Abstract
Background: Data for osteoporotic hip fractures in Greece is limited and little is known upon the meaning of family support during the postoperative/rehabilitation period.
Objective: To identify the factors influencing the mortality after hip fractures in the elderly, the effect of rehabilitation and family support in the post-fracture course, and the impact of these fractures on the family of the injured elderly.
Methods: We conducted an observational study of 218 consecutive patients older than 60 years of age, who underwent surgical management of a unilateral hip fracture at a tertiary hospital of Central Greece, with follow-up contacts at 30 days, 3 months and one year. Demographic characteristics, pre- and post-fracture residential and functional status, assessment of basic activities of daily living (ADL), co-morbidities, type and mechanism of fracture and hospitalization data as well as the modification of activities of the patients’ relatives were recorded.
Results: Fifteen patients (6.9%) died during hospitalization; thirty-nine (17.9%) died within one year of fracture. The factors that were predictive of in-hospital, 30-days and one-year mortality, based on multivariate analysis, were male sex, advanced age >85 and Charson index >3. There was a significant association between delayed surgery (>48 hours) and increased in-hospital mortality. The percentage of patients assessed as ADL A or B at baseline, decreased form 84% preoperatively to 50.4% one year postoperatively. Only one-third of patients walking without aid before the fracture returned to the previous state. Family members modified their activities in 48% of cases to assist their relatives with a hip fracture.
Conclusions: One-year mortality in patients with hip fractures was 17.9%. Surgical delay (>48 hours) increased in-hospital mortality. Comorbidities >3, male sex, and advanced age increased the risk of in-hospital and post-discharge mortality during the 1st year. Twelve months postoperatively, half of patients walking without aid before the fracture returned to the previous state. Despite the beneficial effect of family support, the lack of organized rehabilitation programs and geriatric units are potential negative factors for patients’ functional outcome. In addition, 48% of patients’ relatives changed their daily activities to assist their relatives.
Keywords: Hip fractures, one-year mortality, risk factors, rehabilitation, family support
Introduction
Hip fractures are a major cause of illness, disability and death in the elderly people, with an incidence increasing with age1,2. Because the world’s population is aging, the frequency of hip fractures is increasing by 1-3% per year1 in most areas of the world. Approximately 1.66 million hip fractures per year worldwide were reported in 19902. According to the epidemiologic projections, this worldwide annual number will rise to 6.26 million by the year 20502. The growth of population will be more marked in Asia, Latin America, Middle East and Africa than in Europe and North America, and it is in the former regions that 70% of the fractures will occur. Lifetime risk for sustaining a hip fracture is estimated at 16-18% in white women and 5-6% in white men2-4. In European and American countries the annual incidence is higher for women and ranges from 80.9 fractures/100,000 person-years for females and 51.1/100,000 person-years for males to 1.1% for females and 0.7% for males over 70 years of age 2,5-7. In Greece, the incidence of hip fractures increased from 107.3/100,000 inhabitants before 1992 to 118.6/100,000 inhabitants in 19978,9, and this increase was mainly due to the aging of the population.
Excess mortality following a hip fracture has been shown in many studies10-17, with one year mortality rates varying between 10% and 45%8,12,15,18-21. According to a recent study from southwestern Greece, the mortality rate during the 1st year after a hip fracture was 15.7%8. Similar findings for the Greek population were reported in a study from the urban area of Athens (mortality rate of 18%)21and from the rural area of Crete (mortality rates of 17% for women and 23% for men)8. Although the mortality and morbidity rates in the Greek population are comparable to the ones reported in international studies, there is lack of evidence concerning the residential status before and after the fracture as well as the rehabilitation and the impact of family support in the postoperative period.
The purpose of our study is to identify the factors influencing the mortality after osteoporotic hip fractures and among them the effect of rehabilitation and family support in the post-fracture course. This study also aims at elucidating the impact of these fractures on the family of the injured elderly.
Patients and methods
Two hundred and sixty-one patients older than 60 years who sustained a hip fracture were admitted in the Department of Orthopaedic Surgery of a University Hospital in a period of 3 years. The hospital serves an urban-rural population of 1,000,000 inhabitants and was on call 10 days/month during the study period.
Patients with pathological fractures, previous hip fractures, fractures caused by high energy trauma or patients who were treated nonoperatively due to increased perioperative risk or their own wish were excluded from the study (n = 43).
Finally 218 patients (78 men and 140 women) were enrolled in the study and followed for a period of one year or until death, if it occurred during the follow-up period.
Study design and data collection
The study design was prospective, with follow-up contacts at 30 days and 3 months postoperatively in the outpatient clinic of the Department of Orthopaedic Surgery, and at 12 months postoperatively through telephone communication.
Demographic characteristics, pre-fracture residential and functional status data, co-morbidities, type and mechanism of fracture and hospitalization data (time from admission to surgery, type of anesthesia, fixation material, blood units transfused, pre- and postoperative morbidity, time from admission to discharge and in-hospital mortality) were recorded.
To assess comorbidity the Charlson comorbidity index was calculated for each patient22. Patients with comorbidities were dichotomized into those with zero, 1, or 2 conditions versus those with 3 or more comorbidities. Operative delay was defined as surgery more than 48 hr (> 48 hr) after admission.
The Katz ADL (Activities of Daily Living) index is based on an evaluation of the functional dependence or independence of patients in bathing, dressing, going to the toilet, transferring, continence, and feeding. ADL index A indicates independence in all six functions, index B independence in all but one of the six functions. Indexes C–G indicate dependence in bathing and at least one additional function23-24.
Walking ability was based on the patient’s need for walking aids and was categorised as no need for a walking aid, need for a stick or crutches, need for a walking frame or non-ambulant.
Living conditions were categorised as independent (living alone/with relatives) or dependent (living with relatives/ in a nursing home).
Residence was determined as urban/semi-urban and rural on the basis of the 2001 census25.
Finally, the modification of the daily activities of the patients’ relatives in order to aid, comfort and facilitate the patients was graded and recorded.
Statistics
Normally distributed variables are shown as mean (SD) and differences between groups were analysed using unpaired Student t-tests. Categorical variables are shown as proportions and the differences were analysed using chi-square tests. Odds ratios (ORs) were calculated for the predictors of in-hospital mortality 30-day and 12 months mortality using logistic regression analysis. All statistical analyses were performed using the SPSS software program for Windows (SPSS 17.0, Chicago, IL). Any p-values less than 0.05 were considered statistically significant.
Results
Demographics (Table 1)
Table 1. Characteristics of participants.
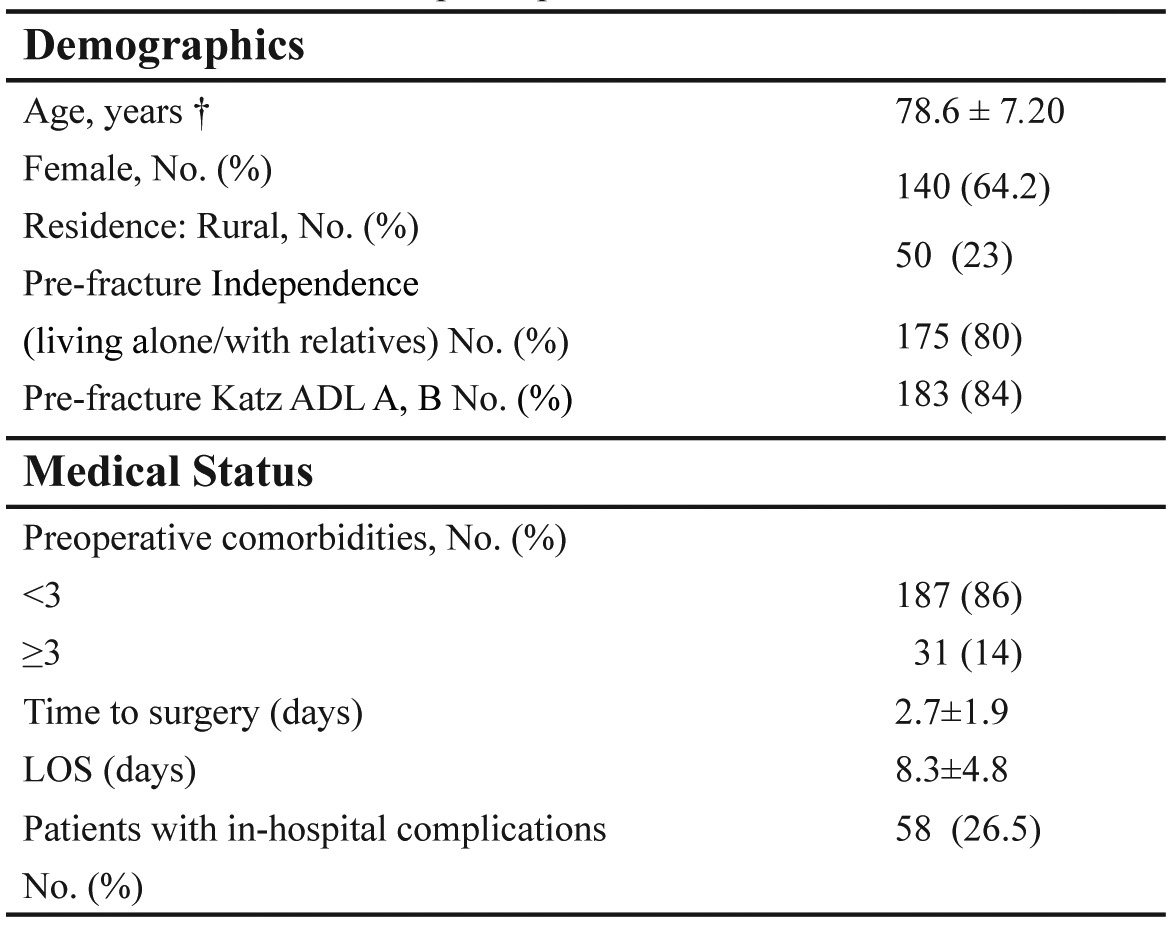
† Values are means (SD). LOS: length of stay, Katz ADL: The Katz Index of Independence in Activities of Daily Living
The mean age was 78.6 years and 64.2% of the patients were female. Mean age of women was 78.4 (SD 7.6) and of men 78.8 (SD 7.7, p=0.412).
The vast majority (80%) were independent, living alone or with relatives, in an urban or semi-urban area (77%).
Eighty four per cent were assessed as ADL A or B (independent in all six functions of ADL or in all but one). Fifty per cent were independent walkers without walking aids and 16% of the patients used a walking frame.
At admission, 52 of 218 patients (24%) had no comorbid conditions, 135 (62%) had 1-2, and 31 patients (14%) had 3 or more comorbidities.
Surgical characteristics (Table 1)
The mean time from admission to surgery was 2.7 days ± 1.85 (range 0-13), and 45.9% of patients were operated within 48 hours of admission. Cessation of anticoagulant medication to avoid excessive bleeding and for security during spinal/epidural anesthesia was the main reason for surgical delay. In total 63 of 218 patients (29%) received anticoagulation before the fracture: 23 patients received aspirin, 32 patients received clopidogrel, and 8 patients received acenocumarol. The delay to surgery for these patients ranged from 4 to 9 days.
The average hospital stay was 8.3 days ± 4.8 (range, 4-27 days).All patients but one (with a concomitant elbow fracture) were operated on under spinal or epidural anesthesia.
Regarding to the type of the fracture, 40 patients (64%) sustained an intertrochanteric fracture, 13 (6%) a subtrochanteric fracture and 65 (30%) a subcapital fracture. Thirteen patients (6%) suffered a concomitant Colle’s, proximal humerus or elbow fracture. Inter- and subtrochanteric fractures were treated either with intramedullary nail (IMN, n=90) or dynamic hip screw (DHS, n=63), and subcapital fractures were treated with hemi- (n=53) or total hip arthroplasty (n=12).
Twenty-two percent of patients received a blood transfusion of 2 or more units of condensed erythrocytes intra- and/or postoperatively. The majority of patients (41/63) receiving pre-fracture anticoagulation with aspirin, clopidogrel, acenocumarol required blood transfusion of 2 or more units.
Prophylactic antibiotics were administered to all patients preoperatively (1 dose) and for 1-2 days postoperatively, while low molecular weight heparin (LMWH) was administered for 30 days postoperatively. Individuals under anticoagulation before the fracture resumed their previous treatment 5 days postoperatively, and were covered with LMWH during the aforementioned interval.
During hospitalization 15 out of 218 patients (6.9%) died because of cardiac event, pulmonary embolism and fatal stroke.
Fifty-four of the remaining 203 patients (26.6%) developed a major medical complication. The most frequent major complications were infections (wound, respiratory and urinary tract), postoperative delirium, deep venous thrombosis and aggravation of a pre-existing morbidity (congestive heart failure, renal failure, respiratory impairment, serum glucose deregulation).
Fifty-four of the 203 patients (26.6%) developed a major medical complication. The most frequent major complications were infections (wound, respiratory and urinary tract), postoperative delirium, deep venous thrombosis and aggravation of a pre-existing morbidity (congestive heart failure, renal failure, respiratory impairment, serum glucose deregulation).
Mortality
After discharge, there were 10 deaths within 30 days (4.6%). In total, 39 deaths occurred within the study period (17.9%). In addition, 40 patients (18.3%) were either lost to follow-up or declined the interview.
In-hospital mortality was found to be higher for men than for women (11.5% versus 4.3%, p<0.01). The higher mortality rate among men persisted after 1 year (32.1 % versus 10%, p<0.001).
In addition, in-hospital mortality increased from 4.3% for those with Charson index less than three to 22.6% for those with Charlson index of greater than three.
The multivariate analysis using logistic regression showed that for in-hospital mortality, there was a significant change in mortality rate for advanced age >85 (OR=2.88; 95% CI 1.20-5.81), male sex (OR =2.90; 95% CI 2.10-3.09), and Charson index >3 (OR=3.21; 95% CI 1.97-4.2)
We found similar results for 30-days and 12-months mortality rates (Table 2).
Table 2. Logistic regression analyses [odds ratio (OR) and 95% confidence interval (CI)] for in- hospital, 30-days, and 12-months mortality.*.

*Each variable presented is adjusted for the others
Surgery was delayed for three or more days in more than 30% of patients with hip fractures. There was a significant association between delayed surgery >48h and increased in-hospital mortality. However, pre-fracture anticoagulation did not influence significantly the mortality. After adjusting for age, sex, and comorbidities, the risk of in-hospital death increased with surgical delay (OR 1.83; 95% CI 1.10–3.50). However, the mortality rates at 30 days (OR 1.19; 95% CI 0.90-1.42) and at one year (OR 1.26; 95% CI 0.88-1.58) were not associated with delayed surgery. Logistic regression analysis also indicated that after controlling for main patients risk factors (age, sex, comorbidities, and delay to surgery) there was no significant association between outcome (mortality rates) and fracture type and thus type of surgical procedure.
Rehabilitation
The patients were mobilized the second postoperative day according to a standardized protocol, unless the treating surgeon suggested otherwise in cases of unstable fixation.
After discharge, 32% of the individuals were further treated/rehabilitated in nursing or intermediate care facilities for 2-4 weeks, 7% received physical therapies at home and 61% had no rehabilitation at all.
Functional outcome
The functional status of the subgroup of patients who completed the one-year follow-up (N=139) is presented.
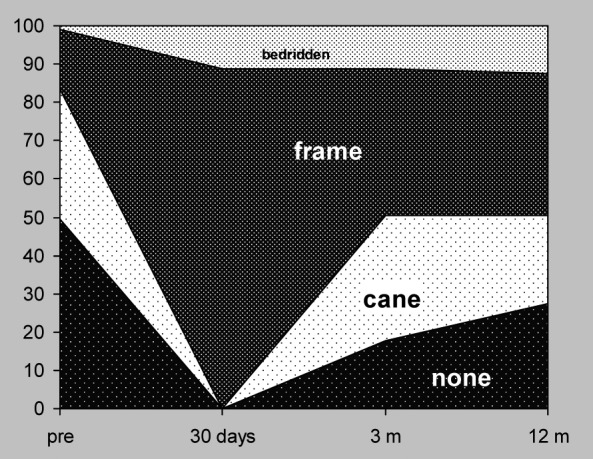
As shown at Figure 1, post fracture assessment indicated a substantial decline in functional status. Before injury, 50% of patients (69/139) walked without aid, 34% of patients (47/139) walked with a cane, 16% of patients (22/139) walked with a frame and one patient (1/139) was bedridden. Twelve months postoperatively, 27% of patients (38/139) walked without aid, 23% of patients (32/139) required a cane, 37% of patients (51/139) required a walking frame, and 12.6% of patients (18/139) were bedridden.
Figure 1. Walking ability at each follow-up, of the subgroup of 139 patients that concluded the postoperative period of 1 year.
Assessment of basic activities of daily living (ADL) indicated that 87% of patients (121/139) were assessed as ADL A or B (independent in all six functions of ADL or in all but one) at baseline. After 12 months 50% of patients (70/139) recovered ADL to level A or B (Figure 2).
Figure 2. Katz ADL A, B and independence (living alone/with relatives) pre- and at 12 months postoperatively, of the subgroup of 139 patients that concluded the postoperative period of 1 year.

Before injury, 83% of patients (115/139) were able to live independent (alone or with relatives) but only 29.5% (41/139) were living independent 12 months later. Two per cent of patients (3/139) were instituted and completely dependent on nursing staff (Figure 2).
Discussion
In our study, the overall mortality during the 1st year after a hip fracture was 18%. Similar findings were also reported in the Greek literature8,21, although fracture registries are poor in Greece and therefore data about mortality after hip fractures are inadequate. One-year mortality rates in Europe range between 19% and 33%: Spain 22.5%18, Italy 23%26, Sweden 22%27, Norway 21%18, Denmark 19-22%28and UK29. Studies from the United States report lower one-year mortality rates, ranging from 12.7%30 to14%31. Lower rates are also reported in two studies from Sweden (10.6%15and 14%31), which however include younger patients (mean age 73.3 years). Finally, our in-hospital mortality rate (6.8%) was higher compared to 1.6%-5% from USA series30,32-34.
There is a 3-fold mortality rate in men than in women in our study (32.1 % vs10 %) although there was no mean age difference between genders (78.8 for males and 78.4 for females). Although this difference confirms the worldwide knowledge of increased male mortality after hip fractures15,17,20, this discrepancy is less pronounced in other studies. A study from Denmark17 suggested that the cumulative one-year mortality rate after a hip fracture was 37.1% for men and 26.4% for women, despite the lower age of men at the time of the injury.
Next to male gender and age, poorly regulated medical conditions are directly related to increased mortality after hip fractures14,16,31,32,35. In our study, patients with 3 or more comorbidities were more than twice likely to die, as compared to those with none or 1-229,30. Elderly from the groups with none or 1-2 comorbidities had an equal mortality rate (20%) during the 1st year.
Delay in surgical treatment of a hip fracture can be caused by numerous factors, which range from the time required to stabilise a patient’s medical condition and the cessation of anticoagulant medication received prior to the fracture to the availability of blood banks to cover a potential surgery. Regardless of the cause, surgical delay increases the time a patient spends in bed and may adversely affect their nutritional status and the eventual outcome. In our study significant delay to surgery was noted in the subgroup of patients that received anticoagulation prior to the surgery. The same group of patients required in their majority transfusion of more than 2 units of condensed erythrocytes.
The effect of surgical delay on mortality has been studied over 2 decades. A systematic review and meta-analysis of 16 observational studies published in an anaesthesiology journal found that operative delays of more than 48 hours were associated with an increased risk of 30-day and one-year mortality36. Another recent review showed that there are a number of reports in the literature suggesting the beneficial effect of early surgery on improvement of short-term mortality, while other studies have not found any effect of early surgery, so no conclusion was drawn37. In our study the risk of death in hospital, increased with surgical delay more than 48 h, however the statistical significance of surgical delay in mortality rates disappeared at 30 days and one year postoperatively.
Regarding the functional capacity, only 18% of our patients walked independently 12 months after the fracture and only one of three patients (35%) who walked free of assistance before the fracture managed to reach the pre-fracture mobility level one year postoperatively. Our findings on walking ability one year after fracture are worse than the ones reported in the literature21,38,39. Pre-fracture mobility level was achieved from 41 to 48% of patients in various studies14,19,34. Considering that only 39% of our patients followed a rehabilitation program by specialized therapists after discharge, the decreased walking independency is an expected consequence. In fact, the majority of our patients had a decrease of functional status of at least one level (e.g. from independency to cane, from cane to frame or from frame to bed confinement). In a review of studies that examined the effectiveness of physical activity counseling, Tullogh et al39 found a significant increase in physical activity and mobilization of the elderly in all provider categories, pointing out the significance of rehabilitation under expert surveillance. Recent data from Bentler et al32, examining the consequences of hip fracture with regard to post-hospital lodging, functional status and mortality, showed that 58% of the patients were discharged to a nursing facility and preserved their mobility status in 44% at one-year follow-up.
The vast majority of patients of the present series (87%) lived with their relatives before their fracture; either in the same apartment or building, or sharing a common yard in a rural residency. This mirrors the traditional strong bonds of the Greek families, especially in the rural and semi-urban regions, by means of in-house support of the aged relatives instead of their discharge to elderly-facilities. In contrast to data from other countries40 where 42% of the patients came to the hospital from an institution, only 2% of the elderly of the present series lived in an institution or a nursing facility before their injury. The 4-month mortality rate in the aforementioned study was 20% similar to the one-year follow-up findings of our study.
One year after their discharge, 92% of the living patients continued living with their relatives, but only one third managed to accomplish their daily activities without help. The percentage of the patients living with relatives and dependent on them, more than doubled after the fracture, pointing out the significance of family support for the survival and well-being of these patients, whereas only 2% of the elderly continued living completely dependent in an institution one year after their discharge. In a study from New Zealand 88% of the patients discharged home remained there one year after fracture, and 65.6% of them were independent19.
The requirements of elderly people living with relatives after a hip fracture and the way this affects the latters’ personal, professional and social lives, is not adequately studied in literature. In our study, in almost one half of the cases, relatives of the patients-usually their children- changed their daily activities, lost hours from work and/or leisure, and modified their household in order to facilitate the living conditions, and the mobilization of their relatives.
Mortimore et al41, studied the association between social contact and mortality after hip fracture in elderly patients. They found that participants, who had no contact with family members prior to the fracture, were twice as likely to die in comparison to those who communicated daily before the fracture. Ceder42 reported that living with someone was a determining factor for the success of rehabilitation after a hip fracture and increases the possibility of remaining at their home and not institutionalized, one year after the fracture.
Conclusions
One-year overall mortality after a hip fracture was 18%. There was an independent relationship between surgical delay >48 h and in-hospital mortality. Comorbidities >3, male sex, and advanced age >85 years increase the risk of in-hospital and post-discharge mortality during the 1st year.
Twelve months postoperatively, only half of patients walking without aid before the fracture returned to the previous state and 29.5% were living independent.
Despite the beneficial effect of family support, the lack of organized rehabilitation programs and geriatric units are potential negative factors for patients’ functional outcome. In addition, in half of the cases, patients’ relatives changed their daily activities, lost hours from work and/or leisure, and modified their household in order to facilitate the living conditions, and the mobilization of their relatives.
Conflict of interest
No conflict of interest.
Acknowledgements
Part of this study, entitled ‘Hip fractures in elderly patients’, with authors Michalitsis S, Dailiana Z, Karamanis N, Malizos K, Papakostidou I, Varitimidis S, was presented (oral presentation) at the 10th Congress of the European Federation of National Associations of Orthopaedics and Traumatology (EFORT), in Vienna, AUSTRIA, in June 2009.
References
- 1.Cummings SR, Melton U. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 2.Kannus P, Parkkari J, Sievänen H, Heinonen A, Vuori I, Järvinen M. Epidemiology of hip fractures. Bone. 1996;18:57S–63S. doi: 10.1016/8756-3282(95)00381-9. [DOI] [PubMed] [Google Scholar]
- 3.Melton LJ 3rd, Therneau TM, Larson DR. Long-term trends in hip fracture prevalence: the influence of hip fracture incidence and survival. Osteoporos Int. 1998;8:68–74. doi: 10.1007/s001980050050. [DOI] [PubMed] [Google Scholar]
- 4.Meunier PJ. Prevention of hip fractures. Am J Med. 1993;95:75S–78S. doi: 10.1016/0002-9343(93)90387-5. [DOI] [PubMed] [Google Scholar]
- 5.Hochberg MC, Williamson J, Skinner EA, Guralnik J, Kasper JD, Fried LP. The prevalence and impact of self-reported hip fracture in elderly community-dwelling women: the Women’s Health and Aging Study. Osteoporos Int. 1998;8:385–389. doi: 10.1007/s001980050079. [DOI] [PubMed] [Google Scholar]
- 6.Scottish Intercollegiate Guidelines Network (SIGN). Prevention and management of hip fractures in older people. SIGN Publication No 56, SIGN, Edinburgh. 2009 [Google Scholar]
- 7.Leslie WD, O’Donell S, Jean S, Lagacé C, Walsh P, Bancej C, et al. Trends in hip fracture rates in Canada. JAMA. 2009;302:883–889. doi: 10.1001/jama.2009.1231. [DOI] [PubMed] [Google Scholar]
- 8.Karagiannis A, Papakitsou E, Dretakis K, Galanos A, Megas P, Lambiris E, et al. Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten year follow-up with reference to the type of fracture. Calcif Tissue Int. 2006;78:72–77. doi: 10.1007/s00223-005-0169-6. [DOI] [PubMed] [Google Scholar]
- 9.Paspati I, Galanos A, Lyritis GP. Hip fracture epidemiology in Greece during 1977-1992. Calcif Tissue Int. 1998;62:542–547. doi: 10.1007/s002239900476. [DOI] [PubMed] [Google Scholar]
- 10.Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization and functional status: a prospective study. Am J Public Health. 1997;87:398–403. doi: 10.2105/ajph.87.3.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elmerson S, Zetterberg C, Andersson GB. Ten year survival after fractures of the proximal end of the femur. Gerontology. 1988;34:186–191. doi: 10.1159/000212951. [DOI] [PubMed] [Google Scholar]
- 12.White BL, Fisher WD, Laurin CA. Rate of mortality for elderly patients after fracture of the hip in the 1980’s. J Bone Joint Surg Am. 1987;69:1335–1340. [PubMed] [Google Scholar]
- 13.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 14.Holt G, Macdonald D, Fraser M, Reece AT. Outcome after surgery for fracture of the hip in patients aged over 95 years. J Bone Joint Surg Br. 2006;88:1060–1064. doi: 10.1302/0301-620X.88B8.17398. [DOI] [PubMed] [Google Scholar]
- 15.Farahmand BY, Michaëlsson K, Ahlbom A, Ljunghall S, Baron JA. Swedish Hip Fracture Study Group. Survival after hip fracture. Osteoporos Int. 2005;16:1583–1590. doi: 10.1007/s00198-005-2024-z. [DOI] [PubMed] [Google Scholar]
- 16.Pande I, Scott DL, O’Neill TW, Prichard C, Woolf AD, Davis MJ. Quality of life, morbidity and mortality after low trauma hip fracture in men. Ann Rheum Dis. 2006;65:87–92. doi: 10.1136/ard.2004.034611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–390. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alegre-López J, Cordero-Guevara J, Alonso-Valdivielso JL, Fernández-Melón J. Factors associated with mortality and functional disability after hip fracture: an inception cohort study. Osteoporos Int. 2005;16:729–736. doi: 10.1007/s00198-004-1740-0. [DOI] [PubMed] [Google Scholar]
- 19.Thwaites J, Mann F, Gilchrist N, McKie J, Sainsbury R. Older patients with hip fractures: evaluation of a long-term specialist orthopedic medicine service in their outcomes. N Z Med J. 2007;120:U2535. [PubMed] [Google Scholar]
- 20.Forsén L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10:73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 21.Stavrou ZP, Erginousakis DA, Loizides AA, Tzevelekos SA, Papagiannakos KJ. Mortality and rehabilitation following hip fracture. A study of 202 elderly patients. Acta Orthop Scand Suppl. 1997;275:89–91. doi: 10.1080/17453674.1997.11744754. [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 24.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 25.Population. CONCISE statistical yearbook 2009. Hellenic Statistical authority-ELSTAT, Piraeus. 2010:35–58. [Google Scholar]
- 26.Olmeda A, Greco F, Timar J, Malgaroli E. Death rate in patients submitted to surgical treatment of fractures of the proximal femur. Chir Organi Mov. 1995;80:179–181. [PubMed] [Google Scholar]
- 27.Svensson O, Strömberg L, Ohlén G, Lindgren U. Prediction of the outcome after hip fracture in elderly patients. J Bone Joint Surg Br. 1996;78:115–118. [PubMed] [Google Scholar]
- 28.Schrøder HM, Erlandsen M. Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 2.5-18.5 years. J Orthop Trauma. 1993;7:525–531. doi: 10.1097/00005131-199312000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Chesser TJ, Handley R, Swift C. New NICE guideline to improve outcomes for hip fracture patients. Injury. 2011;42:727–729. doi: 10.1016/j.injury.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Aharanoff GB, Koval J, Skovron ML, Zuckerman JD. Hip fractures in the elderly: predictors of one year mortality. J Orthop Trauma. 1997;11:162–165. doi: 10.1097/00005131-199704000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Kenzora JE, McCarthy RE, Lowell JD, Sledge CB. Hip fracture mortality: relation to age, treatment, preoperative illness, time of surgery and complications. Clin Orthop Relat Res. 1984;186:45–56. [PubMed] [Google Scholar]
- 32.Ekström W, Németh G, Samnegård E, Dalen N, Tidermark J. Quality of life after a subtrochanteric fracture: a prospective cohort study on 87 elderly patients. Injury. 2009;40:371–376. doi: 10.1016/j.injury.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 33.Bentler SE, Liu L, Obrisan M, Cook EA, Wright KB, Geweke JF, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol. 2009;170:1290–1299. doi: 10.1093/aje/kwp266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, et al. Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA. 2001;285:2736–2742. doi: 10.1001/jama.285.21.2736. [DOI] [PubMed] [Google Scholar]
- 35.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995;310:150–159. [PubMed] [Google Scholar]
- 36.Shiqa T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality after hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 37.Leung F, Lau TW, Kwan K, Chow SP, Kung AW. Does timing of surgery matter in fragility hip fractures? Osteoporos Int. 2010;21:S529–S534. doi: 10.1007/s00198-010-1391-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong MK, Arjandas , Ching LK, Lim SL, Lo NN. Osteoporotic hip fractures in Singapore--costs and patient’s outcome. Ann Acad Med Singapore. 2002;31:3–7. [PubMed] [Google Scholar]
- 39.Fortier M, Tulloch H, Hogg W. A good fit: integrating physical activity counselors into family practice. Can Fam Physician. 2006;52:942-944–947-949. [PMC free article] [PubMed] [Google Scholar]
- 40.van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: outcomes for function, quality of life and type of residence. Clin Orthop Relat Res. 2001;390:232–243. [PubMed] [Google Scholar]
- 41.Mortimore E, Haselow D, Dolan M, Hawkes WG, Langenberg P, Zimmerman S, et al. Amount of social contact and hip fracture mortality. J Am Geriatr Soc. 2008;56:1069–1074. doi: 10.1111/j.1532-5415.2008.01706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ceder L. Predicting the success of rehabilitation following hip fractures. Disabil Rehabil. 2005;27:1073–1080. doi: 10.1080/09638280500056436. [DOI] [PubMed] [Google Scholar]


