Abstract
Background and Purpose:
We sought to determine the current practices and plans for departmental hiring of neurohospitalists at academic medical centers and to identify the core features of a neurohospitalist training program.
Methods:
We surveyed department chairs or residency program directors at 123 Accreditation Council for Graduate Medical Education (ACGME)-accredited US adult neurology training programs.
Results:
Sixty-three(51% response rate) responded, 76% of whom were program directors. In all, 24 (38%) academic neurology departments reported employing neurohospitalists, and an additional 10 departments have plans to hire neurohospitalists in the next year. In all, 4 academic neurology departments have created a neurohospitalist training program, and 10 have plans to create a training program within the next 2 years. Hospitals were the most frequent source of funding for established and planned programs (93% of those reporting). Most (n = 39; 65%) respondents felt that neurohospitalist neurology should be an ACGME-accredited fellowship. The highest priority neurohospitalist training elements among respondents included stroke, epilepsy, and consult neurology as well as patient safety and cost-effective inpatient care. The most important procedural skills for a neurohospitalist, as identified by respondents, include performance of brain death evaluations, lumbar punctures, and electroencephalogram interpretation.
Conclusions:
Neurohospitalists have emerged as subspecialists within neurology, growing both in number and in scope of responsibilities in practice. Neurohospitalists are in demand among academic departments, with many departments developing their existing presence or establishing a new presence in the field. A neurohospitalist training program may encompass training in stroke, epilepsy, and consult neurology with additional focus on patient safety and cost-effective care.
Keywords: neurohospitalist, fellowship, training, academic, education
Introduction
The term “hospitalist” was coined in 1996 to describe specialists in inpatient medicine,1 and their rise was initially in response to the diagnosis-related, group-based reimbursement system and its associated pressures for reduction in length of stay as well as total cost.2 Hospitalist programs were often created with financial support from their respective hospitals, with their value determined by the cost and efficiency of care they provided.2 Subsequently, hospitalist fellowships became valued by employers and practicing hospitalists, although the majority of hospitalists are not fellowship trained.3 Training in curriculum, quality and health care delivery, and business and health administration have been suggested as optional complements to the core academic medical hospitalist training elements of communication, leadership, billing/coding, and clinical care.3,4
Based on the model developed within internal medicine, pediatrics, and family medicine, neurohospitalists have been defined as physicians whose primary focus is the care of inpatients with, or at risk for, neurologic disease.5–7 The Neurohospitalist Section of the American Academy of Neurology (AAN) now totals over 470 members, a near 5-fold increase in only 4 years of self-identified neurohospitalists within the AAN.6,7 Neurohospitalists work in academic and nonacademic centers within varying practice models throughout the United States.6,8 Conditions commonly encountered by neurohospitalists include stroke, encephalitis (both infectious and immune mediated), refractory seizures, and generally patients that tend to have higher acuity, requiring greater care coordination and more complex medical decision making.5,6,8 The coordination of patient care transitions from the inpatient to outpatient settings, models of practice, measures of care quality, neurological disease and treatment, and resident education are among the natural interests of neurohospitalists.5,6 There is an ongoing discussion regarding the necessity of neurohospitalist-specific training, and the core features and standards for a potential fellowship or advanced specialist practice training program and the distinction of such training from other neurology fellowship training are yet to be defined.5,6,8,9
Here, we present a national survey of department chairs and residency program directors of Accreditation Council for Graduate Medical Education (ACGME)-certified adult neurology training programs. We surveyed academic departments, as they are most likely to be involved in the development of neurohospitalist-specific training programs. This survey was designed to explore academic departmental plans for hiring and training neurohospitalists and to identify what such training should entail.
Methods
Inclusion Criteria
The 123 neurology departments within the United States accredited by ACGME for resident training were surveyed.10 For this survey, neurohospitalists were defined according to the American Academy of Neurology Neurohospitalist section as “physicians who have as their primary focus the care of inpatients with, or at risk for, neurologic disease.”7 Using publically available resources, we identified academic neurology department chairs and residency program directors.11 Department chairs and residency program directors were surveyed, as it was felt that they would (1) have knowledge of their program’s needs for neurohospitalists and (2) provide departmental leadership’s perspectives on elements of a neurohospitalist training program. A link to the electronic survey was emailed to department chairs, asking that they, their residency program directors, or other individuals with appropriate expertise within their department complete the survey. The electronic survey was sent to residency program directors of a program if there was no response from the respective department chair, and they were asked to complete the survey. Nonrespondents were contacted using reminder emails and telephone calls. Responses were collected between March 27 and June 27, 2012. This study was approved by the institutional review board of Johns Hopkins School of Medicine.
Survey Instrument
The survey instrument was designed in collaboration with senior faculty from the Johns Hopkins Department of Neurology and School of Public Health. Focus groups with residents and neurology department leadership were held to validate the survey (Appendix e-1 in Supplemental Material). The survey contained 19 questions related to neurohospitalist training and 10 questions on hospital, department, program, and respondent characteristics. A second portion of the survey included additional questions regarding the impact of residency duty hours on neurology programs; results from this portion will be presented in a separate manuscript. A multiple-choice list for many of the questions was provided to respondents for their selection, some of which could accommodate multiple answers. Respondents were asked about their perception of neurohospitalists and neurohospitalist training by choosing their agreement with statements measured by a 5-point Likert-type scale of importance or agreement. Given concern for potential asymmetry in knowledge across respondents and to assure accurate information collection, we included the option for respondents to select “do not know” on some questions or opt out of a question altogether.
Data Analysis
The Wilcoxon-Mann-Whitney test was used to examine the differences between respondents and nonrespondents in first-year resident class size as reported by the Fellowship and Residency Electronic Interactive Database Access (FREIDA) system and 2011 estimated metropolitan size from the US Census Bureau.10 Fisher exact test was used to assess differences in program type (community based, community-based university affiliated, university affiliated) as indicated by FREIDA. Differences between respondents from departments or residency programs that employ neurohospitalists or plan to create a neurohospitalist fellowship/training program compared to those that do not were evaluated across self-reported characteristics (hospital bed size, second postgraduate year (PGY-2) resident class size, department full-time equivalent faculty size, and neurological science bed size) using the Wilcoxon-Mann-Whitney test. For questions on neurohospitalist responsibilities, perceptions of training program elements, and opinions of neurohospitalists, where multiple options could be selected, McNemar exact test was used to determine differences in the marginal frequency of selections between 2 parts of a question. The results for responses on a 5-point Likert-type scale were dichotomized for the statistical analysis. Specifically, “very important and important” or “strongly agree and agree” were grouped and compared to the remaining 3 options on a 5-point scale. All tests were conducted at the 2-sided significance level of 5% using STATA software, version 12.0 (StataCorp, College Station, Texas).
Results
Respondents
Responses were received from 63 of the 123 ACGME-accredited neurology departments (51% response rate). Respondents were either department chairs (23%), residency program directors (75%), or department administrators (n = 1; Table e-1 in Supplemental Material). In all, 71% of the respondents were from institutions whose primary hospital has ≥500 patient beds, and the mean number of neuroscience beds was 44. In all, 84% (n = 53) of the respondents were university affiliated. The average PGY-2 class size was 5.6 residents (standard deviation = 2.7; median = 5). There was no significant difference in region (P = .156), size of metropolitan area (P = .613), residency program type (P = .371), or first-year class size (P = .088; mean of 4.6 vs 5.7) for respondents compared to nonrespondents.
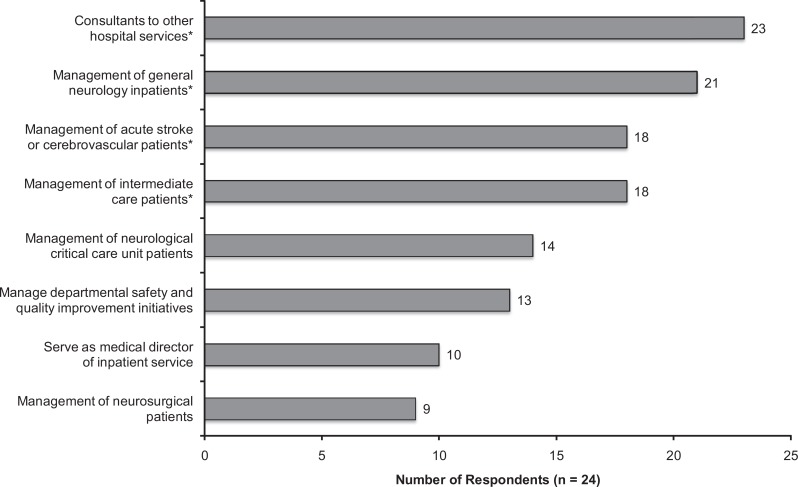
Neurohospitalist Employment
Of the responding academic neurology departments, 24 (38%) reported employing neurohospitalists (Table 1). Programs that currently employ neurohospitalists (n = 24) come from larger metropolitan statistical areas (mean: 14 87 959 vs 5 11 438; P = .02) and have larger resident class size (mean: 6.8 vs 5.1 residents; P = .04). These differences were no longer significant when adding in those that plan to hire neurohospitalists within the next year. Among these 24 departments, an average of 3 neurohospitalists were employed (72 overall). The most common responsibilities of neurohospitalists in these departments are consultation to other hospital services and the management of general neurology inpatients, acute stroke patients, or intermediate care patients (Figure 1). Of those already employing neurohospitalists, 10 departments have plans to hire a total of 15 neurohospitalists in the next year (21% increase in those already employing neurohospitalists). An additional 10 departments that do not currently employ neurohospitalists have plans to hire a total of 19 neurohospitalists in the next year (47% increase overall).
Table 1.
Department Practices and Plans for Neurohospitalist Employment and Training.
| Neurohospitalist Employment and Training Programs | No. of Survey Respondents (%) |
|---|---|
| Department employs neurohospitalists (n = 63) | |
| Yes | 24 (38) |
| No | 39 (62) |
| Number employed (n = 24) | |
| 1 | 8 (33) |
| 2 | 5 (21) |
| 3 | 5 (21) |
| ≥4 | 6 (25) |
| Mean (SD) | 3 (2.4) |
| Department plans to hire neurohospitalists (n = 63)a | |
| Yes | 20 (32) |
| No | 29 (46) |
| Do not know | 14 (22) |
| Number of intended hires (n = 20) | |
| 1 | 11 (55) |
| 2 | 6 (30) |
| 3 | 1 (5) |
| 4 | 2 (10) |
| Mean (SD) | 2 (1.0) |
| Department has a neurohospitalist training program (n = 63)b | |
| Yes | 4 (6) |
| Plans within 2 years | 10 (16) |
| No | 49 (78) |
| Funding source(s) for neurohospitalist training programs (n = 14)c | |
| Hospital Funding | 13 (93) |
| Medicare | 5 (36) |
| Neurology departmentd | 5 (36) |
| Medicaid | 4 (29) |
| School of medicine | 4 (29) |
| Department of defense | 1 (7) |
| Insurance | 1 (7) |
| Should neurohospitalists have an accredited fellowship (n = 60) | |
| Yes | 39 (65) |
| No | 21 (35) |
Abbreviation: SD, standard deviation.
aHiring plans include departments hiring first time as well as additional neurohospitalists.
bIncludes advanced specialist practice programs or nonaccredited neurohospitalist training programs.
cIn all, 9 respondents report multiple funding sources, while 1 respondent has not established or planned for funding at the time of the survey.
dIncludes department neuroscience service line.
Figure 1.
Primary responsibilities of neurohospitalists within respondent departments. *Consultants to other hospital services was the most frequently reported responsibility, although it was not selected significantly more frequently than management of general neurology inpatients (McNemar test: P = .625), acute stroke or cerebrovascular patients (McNemar test: P = .125), or intermediate care patients (McNemar test: P = .063).
Current State of Neurohospitalist Training Programs
Four academic neurology departments reported having created a neurohospitalist training program (Table 1). A total of 10 departments are planning to create a neurohospitalist training program within the next 2 years, 5 of which report plans for both a fellowship and an advanced specialist practice training program. No difference was detected in hospital bed size, neurology bed size, department faculty size, or resident class size between those departments with an existing or planned neurohospitalist training program and those without. The 3 most common funding sources for existing or planned training programs include hospitals, Medicare, and neurology department, while 9 report multiple sources of funding. The majority of respondents felt that neurohospitalist neurology should be an ACGME-accredited fellowship (n = 39; 65%). There was no difference in the opinion of whether there should be an ACGME-accredited neurohospitalist fellowship between those respondents from departments with (or planning for) a training program compared to those without (78.5% of 14 respondents vs 61% of 46 respondents; P = .187).
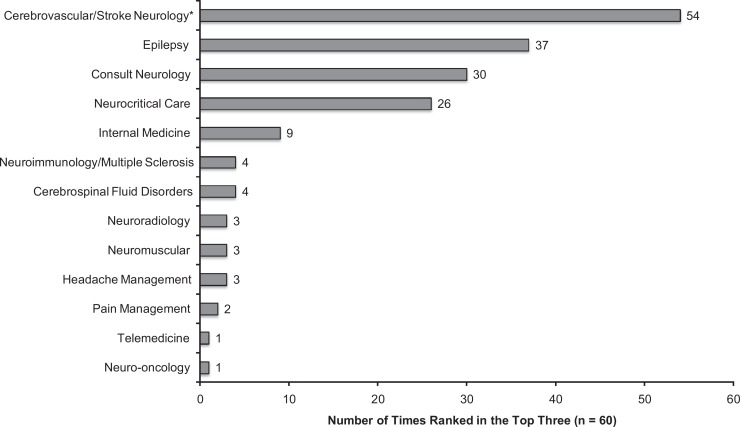
Elements of a Neurohospitalist Training Program
According to respondents, the 3 most important clinical elements of neurohospitalist training, as measured by the frequency of responses marked “very important”, were cerebrovascular or stroke neurology (n = 47; 76%), epilepsy (n = 32; 52%), and consult neurology (n = 32; 52%). Stroke or cerebrovascular neurology was selected as a very important clinical element of a neurohospitalist training program more frequently than all other clinical elements (McNemar test: P < .01). Similarly, respondents most frequently ranked stroke neurology (n = 54; 90%), epilepsy (n = 37; 62%), and consult neurology (n = 30; 50%) in their top 3 most important clinical elements (Figure 2). Notably, stroke neurology was selected more than all others (McNemar test: P < .001), with 73% of respondents (n = 44) indicating stroke as their number 1 choice.
Figure 2.
Perceived importance of clinical elements of a neurohospitalist training program. Respondents were asked to rank the top 3 most important clinical elements in their opinion. *Stroke or cerebrovascular neurology was ranked in the top 3 most important more frequently than all other options (McNemar test: P < .001). Epilepsy and consult neurology were significantly selected more than others except when compared to each other, stroke, and neurocritical care.
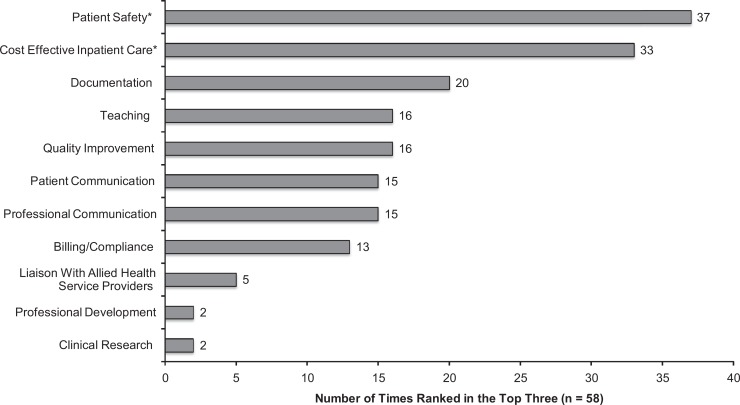
The 3 most important system-based practice elements of neurohospitalist training, as measured by the frequency of responses marked “very important”, were patient safety (n = 38; 64%), patient communication (n = 34; 58%), and professional communication (n = 30; 51%). Patient safety was the most frequently reported very important programmatic element, although not significantly more than patient communication (McNemar test: P = .549) or professional communication (McNemar test: P = .144). However, when ranking their top 3 most important programmatic elements, respondents ranked patient safety (n = 37; 64%) followed by cost-effective inpatient care (n = 33; 57%) most frequently (Figure 3).
Figure 3.
Perceived importance of programmatic elements of a neurohospitalist training program. Respondents were asked to rank the top 3 most important programmatic elements in their opinion. *Patient safety and cost-effective inpatient care were ranked more frequently than all other elements (McNemar test: P < .05), although one element was not significantly selected more than the other (P = .572).
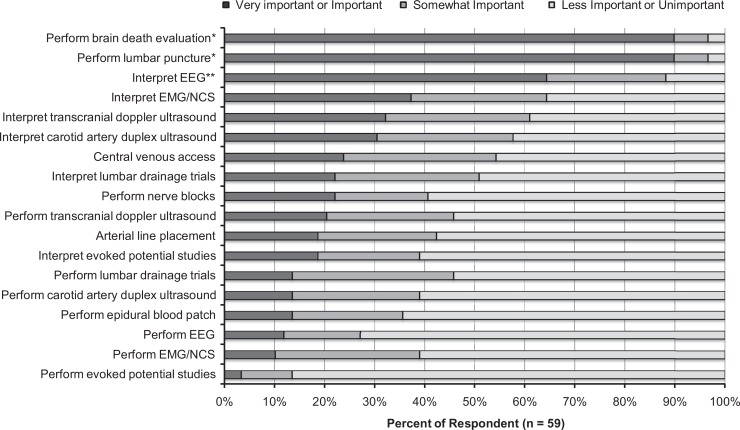
Brain death evaluations (n = 53; 90%), lumbar punctures (n = 53; 90%), and electroencephalogram (EEG) interpretation (n = 38; 64%) were most commonly perceived as very important or important procedural skills for neurohospitalist training (Figure 4).
Figure 4.
Perceived importance of procedural skills in a neurohospitalist training program. *Brain death evaluations and lumbar punctures were significantly selected as very important or important more frequently than all other procedural skills (McNemar test: P < .001). **EEG interpretation was significantly selected as very important or important more frequently than all procedural skills with fewer selections (McNemar test: P < .001). EEG indicates electroencephalogram; EMG, electromyogram; NCS, nerve conduction studies.
Perceptions of Neurohospitalists
The majority of respondents agreed or strongly agreed that neurohospitalists improve the coordination, continuity, safety, and quality of patient care as well as communication with patients and other health professionals (Figure e-1 in Supplemental Material). Most were of the opinion that neurohospitalists positively impact patient care. However, fewer than half of the respondents felt that neurohospitalists provide medical leadership, reduce readmissions, and improve resident education.
Discussion
This survey of academic neurology programs found that the size and scope of neurohospitalists and neurohospitalist training continues to grow. More than one-third of responding academic neurology departments currently employ neurohospitalists, and nearly one-third intend to hire their first or additional neurohospitalists within the next year. Neurohospitalists employed by academic neurology departments responding to our survey primarily serve as consultants or are the primary physicians for general neurology inpatients, intermediate care patients, and patients with cerebrovascular disease.
As has been noted in academic hospitalist medicine, academic neurohospitalists serve in additional capacities, including patient safety, quality improvement, and departmental leadership.4–6 For medical academic hospitalists, nonclinical time is used to develop the key components of academic career advancement, such as clinical research, education, patient safety, quality of care, and administration.4 Our study finds that departmental safety and quality improvement are primary responsibilities for neurohospitalists employed by more than half of the responding academic neurology departments.
As academic neurohospitalists already play both clinical and nonclinical roles within their departments, future academic neurohospitalists should be trained in a variety of clinical and programmatic areas. Nearly two-third (65%) of the respondents agreed that neurohospitalist neurology should be an ACGME-accredited fellowship. This is comparable to previous reports regarding internal medicine hospitalist fellowship training from the perspectives of employers and practicing hospitalists,3,12 although the majority of internal medicine hospitalists are not fellowship trained.13 Similarly, the opinion of academic neurology departmental leadership in favor of an accredited program suggests that there is substantial value in neurohospitalist training. Notably, the views of neurohospitalists themselves, in both academic and nonacademic practice, regarding the necessity of additional training is needed but yet to be fully described.
Our study suggests that the neurohospitalist-specific training need not only be through a fellowship model. For instance, several respondents reported that their departments had created or were creating both fellowships and nonaccredited, advanced specialist practice programs to provide this training, suggesting interest in developing multiple avenues for neurohospitalist training. Regardless of the model, training in cerebrovascular disease management, epilepsy, and consultative neurology were found to be the highest priority among respondents as core clinical features. The overlap of the priority areas for neurohospitalist training with core features of cerebrovascular, epilepsy, and neurointensive care fellowship training invites further conversation and investigation of distinguishing features of neurohospitalist training and practice.
The top procedural-based skills identified by respondents that neurohospitalist trainees should develop competence in were brain death examination and lumbar puncture. Notably, these skills differ from the most commonly performed and interpreted procedures by neurologists in the United States, EEG and electromyogram/nerve conduction studies.14 This highlights the marked difference in responsibilities of the neurohospitalist caring for acutely ill inpatients and outpatient neurologists encountering patients in a clinic setting.
In addition to clinical areas and procedural-based skills, respondents indicated that neurohospitalists should be trained in patient safety and cost-effective inpatient care, among several other highly valued systems-based practice elements. Similar to medical specialties, neurohospitalist programs may host opportunities for advanced degrees, fellowships, and short-term coursework in medical education, quality improvement, clinical research, and leadership/administration in environment of mentorship and academic support.4,15,16 This response by department leadership may reflect expectations of increasingly efficient and higher quality inpatient care, particularly given the adoption of the Affordable Care Act.17
In general, respondents perceived neurohospitalists favorably in their clinical and nonclinical roles, though it may be too early to fully assess their impact on patient care. The rapid emergence of neurohospitalists suggests a growing separation of inpatient and outpatient care for patients with neurological conditions. It remains to be seen how such a separation will affect patient care. Hospitalists in a variety of specialties are perceived to have a positive impact on areas ranging from quality and cost effectiveness of inpatient care to student education and are in demand because of this.12,18–22 In time, academic neurohospitalists may be perceived similarly. A recent study at one academic medical center demonstrated a decreased length of stay and cost associated with a neurohospitalist service as well as improved medical student satisfaction without compromise of resident satisfaction with clinician educators.22 However, the implications of a potentially more fragmented care model on the continuity of care for patients with chronic neurological conditions at high risk of hospitalization, such as those with recurrent stroke or refractory epilepsy, remain unknown.23 Perhaps reassuringly, discontinuity of care among internal medicine patients has not been attributable to hospitalists,24 while the presence of hospitalists does not independently predict readmission rates for some chronic medical conditions.25
Similar to medical hospitalist programs, the creation of neurohospitalist training programs has been primarily through hospital resources,2 with less significant contributions from the Centers for Medicare and Medicaid Services and neurology departments. As hospitals increasingly become pressured to produce low-cost, high-quality care in the wake of health reform and accountable care, they may have greater incentive to fund hospitalist initiatives.17 What influence a reliance on hospital funding has on the training of future neurohospitalists in academia remains to be seen.
Our study was limited to departments with adult neurology residency programs that responded; however, no significant difference was found in region, metropolitan size, resident class size, or program type between respondents and nonrespondents. In addition, our response rate of 51% is comparable to those of prior surveys of neurohospitalists regarding their clinical practice.6,8 The length and breadth of the survey instrument likely impacted the response rate. Also, selection bias may have been introduced in our sample, as the motivations for respondents were not clarified. The motivation of the study was to determine the practices and plans for department hiring and training of neurohospitalists from the perspective of academic departmental leadership, as they are likely to be involved in the development of neurohospitalist-specific training programs. However, the perspectives of academic and nonacademic neurohospitalists as well as nonacademic departmental leadership should also be incorporated in the formulation of key neurohospitalist training features. Respondents included individuals in department leadership with differing positions across academic departments and, therefore, may limit the reliability of the study. Our study was also limited by the possibility that some respondents may have had incomplete information on specific practices and plans for departmental hiring and, therefore, may have underreported. Our study may have underestimated departmental hiring plans of neurohospitalists, since just over 20% of respondents did not know department plans. In addition, we evaluated the perceived importance of neurohospitalist training elements from the perspective of department leadership, many of whom may not share the same opinions as neurohospitalists. Despite these limitations, this survey provides an estimate of the current practices and plans for academic department hiring and training of neurohospitalists and identifies key clinical and programmatic elements and procedural skills for a neurohospitalist training program from the perspective of academic departmental leadership.
Over the past several years, neurohospitalist medicine has risen as a new area of neurology and grown in both the number of neurohospitalists employed and the scope of responsibilities in practice. Responding academic neurology departments demonstrate a strong demand for neurohospitalists with departments looking to both develop their existing presence and establish a new presence in the field. Accredited fellowship training in neurohospitalist neurology is supported by 65% of the academic program respondents, and respondents identified clinical training in cerebrovascular disease, epilepsy, and consultative neurology as key elements of training. Neurohospitalists are also expected to be trained and subsequently lead in areas of patient safety and quality of care, much like their colleagues in hospitalist medicine. In general, neurohospitalists are viewed favorably, though it may be too early to appreciate the impact they will have in the evolving neurological training and clinical practice environments.
Acknowledgment
The authors would like to thank Dr Debra Roter, Professor of Health Behavior and Society at the Johns Hopkins Bloomberg School of Public Health, for her advice and guidance in survey and focus group design and Gita Byraiah, research assistant at the Johns Hopkins School of Medicine, Department of Neurology, for her assistance with institutional review board protocol design. Finally, the authors thank Dr Daniel Brotman, Associate Professor of Medicine and Director of the Johns Hopkins Hospitalist Program, and Dr Albert Wu, Professor of Health Policy and Management, Epidemiology and International Health and Director of Center for the Health Services and Outcomes Research in the Johns Hopkins Bloomberg School of Public Health, for their comments in manuscript preparation.
Supplemental Material
The online appendix, figure, and table are available at http://nho.sagepub.com/supplemental.
Footnotes
Authors’ Note: JP and BG contributed equally to the manuscript. AV had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. JP, BG, RD and AV contributed to drafting/revising the manuscript for content, including medical writing for content. JP, BG and AV contributed to the study concept or design. JP and BG contributed in analysis or interpretation of data. JP and BG contributed in acquisition of data. BG contributed in statistical analysis. RD and AV contributed in study supervision or coordination. Statistical analysis was conducted by BG (Johns Hopkins Bloomberg School of Public Health and University of Rochester School of Medicine and Dentistry).
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Probasco reports no disclosures. Mr George conducts research funded by the Parkinson Disease Foundation (Summer Student Fellowship No. PDF-SFW-1204) and has previously received research funding from the National Institute on Aging, American Academy of Neurology, and New York Academy of Medicine. Dr Dorsey is consultant to Lundbeck Pharmaceuticals and Medtronic and has received research funds from the Robert Wood Johnson Foundation, Prana Biotechnology, Google, and Lundbeck Pharmaceuticals. Dr Venkatesan has received research funds from the National Institutes of Health, the Howard Hughes Medical Institute, the Maryland Stem Cell Research Foundation, and the Accelerated Cure Project for Multiple Sclerosis.
References
- 1. Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514–517 [DOI] [PubMed] [Google Scholar]
- 2. Rachoin JS, Skaf J, Cerceo E, et al. The impact of hospitalists on length of stay and costs: systematic review and meta-analysis. Am J Manag Care. 2012;18(1):e23–e30 [PubMed] [Google Scholar]
- 3. Goodman PH, Januska A. Clinical hospital medicine fellowships: perspectives of employers, hospitalists, and medicine residents. J Hosp Med. 2008;3(1):28–34 [DOI] [PubMed] [Google Scholar]
- 4. Arora V, Fang MC, Kripalani S, Amin AN. Preparing for “diastole”: advanced training opportunities for academic hospitalists. J Hosp Med. 2006;1(6):368–377 [DOI] [PubMed] [Google Scholar]
- 5. Josephson SA, Engstrom JW, Wachter RM. Neurohospitalists: an emerging model for inpatient neurological care. Ann Neurol. 2008;63(2):135–140 [DOI] [PubMed] [Google Scholar]
- 6. Likosky D, Shulman S, Restrepo L, Freeman WD. Survey of neurohospitalists: subspecialty definition and practice characteristics. Front Neurol. 2010;1:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Academy of Neurology: Neurohospitalist Section. http://www.aan.com/go/about/sections/neurohospitalist Accessed June 20, 2012.
- 8. Likosky DJ, Josephson SA, Coleman M, Freeman WD, Biller J. Survey of current neurohospitalist practice. Neurol Clin Pract. 2012;2(4):319–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barrett KM, Fowler MV. Is fellowship training necessary for neurohospitalists? Neurohospitalist. 201. 1;1:125–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fellowship and Residency Electronic Interactive Database, author. https://freida.ama-assn.org/Freida/ Accessed October 10, 2011.
- 11.List of ACGME Accredited Programs and Sponsoring Institutions. , author. http://www.acgme.org/adspublic/ Accessed January 25, 2012.
- 12. Vasilevskis EE, Knebel RJ, Wachter RM, Auerbach AD. California hospital leaders' views of hospitalists: meeting needs of the present and future. J Hosp Med. 2009;4(9):528–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Society of Hospital Medicine FAQ. http://www.hospitalmedicine.org/AM/Template.cfm?Section=FAQs&Template=/FAQ/FAQListAll.cfm Accessed January 9, 2013.
- 14. Adornato BT, Drogan O, Thoresen P, et al. The practice of neurology, 2000-2010: report of the AAN Member Research Subcommittee. Neurology. 2011;77(21):1921–1928 [DOI] [PubMed] [Google Scholar]
- 15. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72 e71–72 e77. [DOI] [PubMed] [Google Scholar]
- 16. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314–318 [DOI] [PubMed] [Google Scholar]
- 17. Buser M. Hospitalist programs in the age of healthcare reform. J Healthc Manag. 2010;55(6):378–380 [PubMed] [Google Scholar]
- 18. Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004–2010 [DOI] [PubMed] [Google Scholar]
- 19. Fernandez A, Grumbach K, Goitein L, Vranizan K, Osmond DH, Bindman AB. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160(19):2902–2908 [DOI] [PubMed] [Google Scholar]
- 20. Hunter AJ, Desai SS, Harrison RA, Chan BK. Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79(1):78–82 [DOI] [PubMed] [Google Scholar]
- 21. Daru JA, Holmes A, Starmer AJ, Aquino J, Rauch DA. Pediatric hospitalists' influences on education and career plans. J Hosp Med. 2012;7(4):282–286 [DOI] [PubMed] [Google Scholar]
- 22. Douglas VC, Scott BJ, Berg G, Freeman WD, Josephson SA. Effect of a neurohospitalist service on outcomes at an academic medical center. Neurology. 2012;79(10):988–994 [DOI] [PubMed] [Google Scholar]
- 23. Meltzer D. Hospitalists and the doctor–patient relationship. J Legal Stud. 2001;30(2):589–606 [DOI] [PubMed] [Google Scholar]
- 24. Fletcher KE, Sharma G, Zhang D, Kuo YF, Goodwin JS. Trends in inpatient continuity of care for a cohort of Medicare patients 1996-2006. J Hosp Med. 2011;6(8):438–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Goodrich K, Krumholz HM, Conway PH, Lindenauer P, Auerbach AD. Hospitalist utilization and hospital performance on 6 publicly reported patient outcomes. J Hosp Med. 2012;7(6):482–488 [DOI] [PMC free article] [PubMed] [Google Scholar]