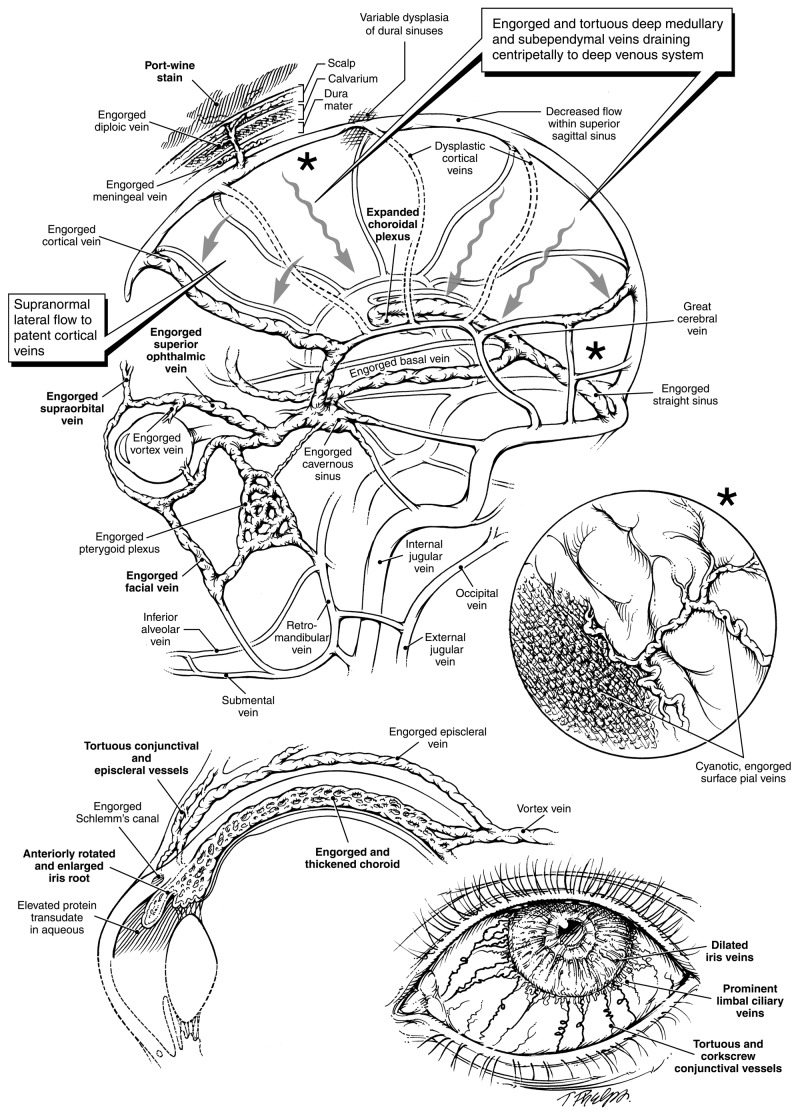
FIGURE 8.
The Sturge-Weber syndrome: dysplasia of cortical veins creates alternative cerebral venous outflow passageways. (Boldfaced letters indicate engorged vessels clinically visible or readily detectable by MRI.) Top left, Superficial cortical veins normally drain blood from brain cortex via bridging segments into the dural sinuses. Absence or dysplasia of these veins will obstruct the flow of venous blood and cause engorgement of surface pial vessels (see insert top right). Rather than draining centrifugally, cortical venous blood will be forced to flow centripetally through deep brain tissue. Remaining cortical veins will conduct supranormal bloodflow. Particularly if there is any dysplasia of the dural venous sinuses, dural sinus pressures may be raised segmentally, also impeding venous drainage from the scalp, consequently also producing port-wine stains visible within the skin. Cortical blood will be forced into the deep venous system via expanded medullary and subependymal veins. The resulting higher pressure in the deep system considerably expands the choroidal plexus, which is linked to the great cerebral vein and the straight sinus, and ultimately joins the cavernous sinus via an engorged basal vein. High cavernous sinus pressures, in turn, impede the normal drainage of orbital and ocular blood, with consequences shown at bottom left and bottom right. Since normal drainage of blood from the face into the orbit is also impeded, this produces the periocular and upper facial port-wine stains characteristic of the Sturge-Weber syndrome. Venous drainage of the mandible occurs via the inferior alveolar and submental veins which do not have any direct connection to the brain. Unless neck veins are also dysplastic, mandibular port-wine stains alone do not occur as part of the syndrome. Middle right insert, Engorgement of surface pial vessels. The obstructed flow of deoxygenated blood with pressure elevation renders a cyanotic appearance to expanded vessels with “angiomatosis” appearance. Bottom left, Restricted outflow from an expansile ocular choroid causes diffuse thickening, much as for the choroidal plexus in the brain. The thickened choroid, in turn, may rotate the iris root forward. In a geometrically smaller eye, this may give the appearance of goniodysgenesis and cause obstruction of the trabecular meshwork and aqueous outflow passages. Elevated intraluminal venous pressures will also cause transudation of protein into the aqueous fluid, which can also block outflow passages. Bottom right, Engorged and tortuous conjunctival and episcleral vessels are often apparent, as may be engorged iris vessels. Corkscrewing venous tortuosity, often visible in older affected individuals, is pathognomonic for an elevated transluminal venous pressure gradient.