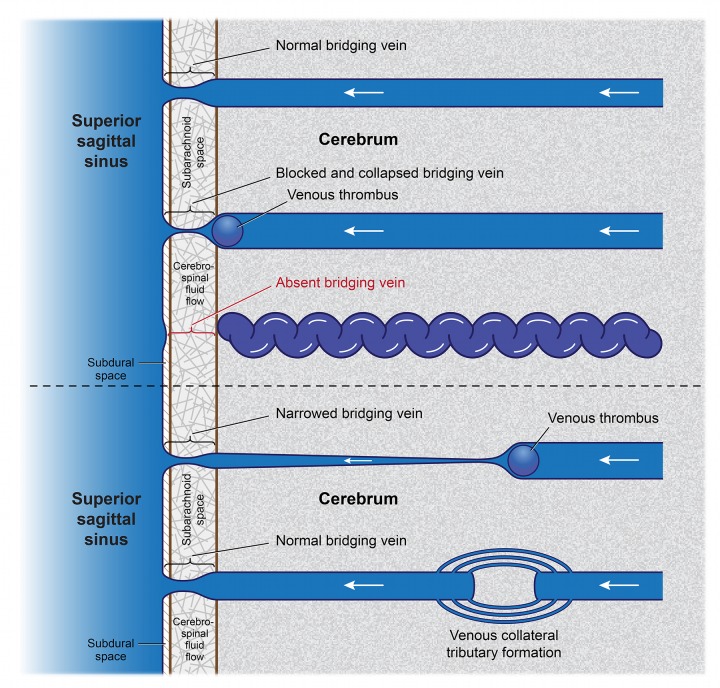
FIGURE 18.
Specificity of venous response according to site of cerebral occlusive thrombus. Top vein: Normal unoccluded superficial cerebral vein passes through the leptomeninges (pia mater and arachnoid) to bridge the space from brain to the dural sinuses. Variable “pinching” of the bridging portion of the vein occurs in response to the surrounding varying cerebrospinal fluid pressure as part of a Starling resistor mechanism to regulate intraluminal venous pressure. Second vein: A venous thrombus that develops and lodges outside the cerebral tissue can obstruct venous flow. Decreased venous flow can cause a collapse of the thin-walled bridging portion of the vein. Third vein: During embryological development, an absence of blood flow can quickly precipitate apoptosis of the bridging portion of the vein along with its disappearance. Since there are no microscopic anastomotic venous channels in the subarachnoid space filled with moving cerebrospinal fluid, collateral venous channels to bypass the obstruction cannot form. Over time, the vein distal to the occlusion, along with its leptomeningeal portion, becomes engorged and tortuous, with higher pressure and deoxygenated cyanotic blood within. Fourth vein: Fibrin clots that may block the venous lumen more distally within cerebral tissue may also cause narrowing of the immediate proximal portion of the vein and cause apoptosis of a venous segment. However, smaller tributary channels continue to feed into the vein more proximally, preserving venous integrity and maintaining a reduced flow into the dural sinus. Bottom vein: Over time, enlargement of otherwise microscopic channels that exist within fixed cerebral substrate, and/or persistence of fetal vasculature can allow for distributory and tributary venous collateral formation to bypass the site of the original thrombus and renormalize blood flow in the proximal vein.