Abstract
Purpose
The aim of this study was to assess the feasibility and safety of laparoscopic resection following the insertion of self-expanding metallic stents (SEMS) for the treatment of obstructing left-sided colon cancer.
Methods
Between October 2006 and December 2012, laparoscopic resection following SEMS insertion was performed in 54 patients with obstructing left-sided colon cancer.
Results
All 54 procedures were technically successful without the need for conversion to open surgery. The median interval from SEMS insertion to laparoscopic surgery was 9 days (range, 3-41 days). The median surgery time was 200 minutes (range, 57-444 minutes), and estimated blood loss was 50 mL (range, 10-3,500 mL). The median time to soft diet was 4 days (range, 2-8 days) and possible length of stay (hypothetical length of stay according to the discharge criteria) was 7 days (range, 4-22 days). The median total number of lymph nodes harvested was 23 (range, 8-71) and loop ileostomy was performed in 2 patients (4%). Six patients (11%) developed postoperative complications: 2 patients with anastomotic leakages, 1 with bladder leakage, and 3 with ileus. There was no mortality within 30 days.
Conclusion
The present study shows that the presence of a SEMS does not compromise the laparoscopic approach. Laparoscopic resection following stent insertion for obstructing left-sided colon cancer could be performed with a favorable safety profile and short-term outcome. Large-scale comparative studies with long-term follow-up are needed to demonstrate a significant benefit of this approach.
Keywords: Colonic neoplasms, Stents, Laparoscopy
INTRODUCTION
About 15-20% of patients with colorectal carcinoma present with acute obstruction that requires urgent decompression at presentation [1,2]. The morbidity and mortality rates of emergency surgery in such cases are reported to be 10% and 30%, respectively [3]. In the emergency setting, although Hartmann's procedure (resection of the colonic segment involved with end colostomy) is still popular, primary resection and anastomosis can be achieved by performing segmental resection with intraoperative "on-table lavage" or subtotal colectomy with ileocolic anastomosis [4,5].
Self-expanding metallic stents (SEMS) have been used both as a palliative treatment for patients with obstructive colorectal cancer in whom resection is not curative or as a bridge to surgery for potentially resectable colorectal cancer. As a bridge to surgery, SEMS allows for mechanical bowel preparation, converts an emergency surgery to an elective surgery, and makes single-stage surgical resection possible. Recently, SEMS has became the treatment of choice in many centers with facilities available to relieve left colonic obstruction [6].
Since laparoscopy-assisted colectomy for colon cancer was first reported in 1991 [7], multicenter prospective randomized trials have established that laparoscopic colectomy for curable colon cancer is not inferior to conventional open surgery and has favorable short-term outcomes [8-11]. However, colonic obstruction has been considered to be a relative contraindication for laparoscopic surgery due to poor surgical field caused by the distended bowel and potential hazard of injury to the fragile bowel. SEMS as a bridge to surgery increases the possibility of laparoscopic resection after bowel preparation in an elective setting. The combination of the 2 minimally invasive techniques can enable single-stage surgical resection with favorable short-term outcomes.
The aim of this study was to assess the feasibility and safety of laparoscopic resection following stent insertion for obstructing left-sided colon cancer.
METHODS
Between October 2006 and December 2012, laparoscopic resection following stent insertion as a bridge to surgery was performed in 54 patients with obstructing left-sided colon cancer at Severance Hospital, Yonsei University College of Medicine. Information regarding patient demographics was obtained from a prospectively collected Yonsei Colorectal Cancer Database that included data on age, sex, body mass index, tumor location, stent indwelling time, type of surgery, and preoperative carcinoembryonic antigen. Perioperative details included operative time, blood loss, days to first flatus and soft diet, length of hospital stay, perioperative complications, and histopathological findings. All the patients had clinical features of colonic obstruction such as obstipation and abdominal distension at presentation and the diagnosis was confirmed with plain abdominal film and/or computed tomography (CT) scan. CT scans of the abdomen and pelvis were performed in all patients before placing colonic stents. The location of the tumor was categorized as descending colon, sigmoid colon, rectosigmoid colon (distal border of tumor, between 15 cm from the anal verge and rectosigmoid junction), upper (10-15 cm from the anal verge), and middle (5-10 cm). In this study, hospital stay was recorded as the observed hospital stay and possible hospital stay. The observed hospital stay was defined as the total period from the surgery date to the discharge date and the possible hospital stay was defined as the hypothetical length of stay according to the discharge criteria. The discharge criteria included tolerance of soft diet and no postoperative complications, because discharge may be delayed due to individual patient preference. A conversion to open surgery was defined as interruption of the laparoscopic approach followed by the need for a laparotomy at any time to complete the entire surgical procedure. Data are expressed as median (range). Analyses were performed by using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA).
Endoscopic technique
Stent placement was performed by the endoscopists at Severance Hospital by using SEMS techniques. After identifying a left colonic obstructive lesion by using flexible colonoscope, a guide wire was passed through the narrowed lumen of the obstructed colon under fluoroscopic guidance. The metallic stent was inserted through the working channel of the endoscope over the guide wire. Abdominal radiography was performed on the same day of the procedure and the next day following stenting to confirm stent expansion and adequate position. Elective laparoscopic resection was scheduled several days after stent placement.
Surgical procedures
For bowel preparation, colonic lavage was performed on the day before surgery with 4 L of Colyte. Patients were given prophylactic antibiotics. All surgical procedures were carried out under general anesthesia, with the patients in the lithotomy position. We created an open access pneumoperitoneum around the umbilicus by using CO2 gas to a maximum pressure of 12 mmHg. We used 5 ports: 2 ports (12 mm) for a camera (umbilicus); 1 working port (above the umbilicus right-side midclavicular line); and another 3 ports (5 mm) in each remaining quadrant. After achieving pneumoperitoneum with insufflations of CO2 to 12 mmHg, a 10-mm diameter telescope with fiber optic light transmission and 30°-angled view was inserted through a camera port. The procedures performed were medial to lateral mobilization of the sigmoid and descending colon along the avascular plane, dissection of lymph nodes around the root of the inferior mesenteric artery, and full splenic flexure mobilization. In cases of anterior and low anterior resection, high or low ligation of inferior mesenteric artery, rectal dissection by using tumor-specific mesorectal excision principles, and division by using an Echelon 60 (Ethicon Endo-surgery, a subsidiary of Johnson & Johnson, Cincinnati, OH, USA) was performed and the end-to-end intracorporeal anastomosis with a double stapling technique was carried out. In cases of left hemicolectomy, the left branch of the middle colic and left colic vessels were ligated and the anastomosis was performed extracorporeally by using a hand-sewing technique. At the end of the surgery, the additional port site was used for pelvic drain placement.
RESULTS
The baseline demographics of patients are shown in Table 1. The median age of the 54 patients was 68 years (range, 26-86 years), with 20 women and 34 men, and body mass index was 22.9 kg/m2 (range, 16.1-31.3 kg/m2). There were 14 cases of descending colon (26%), 28 cases of sigmoid colon (52%), 7 cases of rectosigmoid colon (13%), 2 cases of upper rectal cancer (5%), and 3 cases of middle rectal cancer (5%). The median interval from stent insertion to laparoscopic surgery was 9 days (range, 3-41 days). The procedures included 12 left hemicolectomies, 28 anterior resections, 13 low anterior resections, and 1 segmental resection of the colon and loop ileostomy was performed in 2 patients (4%). Among 54 patients, covered (n = 15) and uncovered stents (n = 33) were used.
Table 1.
Patient characteristics (n=54)
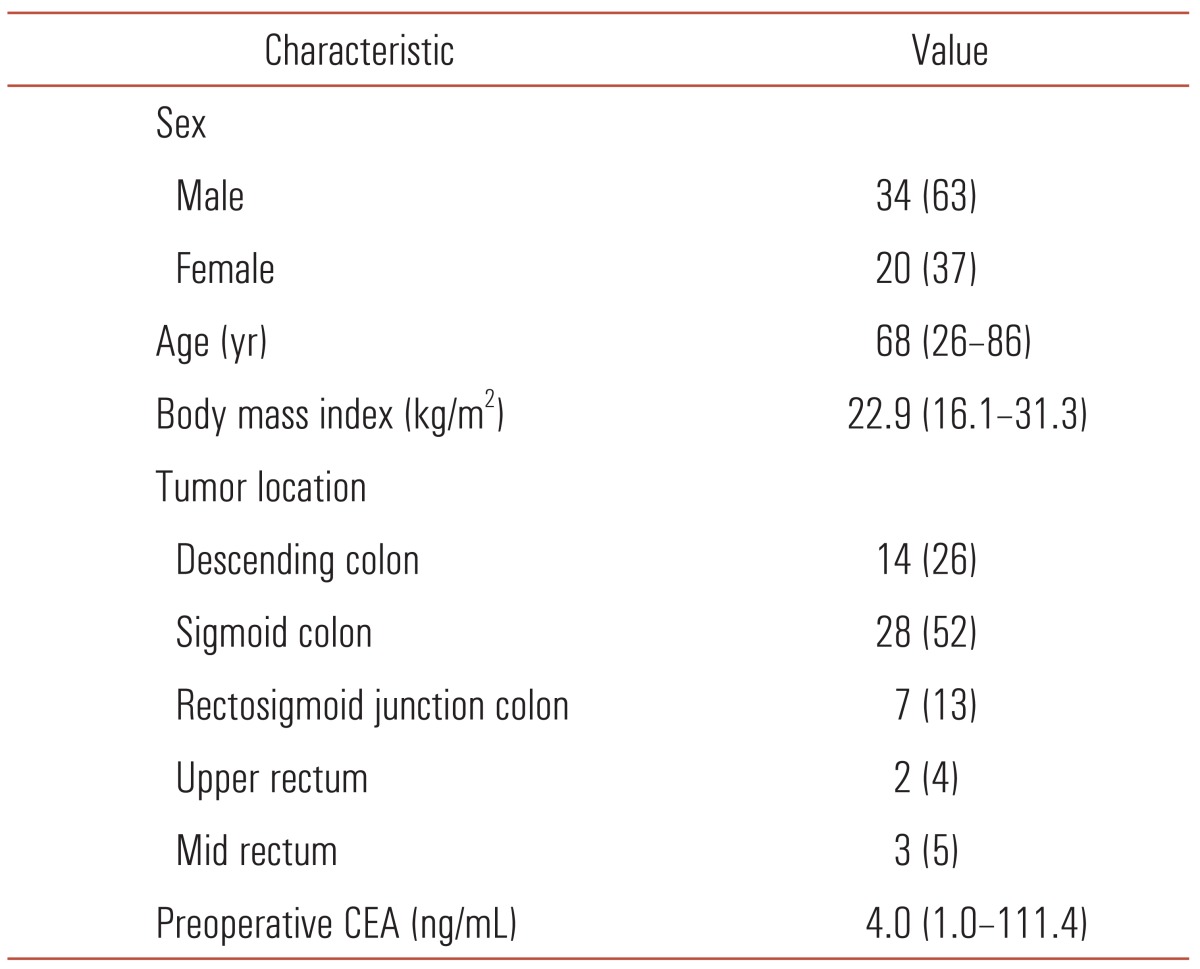
Values are presented as number (%) or median (range).
CEA, carcinoembryonic antigen.
All 54 procedures were technically successful without the need for conversion to open surgery (Table 2). The median surgery time was 200 minutes (range, 57-444 minutes) and estimated blood loss was 50 mL (range, 10-3,500 mL). The median time to first flatus and soft diet were 3 days (range, 1-6 days) and 4 days (range, 2-8 days), respectively. The observed and possible hospital stay was 8 days (range, 5-22 days) and 7 days (range, 4-22 days), respectively. Six patients (11%) developed postoperative complications: 2 patients with anastomotic leakages, 1 with bladder leakage, and 3 with ileus. One case of minor anastomotic leakage was treated with conservative management and observed, and 1 case of major leakage was treated by performing laparoscopic drainage and protective ileostomy. Reoperation was required in 1 patient with anastomotic leak. The procedure was not associated with any mortality.
Table 2.
Perioperative outcomes
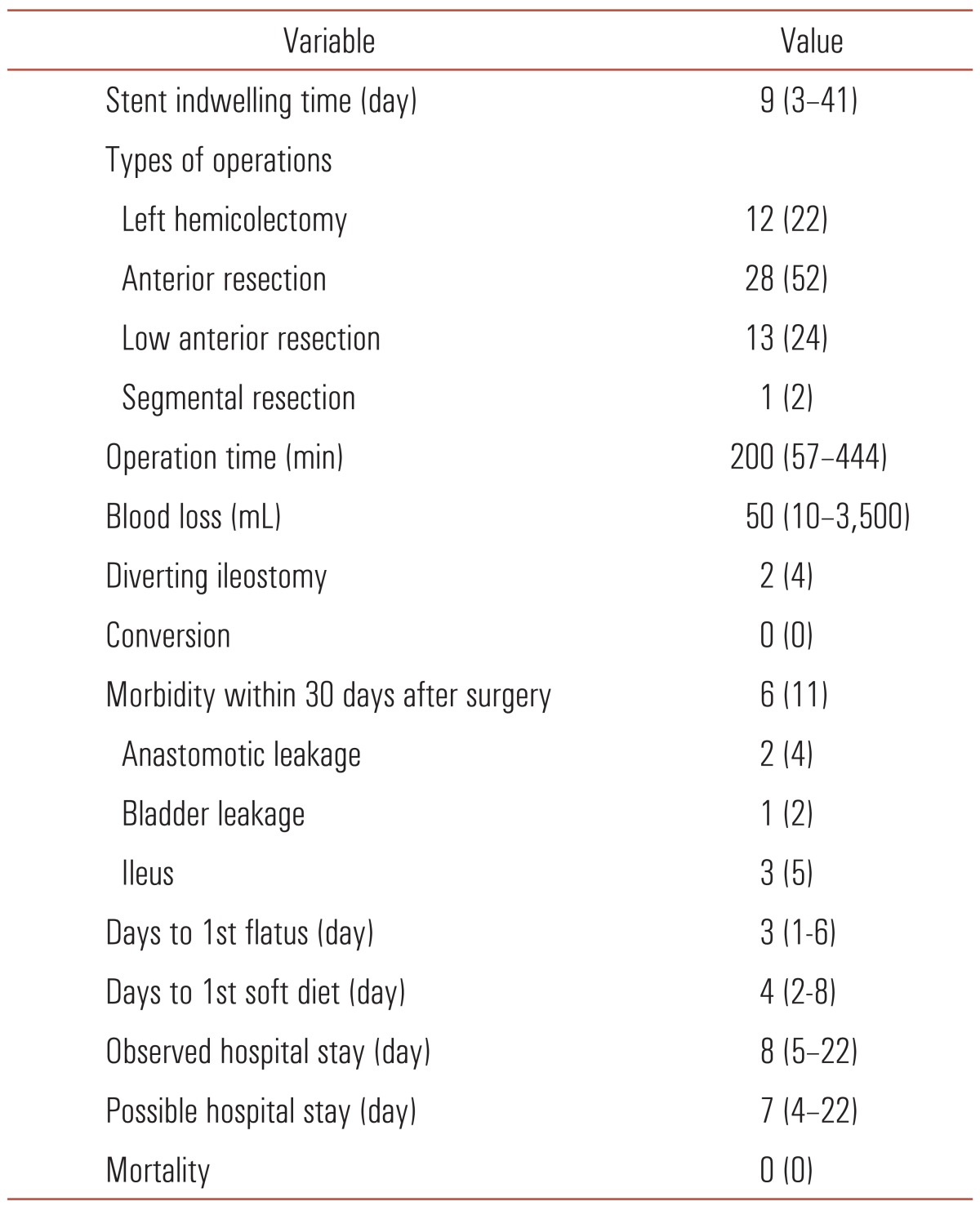
Values are presented as number (%) or median (range).
Pathologic characteristics are displayed in Table 3. The median tumor size was 6 cm (range, 2.5-10.0 cm) and total number of lymph nodes harvested was 23 (range, 8-71). The median proximal and distal resection margins were 10.0 cm (range, 5.0-33.0 cm) and 6.5 cm (range, 2.0-20.0).
Table 3.
Postoperative pathologic outcomes
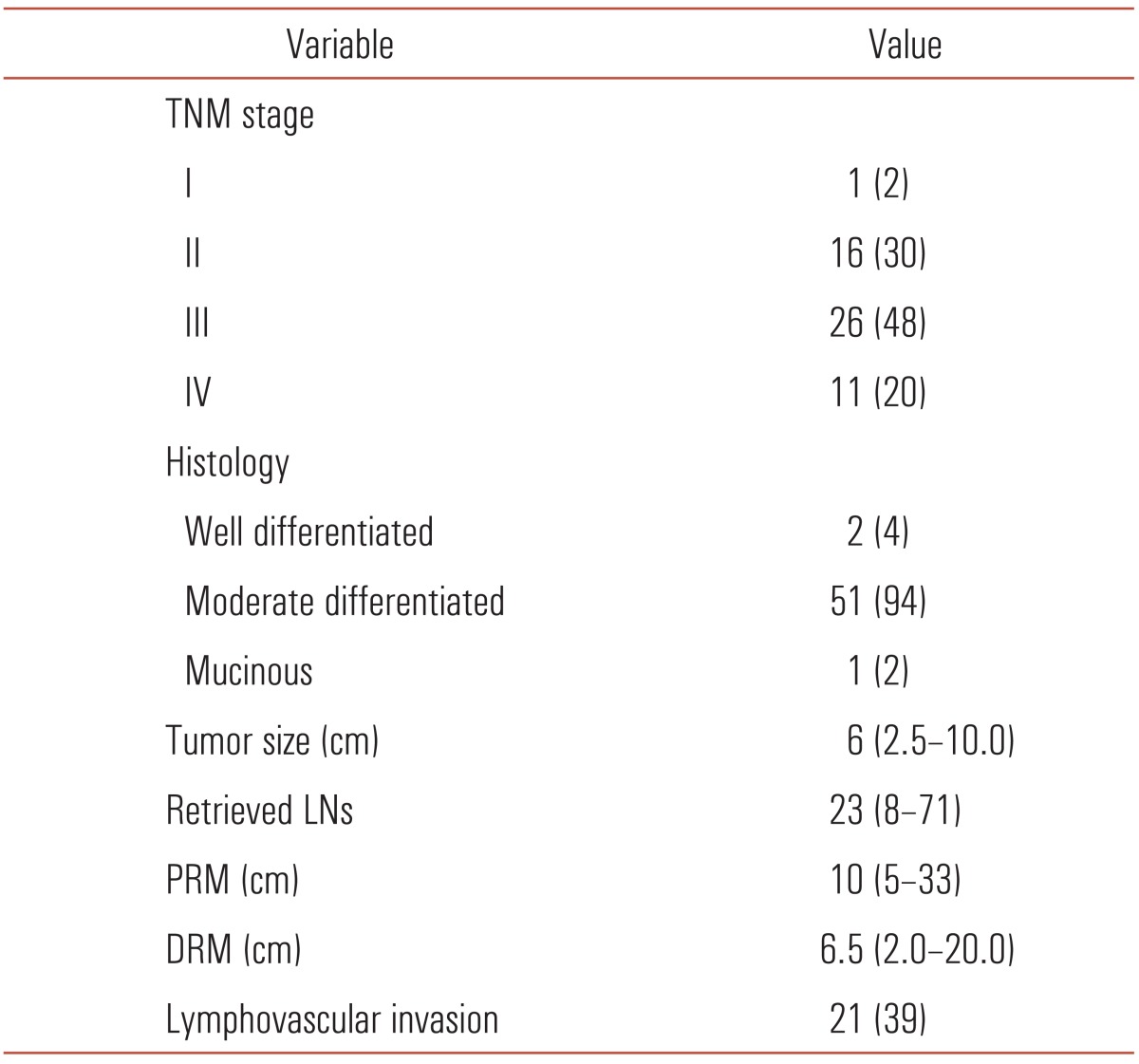
Values are presented as number (%) or median (range).
LNs, lymph nodes; PRM, proximal resection margin; DRM, distal resection margin.
DISCUSSION
About 80% of colonic obstructions are due to malignant lesions [3,12] and 15-20% of patients with colorectal carcinoma present with acute obstruction that requires urgent decompression at initial presentation [1,2]. In the emergency setting, there are some surgical options including a 2-stage surgery (Hartmann's procedure and reconstruction of the colon) and a 1-stage surgery (subtotal colectomy or "on-table lavage" surgery). However, only 60% of patients who undergo a Hartmann's procedure achieve closure of the colostomy [3,13] and subtotal colectomy has the disadvantage of an increased daily frequency of stools. In addition, the morbidity and mortality rates of emergency surgery in such cases are reported to be 10% and 30%, respectively [2].
While endoscopic stent implantation was initially used for the treatment of malignant esophageal, duodenal, and biliary strictures [14-16], its role has expanded to the treatment of colonic obstruction [17]. SEMS for colonic obstruction was first reported in 1991 by Dohmoto [17] as a palliative treatment for an obstructing rectal cancer and it has become the optimal treatment alternative to colostomy for palliation in advanced colon cancer [18,19]. Recently, this method was extended to relieve colonic obstruction as a "bridge to surgery" before surgical resection. As a bridge to surgery, SEMS allows mechanical bowel preparation and converts an emergency surgery to an elective surgery that increases the likelihood of a primary anastomosis and laparoscopic resection. SEMS became the treatment of choice in many centers with facilities available to relieve left colonic obstruction [6].
Laparoscopic colon resection for malignant disease has been accepted since multicenter prospective randomized trials established that laparoscopic colectomy for curable colon cancer is not inferior to conventional open surgery, and has favorable short-term outcomes in terms of earlier return of bowel motility, less pain and use of analgesics, and a shorter hospital stay [8-11]. However, colonic obstruction has been considered as a relative contraindication for laparoscopic surgery due to poor surgical field caused by the distended bowel and potential hazard of injury to the fragile bowel.
Morino et al. [20] first reported an approach to malignant colonic obstructions involving laparoscopic resection following stent insertion in 2002, and some other groups have reported similar studies [21-24]. Park et al. [25] compared the clinical results of 25 patients who underwent stent-laparoscopy with 70 patients who underwent resection of the colon or rectum with primary anastomosis after intraoperative colon lavage, and Law et al. [26] compared open (n = 18) and laparoscopic approaches (n = 18) after SEMS insertion for colonic obstruction. However, while stent-laparoscopic treatment is becoming more popular, studies with a sizable number of patients are still lacking. To our knowledge, our study of 54 patients represents the largest series to date.
In the present study, perioperative outcomes, including surgery time of 200 minutes (range, 57-444 minutes), number of days to first gas passing of 3 days (range, 1-6 days), time to soft diet of 4 days (range, 2-8 days), and possible hospital stay of 7 days (range, 4-22 days), are comparable with those of previous studies [24-26]. In addition, these results are consistent with perioperative outcomes of laparoscopic colonic resection at our institute [27]. These results show the advantages of laparoscopic surgery and that the presence of a SEMS does not compromise the laparoscopic approach.
There were 2 instances of anastomotic leaks in this study. In the 1 case of minor leak, which was treated with conservative management, CT scan showed diffuse edematous change involving the entire colon proximal to the anastomosis that was consistent with "obstructive colitis." The term "obstructive colitis" refers to ulcero-inflammatory lesions occurring in the colon proximal to a completely or partially obstructing lesion [28]. If the ischemic lesion is involved in the anastomosis, the risk of anastomotic failure is increased. Therefore, it is important to check the status of mucosa at the proximal margin and the proximal remnant before performing anastomosis. If ulceration is noted, further resection of the bowel and obtaining the healthy mucosal margin must be considered.
Stent-laparoscopic treatment for obstructing colon cancer has some technical challenges. Balague et al. [21] stated that the rigidity of the colonic segment containing the stent and the tumor made its dissection more difficult than usual, and difficult laparoscopic techniques affected the surgery time, and Park et al. [25] reported that in some cases, colonic decompression was insufficient and made laparoscopic surgery more difficult. Bowel distension by gas and fecal material proximal to the obstruction may result in tearing of the muscular fibers and gentle manipulation is needed. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines for the laparoscopic resection of curable colon and rectal cancer recommended that atraumatic handling of the bowel should be achieved by blunt retraction, grasping of the epiploic appendages, and the use of atraumatic graspers [29]. Several advantages of the hand-assisted approach have been stated in some studies: the inserted hand can provide blunt dissection, better control of bleeding, and better organ retraction for more complex procedures or more difficult pathologies, and tactile feedback helps to identify lesions that are not clearly visible [30].
The limitations of this study include the retrospective nature and the lack of long-term and oncological outcomes and a control group. Therefore, large-scale studies comparing laparoscopy versus open resection after colonic stent as a bridge to definitive surgery or comparing stent-laparoscopic treatment to nonobstructing laparoscopic resection with long-term follow-up are needed to demonstrate a significant benefit of this approach.
In conclusion, the present study shows that the presence of a SEMS does not compromise the laparoscopic approach. Laparoscopic resection following stent insertion for obstructing left-sided colon cancer could be performed with a favorable safety profile and short-term outcome. Large-scale comparative studies with long-term follow-up are needed.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Phillips RK, Hittinger R, Fry JS, Fielding LP. Malignant large bowel obstruction. Br J Surg. 1985;72:296–302. doi: 10.1002/bjs.1800720417. [DOI] [PubMed] [Google Scholar]
- 2.Serpell JW, McDermott FT, Katrivessis H, Hughes ES. Obstructing carcinomas of the colon. Br J Surg. 1989;76:965–969. doi: 10.1002/bjs.1800760932. [DOI] [PubMed] [Google Scholar]
- 3.Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br J Surg. 1994;81:1270–1276. doi: 10.1002/bjs.1800810905. [DOI] [PubMed] [Google Scholar]
- 4.Mealy K, Salman A, Arthur G. Definitive one-stage emergency large bowel surgery. Br J Surg. 1988;75:1216–1219. doi: 10.1002/bjs.1800751224. [DOI] [PubMed] [Google Scholar]
- 5.Lau PW, Lo CY, Law WL. The role of one-stage surgery in acute left-sided colonic obstruction. Am J Surg. 1995;169:406–409. doi: 10.1016/s0002-9610(99)80185-8. [DOI] [PubMed] [Google Scholar]
- 6.Sagar J. Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev. 2011;(11):CD007378. doi: 10.1002/14651858.CD007378.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy) Surg Laparosc Endosc. 1991;1:144–150. [PubMed] [Google Scholar]
- 8.Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061–3068. doi: 10.1200/JCO.2006.09.7758. [DOI] [PubMed] [Google Scholar]
- 9.COLOR Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Dig Surg. 2000;17:617–622. doi: 10.1159/000051971. [DOI] [PubMed] [Google Scholar]
- 10.Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655–662. doi: 10.1097/SLA.0b013e318155a762. [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa H, Kabeshima Y, Watanabe M, Yamamoto S, Kitajima M. Randomized controlled trial of laparoscopic versus open colectomy for advanced colorectal cancer. Surg Endosc. 2003;17:636–640. doi: 10.1007/s00464-002-8516-4. [DOI] [PubMed] [Google Scholar]
- 12.Rault A, Collet D, Sa Cunha A, Larroude D, Ndobo'epoy F, Masson B. Surgical management of obstructed colonic cancer. Ann Chir. 2005;130:331–335. doi: 10.1016/j.anchir.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Wong RW, Rappaport WD, Witzke DB, Putnam CW, Hunter GC. Factors influencing the safety of colostomy closure in the elderly. J Surg Res. 1994;57:289–292. doi: 10.1006/jsre.1994.1147. [DOI] [PubMed] [Google Scholar]
- 14.Kaw M, Singh S, Gagneja H, Azad P. Role of self-expandable metal stents in the palliation of malignant duodenal obstruction. Surg Endosc. 2003;17:646–650. doi: 10.1007/s00464-002-8527-1. [DOI] [PubMed] [Google Scholar]
- 15.Knyrim K, Wagner HJ, Bethge N, Keymling M, Vakil N. A controlled trial of an expansile metal stent for palliation of esophageal obstruction due to inoperable cancer. N Engl J Med. 1993;329:1302–1307. doi: 10.1056/NEJM199310283291803. [DOI] [PubMed] [Google Scholar]
- 16.Knyrim K, Wagner HJ, Pausch J, Vakil N. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy. 1993;25:207–212. doi: 10.1055/s-2007-1010294. [DOI] [PubMed] [Google Scholar]
- 17.Dohmoto M. New method: endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Dig. 1991;3:1507–1512. [Google Scholar]
- 18.Law WL, Choi HK, Lee YM, Chu KW. Palliation for advanced malignant colorectal obstruction by self-expanding metallic stents: prospective evaluation of outcomes. Dis Colon Rectum. 2004;47:39–43. doi: 10.1007/s10350-003-0005-x. [DOI] [PubMed] [Google Scholar]
- 19.Maetani I, Tada T, Ukita T, Inoue H, Yoshida M, Saida Y, et al. Self-expandable metallic stent placement as palliative treatment of obstructed colorectal carcinoma. J Gastroenterol. 2004;39:334–338. doi: 10.1007/s00535-003-1299-0. [DOI] [PubMed] [Google Scholar]
- 20.Morino M, Bertello A, Garbarini A, Rozzio G, Repici A. Malignant colonic obstruction managed by endoscopic stent decompression followed by laparoscopic resections. Surg Endosc. 2002;16:1483–1487. doi: 10.1007/s00464-001-9182-7. [DOI] [PubMed] [Google Scholar]
- 21.Balagué C, Targarona EM, Sainz S, Montero O, Bendahat G, Kobus C, et al. Minimally invasive treatment for obstructive tumors of the left colon: endoluminal self-expanding metal stent and laparoscopic colectomy. Preliminary results. Dig Surg. 2004;21:282–286. doi: 10.1159/000080202. [DOI] [PubMed] [Google Scholar]
- 22.Law WL, Choi HK, Lee YM, Chu KW. Laparoscopic colectomy for obstructing sigmoid cancer with prior insertion of an expandable metallic stent. Surg Laparosc Endosc Percutan Tech. 2004;14:29–32. doi: 10.1097/00129689-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Dulucq JL, Wintringer P, Beyssac R, Barberis C, Talbi P, Mahajna A. One-stage laparoscopic colorectal resection after placement of self-expanding metallic stents for colorectal obstruction: a prospective study. Dig Dis Sci. 2006;51:2365–2371. doi: 10.1007/s10620-006-9223-0. [DOI] [PubMed] [Google Scholar]
- 24.Chung TS, Lim SB, Sohn DK, Hong CW, Han KS, Choi HS, et al. Feasibility of single-stage laparoscopic resection after placement of a self-expandable metallic stent for obstructive left colorectal cancer. World J Surg. 2008;32:2275–2280. doi: 10.1007/s00268-008-9695-5. [DOI] [PubMed] [Google Scholar]
- 25.Park IJ, Choi GS, Kang BM, Lim KH, Lee IT, Jeon SW, et al. Comparison of one-stage managements of obstructing left-sided colon and rectal cancer: stent-laparoscopic approach vs. intraoperative colonic lavage. J Gastrointest Surg. 2009;13:960–965. doi: 10.1007/s11605-008-0798-y. [DOI] [PubMed] [Google Scholar]
- 26.Law WL, Poon JT, Fan JK, Lo OS. Colorectal resection after stent insertion for obstructing cancer: comparison between open and laparoscopic approaches. Surg Laparosc Endosc Percutan Tech. 2013;23:29–32. doi: 10.1097/SLE.0b013e318275743b. [DOI] [PubMed] [Google Scholar]
- 27.Cho JH, Lim DR, Hur H, Min BS, Baik SH, Lee KY, et al. Oncologic outcomes of a laparoscopic right hemicolectomy for colon cancer: results of a 3-year follow-up. J Korean Soc Coloproctol. 2012;28:42–48. doi: 10.3393/jksc.2012.28.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Toner M, Condell D, O'Briain DS. Obstructive colitis: ulceroinflammatory lesions occurring proximal to colonic obstruction. Am J Surg Pathol. 1990;14:719–728. [PubMed] [Google Scholar]
- 29.Zerey M, Hawver LM, Awad Z, Stefanidis D, Richardson W, Fanelli RD, et al. SAGES evidence-based guidelines for the laparoscopic resection of curable colon and rectal cancer. Surg Endosc. 2013;27:1–10. doi: 10.1007/s00464-012-2592-x. [DOI] [PubMed] [Google Scholar]
- 30.Hassan I, You YN, Cima RR, Larson DW, Dozois EJ, Barnes SA, et al. Hand-assisted versus laparoscopic-assisted colorectal surgery: practice patterns and clinical outcomes in a minimally-invasive colorectal practice. Surg Endosc. 2008;22:739–743. doi: 10.1007/s00464-007-9477-4. [DOI] [PubMed] [Google Scholar]


