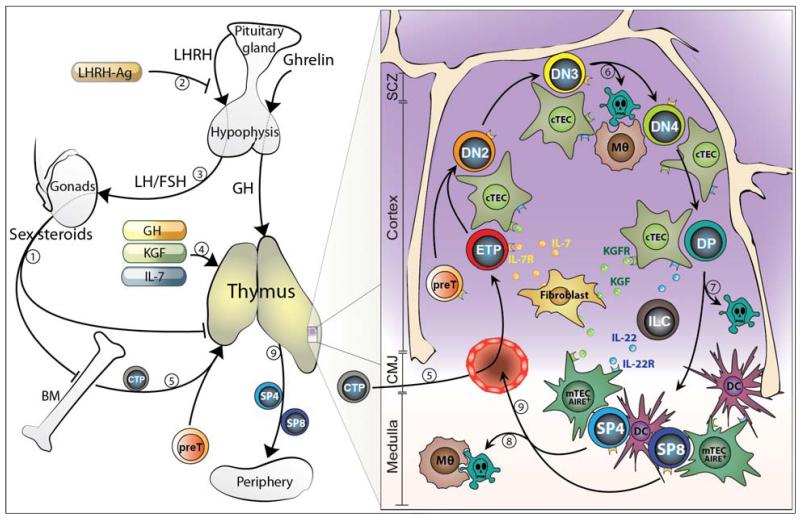
Figure 1. Overview of steady-state thymopoiesis in addition to therapeutic strategies currently in clinical trials to enhance thymic recovery after HSCT.
The increase in sex steroids during life is generally thought to progressively impair BM and thymic lymphopoiesis (1). SSA using a LHRH-Ag (2) (that blocks the upstream signals stimulating sex steroid production (3)) reverses the age-related decline in BM and thymic function and promotes their rejuvenation. Similarly, therapeutic administration with GH, KGF or IL-7 promotes the regeneration of T cell lymphopoiesis (4). The process of thymopoiesis begins when circulating BM-derived T-lineage progenitors (CTP) seeds the thymus in the cortico-medullary junction (CMJ) (5) and undergo a series of well-defined maturation steps. This all occurs under the guidance and close interaction with the thymic stromal microenvironment; which is comprised of cTEC, mTEC, fibroblasts, macrophages (Mθ) and DC, and which provide survival, differentiation and homing factors to the developing thymocytes. Approximately 95% of thymocytes produced daily die during the process of beta-selection (6), positive selection (7) and negative selection (8) by apoptosis, which results in the generation of self-restricted and self-tolerant naïve CD4+ and CD8+ T cells (SP4 and SP8) (8). Several intrathymic factors have been shown to be important for endogenous T cell regeneration and may have some therapeutic benefit including IL-7, KGF and IL-22. SCZ (Sub-capsular zone), ILC (Innate lymphoid cells)