devised to reduce barriers to the use of maternal health-care services and to increase deliveries involving a skilled birth attendant. The intervention was novel because it involved the whole community and emphasized social approval and its ability to bring about changes in behaviour. The involvement of men, older women and community leaders is vital in places where behaviour is dependent on their approval. In our intervention, men were encouraged to become emergency transport drivers, community leaders were invited to train as community volunteers and older women, who are often traditional birth attendants, were encouraged to become mother’s helpers and were trained to recognize obstetric danger signs. This reduced the likelihood that older women would pressure younger women to conform to dangerous practices.
The intervention involved improving the effectiveness of Safe Motherhood Action Groups by training volunteers and developing and strengthening systems in the community that help women get to heath-care facilities, such as existing arrangements for emergency transport. In practice, training was cascaded across communities: core trainers trained lead volunteers at district health offices and lead volunteers, in turn, trained volunteers within each community. Since the literacy level of volunteers and communities was poor, we adopted a largely paper-free approach to training volunteers and to communicating with communities. Each trained volunteer coordinated a cycle of four community discussions on safe pregnancy and delivery, with additional discussions on neonatal care. Both women and men were encouraged to participate. In addition, communities were encouraged to develop plans for helping women access maternal health services, which included ensuring that transport was accessible and that people (i.e. “mother’s helpers”) were available to assist with child-minding or to accompany women to health-care facilities. Communities were also asked to think about other actions that could be taken to ensure that pregnant women were taken to a health centre in an emergency (e.g. the introduction of a local “law”), to consider social issues that could have a bearing on maternal health, such as violence against women, and to ensure that women without family or other support were included in any initiatives. Although there was some investment in equipment and supplies at health-care facilities in the intervention areas, most was provided towards the end of the intervention period and was unlikely to have had a substantial impact on the use of maternal health-care services.
The intervention was also intended to reduce the delay many women experience in reaching health-care facilities. The distances involved and the poor road conditions mean that, for rural communities, travel is often slow and may be dangerous. Moreover, emergency transport to hospitals is seldom available at health centres. As part of the intervention, community transport, appropriate to the terrain, was provided for groups of two or three villages. In most cases, bicycle ambulances were provided but, in areas where the terrain was particularly uneven or sandy, communities were given ox or donkey carts. One community, which is situated next to a river, was provided with a boat. In addition, health centres were provided with motorcycle ambulances. Each community identified a group of volunteers who were willing to operate and maintain the vehicles and some basic training was provided through the intervention. Follow-up reviews revealed that, in most cases, the vehicles had been well maintained by the communities and that additional vehicle operators were being recruited and trained. Information on the use of emergency transport during the intervention period was obtained by asking women if they had used community transport or transport provided by a health-care facility to reach a health-care facility or hospital for delivery. Additional information on transport was available through a community monitoring system, which was established as part of the intervention to report on women’s use of emergency transport and of health services, such as antenatal care.
The intervention was implemented in six districts selected by the Zambian Ministry of Health largely because they were not already receiving substantive assistance from donors to improve maternal health. Three districts – Serenje, Mongu and Choma – took part in phase one, which started in July 2011, and three – Chama, Kaoma and Mkushi – took part in phase two, which started in January 2012. As a result of the experience gained in phase one, implementation of the intervention – the procurement of vehicles, for example – was slightly quicker in phase two. Otherwise the interventions were identical. Two catchment areas were selected for the intervention in Serenje, Mongu, Choma and Chama, three were selected for Kaoma and one was selected for Mkushi. Each district had a basic emergency obstetric care centre to which smaller health centres or posts were most likely to refer patients. The intervention covered about 25% of the population of each district and included a total of 250 000 inhabitants. In addition, data were collected in five control districts with similar maternal health indicators to monitor changes over time. Any spill-over effects of the intervention were minimized by ensuring that control districts were not adjacent to intervention districts.
A baseline survey of recent births was conducted between December 2010 and May 2011 in both intervention and control districts to assess: (i) current use of maternal and neonatal health-care services; (ii) knowledge of maternal care, including when antenatal care should first be received, and of obstetric danger signs; and (iii) use of community systems that help women obtain care, such as savings schemes and emergency transport (Table 1). A list of all births in the three months before the survey in each area was made using information provided by Safe Motherhood Action Groups. The sample size of women who had recently given birth was 3405 at baseline: 1775 in intervention districts and 1630 in control districts. In the final survey, which was carried out in October 2012, the sample size was 2788: 1445 in intervention districts and 1343 in control districts.
Table 1. Maternal health indicators in intervention and control districts before and after the intervention, 2010–2011, Zambia.
| Indicator | Control districts |
Intervention districts |
|||
|---|---|---|---|---|---|
| Baseline survey (n = 1630) | Final survey (n = 1343) | Baseline survey (n = 1775) | Final survey (n = 1445) | ||
| No. (%) of women who used emergency transport | 21 (1.3) | 20 (1.5) | 12 (0.7) | 215 (14.9) | |
| No. (%) of women who knew three obstetric danger signs | 761 (46.7) | 588 (43.8) | 959 (54.0) | 883 (61.1) | |
| No. (%) of women who knew they should receive antenatal care in the first trimester | 924 (56.7) | 851 (63.4) | 847 (47.7) | 1046 (72.4) | |
| No. (%) of women who received 4 or more antenatal care visits from a skilled birth attendant, with the first in the first trimester | 587 (36.0) | 577 (43.0) | 579 (32.6) | 650 (45.0) | |
| No. (%) of deliveries involving a skilled birth attendant | 660 (40.5) | 618 (46.0) | 731 (41.2) | 984 (68.1) | |
| No. (%) of deliveries involving a skilled birth attendant at a health-care facility | 618 (37.9) | 596 (44.4) | 706 (39.8) | 946 (65.5) | |
| No. (%) of women who received postnatal care within 6 days | 618 (37.9) | 646 (48.1) | 604 (34.0) | 670 (46.4) | |
| No. (%) of women who used modern contraception immediately after giving birth | 453 (27.8) | 424 (31.6) | 364 (20.5) | 449 (31.1) | |
For any intervention for improving maternal health care, it is important to know whether it is sustainable, scalable and cost effective. Although a full cost-effectiveness analysis was outside the scope of this study, we examined some of the costs involved. The main start-up costs were for training volunteers and providing vehicles. We assumed that 20% of volunteers would drop out of the programme each year. The main recurrent costs were for maintenance of vehicles and transportation. As a summary measure, we used the incremental cost per additional delivery involving a skilled birth attendant.
Ethical approval for the study was obtained from the University of Zambia Biomedical Research Ethics Committee. All study participants were provided with, or had read out to them, an informed consent form approved by the ethics committee. The form provided information on the study, on how data would be used and on the participant’s right to withdraw at any time.
The indicators used to assess the effect of the intervention on maternal health care were, before delivery, knowledge that antenatal care should first be received in the first trimester, receipt of antenatal care, knowledge of obstetric danger signs (i.e. fever, discharge, blood loss, severe headache and retained placenta) and use of emergency transport and, subsequently, delivery involving a skilled birth attendant, delivery at a health-care facility, receipt of postnatal care within 6 days and use of modern contraceptives after giving birth. Changes in these indicators due to the intervention were assessed using a difference-in-difference approach that involved a proxy counterfactual drawn from households in control districts. This approach controls for confounding factors and for any general changes that would have occurred over time in the absence of the intervention.
The basic equation used in the difference-in-difference approach was:
where Y is the binary response variable (e.g. delivery at a health-care facility or knowledge of three obstetric danger signs), T is a time variable (baseline = 0, final survey = 1), I is the intervention variable (intervention district = 1, control district = 0), X is a vector of covariates, including education (i.e. highest level achieved), household wealth, the woman’s age and parity and the distance of the woman’s home from the health centre. The impact of the intervention is expressed by the parameter β3, β1 is a measure of the general change in the response variable between baseline and final surveys, β2 represents the general difference in the response variable between intervention and control areas, β0 is a constant, γ is a vector representing the impact of covariates and e is an error term.
Since the accuracy of the difference-in-difference approach is greater if time trends in the control and intervention groups are similar and the time trends are more likely to be similar if the characteristics of the individuals in the groups are broadly similar, we used propensity score matching to match individuals in intervention districts with similar individuals in control districts. Individuals without a close match were excluded from the analysis. Three types of propensity score matching were used: (i) nearest-neighbour matching, which provides a one-to-one match between an observation in the intervention group and the nearest observation in the control group; (ii) calliper matching, which matches observations within a defined distance (i.e. the difference in propensity score between an observation in the intervention group and the nearest observation in the control group); and (iii) radius matching, which takes a weighted average of all observations within a defined distance. Matching reduced the average difference between control and intervention areas to below 10% for most key characteristics. The remaining differences were controlled for by including the relevant characteristics in the difference-in-difference specification.
Results
For both phases of the intervention, significant increases were observed between baseline and final surveys in the proportion of women who (i) knew they should receive antenatal care in the first trimester, (ii) knew three or more obstetric danger signs and (iii) used emergency transport (Table 2). Data from the community monitoring system confirmed the magnitude of the increase in the use of emergency transport.
Table 2. Percentage point change in selected maternal health indicators associated with the intervention, by intervention phase, 2011–2012, Zambia.
| Indicator | No. of women (%) |
Change (percentage points) | Pa | Change reported by community monitoring system (percentage points) | |
|---|---|---|---|---|---|
| Baseline survey | Final survey | ||||
| Districts in phase 1 | |||||
| All women | 1140 (100) | 927 (100) | NA | NA | NA |
| Women who knew they should receive antenatal care in the first trimester | 584 (51.2) | 684 (73.8) | 22.6 | < 0.01 | ND |
| Women with adequate knowledge of obstetric danger signsb | 637 (55.9) | 567 (61.2) | 5.3 | < 0.01 | ND |
| Women who used emergency transportc | 8 (0.7) | 149 (16.1) | 15.4 | < 0.01 | 15.7 |
| Districts in phase 2 | |||||
| All women | 635 (100) | 518 (100) | NA | NA | NA |
| Women who knew they should receive antenatal care in the first trimester | 263 (41.4) | 363 (70.1) | 28.7 | < 0.01 | ND |
| Women with adequate knowledge of obstetric danger signsb | 322 (50.7) | 316 (61) | 10.3 | < 0.01 | ND |
| Women who used emergency transportc | 4 (0.6) | 66 (12.7) | 12.1 | < 0.01 | 14.7 |
NA, not applicable; ND, not determined.
a P-values were calculated using the Welch t test.
b Adequate knowledge was defined as being able to recall three or more obstetric danger signs.
c Use of emergency transport in the community or at a health-care facility when the woman last gave birth.
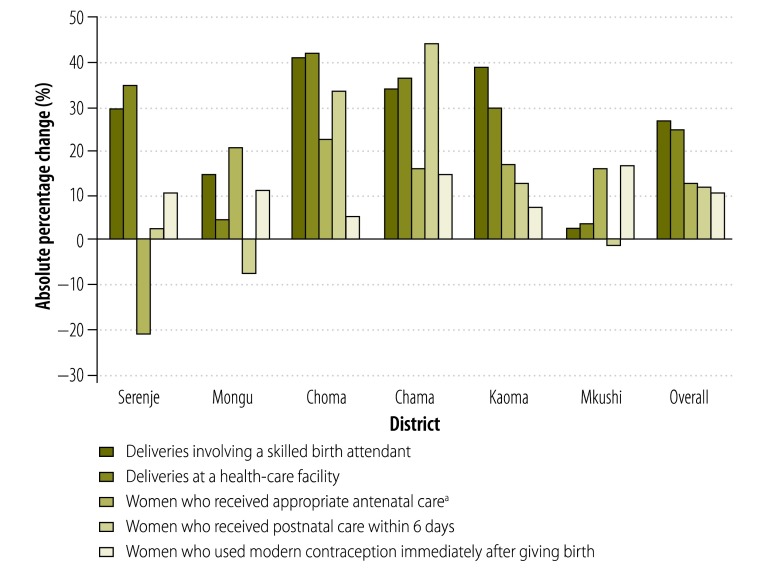
The final survey showed that 75% of deliveries took place at a health-care facility after the intervention compared with 49% before. In general, there were improvements in all six intervention districts in the proportion of deliveries that involved a skilled birth attendant and that took place at a health-care facility and in the proportion of women who received appropriate antenatal and postnatal care and who used modern contraception after giving birth (Fig. 1). In particular, the proportion of deliveries involving a skilled birth attendant increased in all districts; only the increase in Mkushi was not significant. Although improvements were generally observed in all other indicators, the proportion of women who received four or more antenatal care visits decreased in Serenje and the proportion who received postnatal care within 6 days of delivery decreased in Mongu and Mkushi. We believe that the decrease in postnatal care may have been an artefact of the data collection process because respondents often rounded up the time when they received care to the nearest week. Hence, care that was actually received within 6 days was recorded as occurring outside this period.
Fig. 1.
Absolute percentage change in selected maternal health indicators associated with the intervention (difference between baseline and final surveys), by district, 2011–2012, Zambia
a Appropriate antenatal care was defined as the receipt of antenatal care four or more times, with the first time in the first trimester.
The difference-in-difference approach, both with and without propensity score matching, showed that the intervention was associated with a greater increase in maternal health indicators in intervention districts than control districts (Table 3). Depending on the type of matching applied, the proportion of women who used emergency transport increased by between 12.4 and 18.7%; the proportion who knew that antenatal care should be provided in the first trimester increased by between 14.5 and 15.7%; and the proportion who knew three obstetric danger signs increased by between 10.3 and 14.9%. In addition, the proportion of deliveries that involved a skilled birth attendant at a health-care facility increased by between 16.4 and 21.0% and the proportion that involved a skilled birth attendant outside a health-care facility increased by between 9.0 and 16.7%. The increase in the proportion of women who received four or more antenatal care visits and in those who received postnatal care within 6 days was not significantly different from the increase observed in control districts. Data from the community monitoring system, which provided information to the end of 2012, 2 months after the final survey, indicated that just over 70% of women received postnatal care during 2012.
Table 3. Change in maternal health indicators associated with the intervention, by analytical approach, 2011–2012, Zambia.
| Indicator | Unadjusted |
Adjusted for covariates |
Propensity score matching |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Calliper |
Radius |
Nearest neighbour |
||||||||||||
| Difference-in-difference estimatea | tb | Difference-in-difference estimatea | tb | Difference-in-difference estimatea | tb | Difference-in-difference estimatea | tb | Difference-in-difference estimatea | tb | |||||
| Women who used emergency transport | 14.0 | 14.26* | 14.6 | 14* | 12.4 | 2.81* | 13.1 | 2.75* | 18.7 | 3.47* | ||||
| Women who knew three obstetric danger signs | 10.1 | 3.85* | 10.5 | 3.79* | 14.2 | 4.25* | 14.9 | 4.44* | 10.3 | 3.79* | ||||
| Women who knew they should receive antenatal care in the first trimester | 18.1 | 7.14* | 16.6 | 6.18* | 15.5 | 4.97* | 14.5 | 4.43* | 15.7 | 6.54* | ||||
| Women who received four or more antenatal care visits from a skilled birth attendant, with the first in the first trimester | 5.5 | 2.08* | 4.7 | 1.70 | 5.0 | 1.52 | 6.1 | 1.68 | 4.0 | 1.4 | ||||
| All deliveries involving a skilled birth attendant | 21.4 | 8.32* | 18.4 | 6.8* | 24.0 | 7.51* | 22.0 | 6.48* | 22.0 | 8.56* | ||||
| Deliveries involving a skilled birth attendant at a health-care facility | 19.3 | 6.02* | 16.3 | 6.02* | 21.0 | 6.23* | 18.7 | 5.2* | 16.4 | 5.9* | ||||
| Women who received postnatal care within 6 days | 2.3 | 0.88 | 0.6 | 0.23 | 2.5 | 0.75 | 5.3 | 1.50 | 0.2 | 0.08 | ||||
| Women who used modern contraception immediately after giving birth | 6.8 | 2.57* | 7.1 | 2.55* | 4.0 | 1.29 | 6.0 | 1.66 | 6.0 | 2.09* | ||||
* P < 0.05.
a The difference-in-difference estimate is a measure of the difference between the change from before to after treatment in intervention districts and the change from before to after treatment in control districts. It is given in percentage points.
b The t-statistic is the ratio of the change in percentage to the standard error.
The start-up cost of training volunteers was 408 United States dollars (US$) per neighbourhood committee, each of which covered four Safe Motherhood Action Groups on average; training was provided for the lead volunteer, regular volunteers and follow-up support. The start-up costs for vehicles were annualized according to their assumed useful life (Table 4). We found that around 5% of volunteers dropped out of the programme each year, rather than the 20% anticipated. Recurrent costs included the cost of maintenance, which was a proportion of the start-up cost (Table 4), and the cost of the fuel or animal feed used while transporting women to a health centre or hospital. Also included was the cost of a project staff member with a social development or nursing background who was assigned to each district to manage the programme and organize training in partnership with members of the District Health Management Team. The estimated annual cost of running the programme in the six districts, including annualized capital and recurrent costs, was US$ 115 489, which is equivalent to US$ 0.46 per capita or US$ 15 per delivery involving a skilled birth attendant. Our analysis indicates that the intervention was responsible for an increase of 20% in deliveries involving a skilled birth attendant, which corresponds to an increase of 1694 deliveries. Consequently, the incremental cost per additional delivery involving a skilled birth attendant was US$ 68. If the intervention were implemented in all areas of the six districts, the total cost would be US$ 386 389, the per capita cost would be US$ 0.37, the cost per delivery would be US$ 12 and the incremental cost per delivery would be US$ 54.
Table 4. Cost of emergency transportation to a health centre or hospital, 2011–2012, Zambia.
| Vehicle | Start-up cost (US$)a | Useful life (years) | Annual maintenance cost (% of start-up cost) | Cost per trip (US$)a,b |
|---|---|---|---|---|
| Bicycle | 710 | 6 | 10 | 0 |
| Ox cart | 2088 | 12 | 10 | 13 |
| Donkey and cart | 1453 | 12 | 20 | 13 |
| Boat | 1679 | 12 | 10 | 0 |
| Motorcycle | 6327 | 6 | 20 | 24 |
US$, United States dollar.
a Costs were recorded in pounds sterling (£) and converted at a rate of £1 to US$ 1.52.
b The cost per trip is the average cost of the fuel or animal feed needed for each return trip of a woman from the community to a health centre or hospital. No fuel was consumed by the boat or bicycle.
Discussion
The intervention was associated with significant improvements in women’s knowledge of when they should receive antenatal care and of obstetric dangers signs, in the use of emergency transport, in deliveries involving a skilled birth attendant and in the use of modern contraception. However, the increase in the proportion of women who received four or more antenatal care visits and in those who received postnatal care within 6 days was not significant, which may have resulted from women or interviewers rounding up the time when they received care to the nearest week.
Since we used a quasi-experimental approach to evaluate changes in a relatively small total population of 250 000, the findings are necessarily weaker than if randomization had been used. Moreover, the intervention was complex and incorporated several activities in the community. Consequently, it was not possible to separate out the effect of individual components, particularly since an underlying principle of the intervention was that community members themselves should decide on the details of its implementation. Increasing the use of maternal health-care services probably depends on a combination of better community knowledge, the development of strategies to prepare for birth and the provision of emergency transport.
We found that the incremental cost per additional delivery involving a skilled birth attendant would be US$ 54 if the intervention were implemented throughout the six districts studied. This cost is comparable to that of other demand-side interventions in developing countries. For example, in a maternal incentive scheme in Nepal, the estimated cost of each additional delivery at a health-care facility was around US$ 110 and the cost of a voucher scheme in Bangladesh was US$ 70 per delivery.9,10
Since our intervention was largely dependent on community volunteers, retention was a key issue. We did not offer material incentives to volunteers apart from small items such as T-shirts (for identification), pens and exercise books. Vastly different volunteer drop-out rates have been reported by other programmes: one study in urban Bangladesh had a drop-out rate of 90% in the year after training, whereas a programme developed for rural areas in Uganda had a rate of only 14% after 18 months.11,12 Early indications are that the drop-out rate in our intervention areas in Zambia was low, at around 5%. Moreover, an analysis conducted towards the end of the 18-month implementation period found rates ranging from 1 to 12% (mean: 5.4%) in the six districts.13 Two factors that may be important for retaining volunteers are the time that has to be devoted to the work each week (for our intervention, the average was 3 hours) and a strong belief in the value of the programme, which would ensure a high level of intrinsic motivation.
Steps are now underway to absorb the intervention into a government programme. The function of the project staff members who managed the programme and organized training will be taken over by district offices, which are now in the process of scaling up the intervention. It is encouraging that implementation took less time in districts that participated in the second phase of the intervention. Although there remain concerns about the loss of volunteers, it is expected that volunteers will be phased out over time once social approval for the behavioural changes promoted by the intervention is established. It will be interesting to see how this affects sustainability. Future evaluations should monitor whether change becomes self-perpetuating and, if so, how long volunteers need to be active for this to occur.
Funding:
This study was funded by aid from the Government of the United Kingdom of Great Britain and Northern Ireland.
Competing interests:
None declared.
References
- 1.Central Statistical Office, Ministry of Health, Zambia, Tropical Diseases Research Centre, University of Zambia and Macro International Inc. Zambia Demographic and Health Survey 2007. Lusaka & Calverton: Central Statistical Office of Zambia & Macro International Inc; 2009.
- 2.Gabrysch S, Cousens S, Cox J, Campbell OM. The influence of distance and level of care on delivery place in rural Zambia: a study of linked national data in a geographic information system. PLoS Med. 2011;8:e1000394. doi: 10.1371/journal.pmed.1000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabrysch S, Simushi V, Campbell OM. Availability and distribution of, and geographic access to, emergency obstetric care in Zambia. Int J Gynaecol Obstet. 2011;114:174–9. doi: 10.1016/j.ijgo.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Stekelenburg J, Kyanamina S, Mukelabai M, Wolffers I, van Roosmalen J. Waiting too long: low use of maternal health services in Kalabo, Zambia. Trop Med Int Health. 2004;9:390–8. doi: 10.1111/j.1365-3156.2004.01202.x. [DOI] [PubMed] [Google Scholar]
- 5.Potts D. Counter-urbanisation on the Zambian copperbelt? Interpretations and implications. Urban Studies. 2005;42:583–609. doi: 10.1080/00420980500060137. [DOI] [Google Scholar]
- 6.Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Educ Res. 2007;22:166–76. doi: 10.1093/her/cyl060. [DOI] [PubMed] [Google Scholar]
- 7.Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria–looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43. doi: 10.1186/1471-2393-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McPherson RA, Khadka N, Moore JM, Sharma M. Are birth-preparedness programmes effective? Results from a field trial in Siraha district, Nepal. J Health Popul Nutr. 2006;24:479–88. [PMC free article] [PubMed] [Google Scholar]
- 9.Powell-Jackson T, Hanson K. Financial incentives for maternal health: impact of a national programme in Nepal. J Health Econ. 2012;31:271–84. doi: 10.1016/j.jhealeco.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Hatt L, Nguyen H, Sloan N, Miner S, Magvanjav O, Sharma A, et al. Economic evaluation of demand-side financing (DSF) program for maternal health in Bangladesh Bethesda: Abt Associates Inc; 2010. Available from: http://reliefweb.int/sites/reliefweb.int/files/resources/Bangladesh%20DSF%20evaluation_FINAL_Feb%202010.pdf [accessed 8 October 2012].
- 11.Alam K, Khan JA, Walker DG. Impact of dropout of female volunteer community health workers: an exploration in Dhaka urban slums. BMC Health Serv Res. 2012;12:260. doi: 10.1186/1472-6963-12-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brenner JL, Kabakyenga J, Kyomuhangi T, Wotton KA, Pim C, Ntaro M, et al. Can volunteer community health workers decrease child morbidity and mortality in southwestern Uganda? An impact evaluation. PLoS One. 2011;6:e27997. doi: 10.1371/journal.pone.0027997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harnessing volunteerism in support of maternal and newborn health goals Lewes: Health Partners International; 2012. Available from: http://www.healthpartners-int.co.uk/our_projects/documents/MAMaZPolicyBrief-Volunteerism_000.pdf [accessed 8 October 2013].