Abstract
Introduction
The effect of dexmedetomidine on length of intensive care unit (ICU) stay and time to extubation is still unclear.
Materials and Methods
Pertinent studies were independently searched in BioMedCentral, PubMed, Embase, and the Cochrane Central Register of clinical trials (updated February first 2013). Randomized studies (dexmedetomidine versus any comparator) were included if including patients mechanically ventilated in an intensive care unit (ICU). Co-primary endpoints were the length of ICU stay (days) and time to extubation (hours). Secondary endpoint was mortality rate at the longest follow-up available.
Results
The 27 included manuscripts (28 trials) randomized 3,648 patients (1,870 to dexmedetomidine and 1,778 to control). Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction in length of ICU stay (weighted mean difference (WMD) = −0.79 [−1.17 to −0.40] days, p for effect <0.001) and of time to extubation (WMD = −2.74 [−3.80 to −1.65] hours, p for effect <0.001). Mortality was not different between dexmedetomidine and controls (risk ratio = 1.00 [0.84 to 1.21], p for effect = 0.9). High heterogeneity between included studies was found.
Conclusions
This meta-analysis of randomized controlled studies suggests that dexmedetomidine could help to reduce ICU stay and time to extubation, in critically ill patients even if high heterogeneity between studies might confound the interpretation of these results.
Introduction
Dexmedetomidine was approved by the Food and Drug Administration (FDA) at the end of 1999 as a short-term medication (<24 hours) for analgesia and sedation in mechanical ventilated intensive care unit (ICU) patients. In 2008, the FDA approved a new indication in non intubated patients requiring sedation before and/or during surgical and non-surgical procedures. Dexmedetomidine is a highly selective a2-adrenergic receptor agonist, which binds to transmembrane G protein-binding adrenoreceptors in the periphery (α2A), brain and spinal cord (α2B, α2C) tissues [1]. In contrast to other sedative agents, dexmedetomidine, by acting on a2 receptors in the locus caeruleus [2], has potential analgesic effects [3] without respiratory depression [4], [5]. Only one meta-analysis of randomized controlled trials (RCTs) [6] was published so far: Tan and Ho reported a reduction in length of ICU stay, but not in duration of time to extubation when dexmedetomidine was compared with alternative sedative agents.
Since several RCTs [7]–[14], including two large ones [8], were recently published, and one further RCT [15] was not included in the previous meta-analysis [6] we decided to perform an updated meta-analysis of all the RCTs ever performed on dexmedetomidine versus any comparator in the ICU setting to evaluate time to extubation, ICU stay and survival.
Materials and Methods
Search Strategy
Pertinent studies were independently searched in BioMedCentral, PubMed, Embase, and the Cochrane Central Register of clinical trials (updated February 1st 2013) by four trained investigators. The full PubMed search strategy aimed to include any RCTs ever performed in humans with dexmedetomidine in any clinical setting and is presented in the supplemental material (Text S1). In addition, we employed backward snowballing (i.e., scanning of references of retrieved articles and pertinent reviews) and contacted international experts for further studies with no language restriction.
Study Selection
References were first independently examined at a title/abstract level by four investigators, with divergences resolved by consensus, and then, if potentially pertinent, retrieved as complete articles. The following inclusion criteria were used for potentially relevant studies: random allocation to treatment (dexmedetomidine versus any comparator with no restrictions on dose or time of administration); studies involving patients who required mechanical ventilation in an ICU. The exclusion criteria were duplicate publications (in this case we referred to the first article published while retrieved data from the article with the longest follow-up available), non-adult patients and lack of data on all of the following: ICU stay, time to extubation and mortality. Two investigators independently assessed compliance to selection criteria and selected studies for the final analysis, with divergences resolved by consensus.
Data Abstraction and Study
Baseline, procedural, and outcome data were independently abstracted by four trained investigators (table 1 and table 2). If a trial reported multiple comparisons [25], [34], the comparators were aggregated as a single control group. At least two separate attempts at contacting original authors were made in cases of missing data. The co-primary endpoints of the present review were the length of ICU stay (days) and time to extubation (hours from randomization to extubation).
Table 1. Description of the 28 trials included in the meta-analysis.
| First author | Year | Setting | Dex patients | Control patients | Comparator | Comparator dose | Follow-up |
| Aziz AN [7] | 2011 | Cardiac surgery | 14 | 14 | Morphine | 4.6–46 µg/kg/h | 24 hours |
| Corbett SM [21] | 2005 | Cardiac surgery | 43 | 46 | Propofol | 0.2–0.7 µg/kg/h or 5–75 µg/kg/min | ICU stay |
| Elbaradie S [22] | 2004 | Major surgeries | 30 | 30 | Propofol | Bolus dose of 1 mg/kg followed by an infusion of 0.5–1 mg/kg/h | 24 hours after commencement of sedative infusions |
| Esmaoglu A [23] | 2009 | Post caesarean eclampsia | 20 | 20 | Midazolam | Loading dose of 0.05 mg/kg followed by an infusion of 0.1 mg/kg/h | ICU stay |
| Herr DL [24] | 2003 | Cardiac surgery | 148 | 147 | Propofol | NA | 24 hours after discharge from ICU |
| Jakob SM MIDEX [8] | 2012 | ICU | 249 | 251 | Midazolam | 0.03–0.2 mg/kg/h | 45 days |
| Jakob SM PRODEX [8] | 2012 | ICU | 251 | 247 | Propofol | 0.3–4.0 mg/kg/h | 45 days |
| Khalil MA [14] | 2012 | Cardiac surgery | 25 | 25 | Placebo | Loading dose 1 µg/kg over 10 minutes followed by a maintenance infusion of 0.5 µg/kg/h | Hospital stay |
| Leino K [9] | 2011 | Cardiac surgery | 44 | 43 | Placebo | 39 ml/h for 20 min, 24.5 ml/h for 40 minutes, 14 ml/h for 60 min, 10.5 ml/h for 120 min and then 7 ml/h | 48 hours after catheter insertion |
| Maldonado JR [25] | 2009 | Cardiac surgery | 4040 | 3840 | Propofol, midazolam | Propofol: 25–50 µg/kg/min; Midazolam: 0.5–2 mg/h | Hospital stay |
| Martin E [26] | 2003 | ICU | 203 | 198 | Placebo | 1 µg/kg for 10 min (loading dose) and then 0.4 µg/kg/h. The latter rate could be adjusted within the range of 0.2 to 0.7 µg/kg/h | 24 hours from infusion end |
| Memis D [27] | 2006 | ICU | 12 | 12 | Propofol | 2 mg/kg/h over 5-h infusion | ICU stay |
| Memis D [28] | 2007 | ICU | 20 | 20 | Midazolam | Loading dose of 0.2 mg/kg over 10 min followed by 0.1–0.5 mg/kg/h infusion | ICU stay |
| Memis D [29] | 2009 | ICU | 20 | 20 | Propofol | 1 mg/kg over 15 min followed by a maintenance dose of 1 to 3 mg/kg per hour | ICU stay |
| MendaF[10] | 2010 | Cardiac surgery | 15 | 15 | Placebo | 1 µg/kg in 15 min | ICU stay |
| Ozkan N [30] | 2007 | Cardiac surgery | 20 | 20 | Midazolam | 0.05–0.07 mg/kg/h | 24 hours post extubation |
| Pandharipande PP [31] | 2007 | ICU | 52 | 51 | Lorazepam | Maximum 10 mg/hr | 12 months |
| Reade MC [32] | 2009 | ICU | 10 | 10 | Haloperidol | 0.5–2 mg/hour preceded by a loading dose of 2.5 mg if desired | Hospital stay |
| Riker RR [33] | 2009 | ICU | 244 | 122 | Midazolam | Loading dose 0.05 mg/kg then infusion rate 0.02–0.1 mg/kg/h | 30 days |
| Ruokonen E [34] | 2009 | ICU | 41 | 44 | Propofol Midazolam | Propofol: 2.4 mg/kg/h for 1 h and then adjusted stepwise at 0.8, 1.6, 2.4, 3.2, and 4.0 mg/kg/h; Midazolam: boluses (1–2 mg), starting at 3 boluses per hour for 1 h, and thereafter 1–4 boluses per h, and if not sufficient as continuous infusion | 45 days |
| Sahin N [15] | 2005 | Cardiac surgery | 15 | 15 | Midazolam | 0.1 mg/kg/h intraoperative; 0.5–1 µg/kg/min ICU | 12 hours postoperatory |
| Shehabi Y [35] | 2009 | Cardiac surgery | 154 | 152 | Morphine | 10–70 µg/kg/ml | Hospital stay |
| Tasdogan M [36] | 2009 | Abdominal surgery | 20 | 20 | Propofol | 1 mg/kg over 15 minutes followed by a maintenance dose of 1–3 mg/kg/h | 25 days |
| Terao Y [11] | 2012 | Cervical spine surgery | 16 | 16 | Propofol | 0.1 mg/kg/min for 10 minutes as a loading dose, followed by a continuous infusion at 1 mg/kg/h | Hospital stay |
| Triltsch AE [37] | 2002 | ICU | 15 | 15 | Placebo | Loading dose of 6 µg/kg/h 1 for 10 min; maintenance infusion of 0.1–0.7 µg/kg/h | 24 hours after the end of study drug infusion |
| Venn RM [38] | 2001 | Major surgery | 10 | 10 | Propofol | 1–3 mg/kg/h after loading dose of up to 1 mg/kg over 10 min | 35 days |
| Wan LJ [12] | 2011 | ICU | 102 | 98 | Midazolam | NA | 24 hours |
| Yao L [13] | 2010 | ICU | 35 | 38 | Midazolam | Loading dose (0.06 mg/kg) and then maintained with 0.04–0.20 mg/kg/h | Time on mechanical ventilation |
Dex: dexmedetomidine; ICU: Intensive Care Unit; NA: not available; RASS: Richmond Agitation Sedation Scale; BIS: BispectralIndex ; MAAS: Motor Activity Assessment Scale.
Table 2. Doses, sedation scales and target sedation levels.
| First author | Study endpoint | Dexmedetomidine dose | Start study drug | Stop study drug |
| Aziz NA [7] | Sedation quality | 0.03–0.25 µg/kg/h | ICU arrival | After 24 hours |
| Corbett SM [17] | Sedation quality | Loading dose of 1 µg/kg in 15 min, followed by a 0.4/µg/kg/h infusion | During surgery, after CPB | Propofol was discontinued before extubation while dexmedetomidine was continued for up to 1 hour after extubation |
| Elbaradie S [22] | Sedation quality | Loading dose of 2.5 µg/kgin10 min followed by a 0.2–0.5 µg/kg/h infusion | ICU arrival | Before extubation |
| Esmaoglu A [23] | Sedation quality | Loading dose of 1 µg/kg in 20 min followed by a0.7 µg/kg/h infusion | ICU arrival | NA |
| Herr DL [24] | Sedation quality | Loading dose of 1 µg/kg in20 min followed by a0.4 µg/kg/h infusion. After transfer to the ICU, the infusion rate was titrated in the range of 0.2 to 0.7 µg/kg/h | Sternal closure | 6–24 hours after extubation |
| Jakob SM MIDEX [8] | Sedation quality | 0.2–1.4 µg/kg/h | Within 72 hours after ICU admission | Extubation, 14 days maximum |
| Jakob SM PRODEX [8] | Sedation quality | 0.2–1.4 µg/kg/h | Within 72 hours after ICU admission | Extubation, 14 days maximum |
| Khalil MA [14] | Sedation quality | Loading dose of 1 µg/kg in 10 minutes followed by a 0.5 µg/kg/h infusion | After induction of general anaesthesia | After stabilization of haemodynamics in the ICU |
| Leino K [9] | Renal effects | Five-step infusion of 4 µg/ml with the following decreasing infusion rate: 39 ml/h for 20 min, 24.5 ml/h for 40 min, 14 ml/h for 60 min, 10.5 ml/h for 120 min and then 7 ml/h (rates needed to achieve a pseudo steady-state plasma concentration of 0.60 µg/ml) | Immediately after anaesthesia induction | 4 h after ICU arrival |
| Maldonado JR [25] | Sedation quality | Loading dose of 0,4 µg/kg followed by 0.2–0.7 µg/kg/h | After CPB weaning | Maximum 24 h |
| Martin E [26] | Sedation quality | Loading dose of 1 µg/kg in 10 min followed by 0.4 µg/kg/h. The latter rate could be adjusted within the range of 0.2 to 0.7 µg/kg/h | Within 1 hour after ICU admission | For a minimum of 6 hours post extubation; total time was <24 hours |
| Memis D [27] | Gastric emptying | Loading dose of 2.5 µg/kg in 10 min followed by 0.2 µg kg/h over 5 h infusion | Within 4 hours after ICU admission | 5 hours |
| Memis D [28] | Inflammatory responses and gastric intramucosal pH | Loading dose of 1 µg/kg in 10 min followed by 0.2–2.5 µg/kg over 24 h infusion | ICU | NA |
| Memis D [29] | Indocyanine green elimination | Loading dose of 1 µg/kg in 10 min followed by a maintenance of 0.2–2.5 µg/kg/h | NA | 24 hours |
| Menda F [10] | Haemodynamic response to endotracheal intubation | 1 µg/kg in 15 min | Anaesthesia induction | NA |
| Ozkan N [30] | Haemodynamics and mixed venous oxygen saturation | Loading dose of 1 µg/kg followed by 0.2–0.4 µg/kg/h | Anaesthesia induction | NA |
| Pandharipande PP [31] | Sedation quality | Maximum 1.5 µg/kg/hr | ICU | Until extubation, for maximum 120 hours |
| Reade MC [32] | Sedation quality | Loading dose of 1.0 µg/kg in 20 min (if desired) followed by 0.2–0.7 µg/kg/hour | ICU | As long as clinically indicated, including following extubation if required |
| Riker RR [33] | Sedation quality | Loading dose of 1 µg/kg followed by 0.2–1.4 µg/kg/h | Within 96 hours after intubation | Extubation, 30 days maximum |
| Ruokonen E [34] | Sedation quality | 0.8 µg/kg/h for 1 h and then adjusted stepwise at 0.25, 0.5, 0.8, 1.1, and 1.4 µg/kg/h | Within 72 hours after ICU admission | Maximum 14 days |
| Sahin N [15] | Sedation quality and haemodynamics | 0.4 µg/kg/h intraoperative; 0.2–0.4 µg/kg/h in ICU | Anesthesia induction | 45 hours after extubation |
| Shehabi Y [35] | Sedation quality | 0.1–0.7 µg/kg/ml | Within 1 hour after ICU admission | Removal of chest drains, maximum 48 hours |
| Tasdogan M [36] | Inflammatory responses and intra abdominal pressure | Loading dose of 1 µg/kg in 10 min followed by 0.2–2.5 µg/kg/h | ICU arrival | 24 hours |
| Terao Y [11] | Sedation quality | Loading dose of 0.1 µg/kg/min in 10 minutes followed by 0.4 µg/kg/h | ICU arrival | First postoperative morning |
| Triltsch AE [37] | Sedation quality | Loading dose of 6 µg/kg/h in 10 min followed by 0.1–0.7 µg/kg/h | Within 1 hour after ICU admission | 6–7 hours after extubation, maximum overall 72 h |
| Venn RM [38] | Sedation quality | Loading dose of 2,5 µg/kg/h followed by 0,2–2,5 µg/kg/h | ICU arrival | Extubation |
| Wan LJ [12] | Sedation quality | NA | NA | NA |
| Yao L [13] | Sedation quality | Loading dose of 1 µg/kg in 10 min followed by 0.2–0.7 µg/kg/h | NA | NA |
ICU: Intensive Care Unit; CPB: cardiopulmonary bypass; NA: not available.
The secondary endpoint was mortality rate at the longest follow-up available. Adverse effects (hypotension and bradycardia as per author definition) were also analysed. Further endpoints included the number of patients requiring rescue doses of analgesic (opioids) or sedative (propofol, benzodiazepines, or any antipsychotics) drugs and the number of patients completely comfortable during ICU stay.
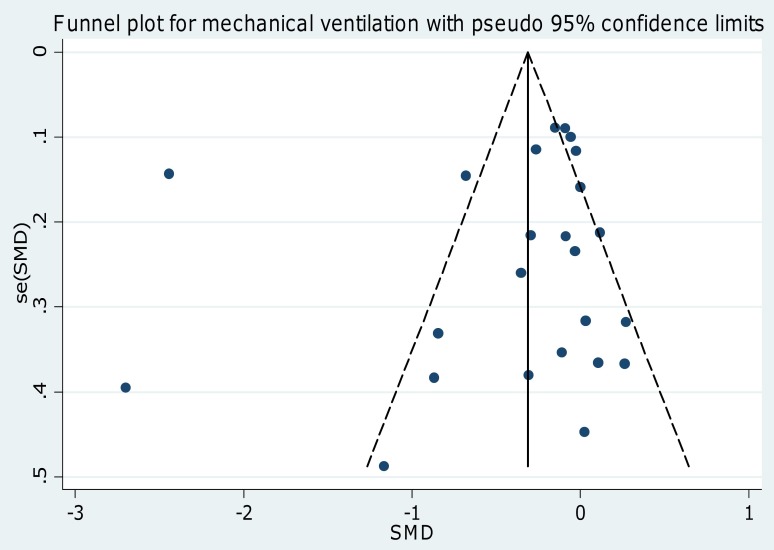
The internal validity and risk of bias of included trials was appraised by two independent reviewers according to the latest version of the “Risk of bias assessment tool” developed by The Cochrane collaboration [16], with divergences resolved by consensus. Publication bias was assessed by visually inspecting funnel plots and scatter plots and by analytical appraisal based on the Egger's linear regression test and on the Peters' test for asymmetry. According to the Egger [17] or Peters [18] methods for publication bias evaluation, a two-sided p value of 0.10 or less was regarded as significant.
Data Analysis and Synthesis
Computations were performed with Stata release 11, College Station, TX) and SAS 2002–08 program (release 9.2, SAS Institute, Inc, Cary, NC). Hypothesis of statistical heterogeneity was tested by means of Cochran Q test, with statistical significance set at the two-tailed 0.10 level, whereas extent of statistical consistency was measured with I2, defined as 100%×(Q-df)/Q, where Q is Cochran's heterogeneity statistic and df the degrees of freedom. Binary outcomes from individual studies were analysed to compute individual and pooled risk ratio (RR) with pertinent 95% confidence interval (CI), by means of inverse variance method and with a fixed-effect model in case of low statistical inconsistency (I2<25%) or with random-effect model (which better accommodates clinical and statistical variations) in case of moderate or high statistical inconsistency (I2>25%). Standardized mean differences (SMD), or weighted mean difference (WMD), and 95% confidence intervals were computed for continuous variables using the same models as just described. To evaluate if the small study effect had an influence on the treatment effect estimate, in case of evidence of between-study heterogeneity (I2>25), we compared the results of both fixed and random effect models. Sensitivity analyses were performed by sequentially removing each study and reanalysing the remaining dataset (producing a new analysis for each study removed) and by analysing only data from blinded studies and studies with low risk of bias.
Statistical significance was set at the two-tailed 0.05 level for hypothesis testing. Unadjusted p values are reported throughout. This study was performed in compliance with The Cochrane Collaboration and Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [16], [19], [20] (Checklist S1).
Results
Study Characteristics
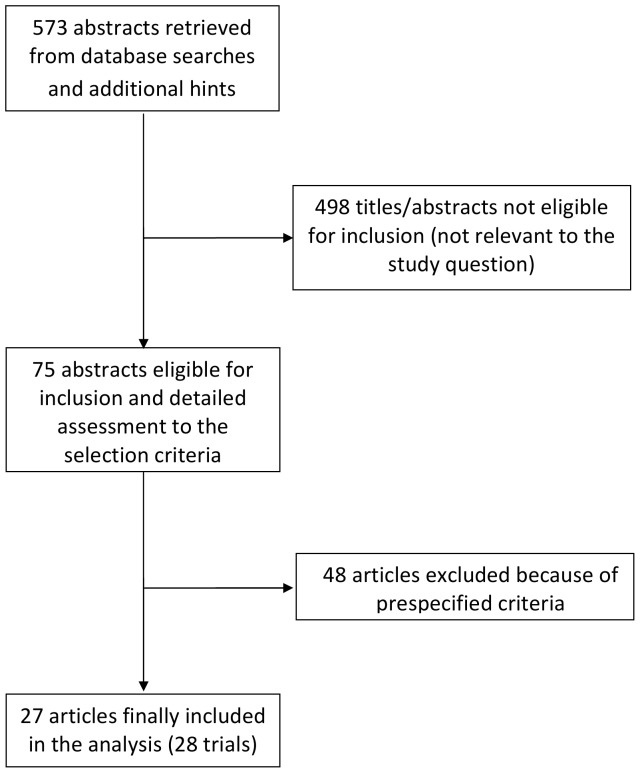
Database searches, snowballing, and contacts with experts yielded a total of 573 articles. The flow chart to select the final 27 manuscripts (28 trials) [7]–[15], [21]–[38] is detailed in figure 1, with major exclusions available in the supplemental material (Texts S2 and S3).
Figure 1. Flow diagram.
The flow chart to select the final 27 manuscripts (28 trials).
The 27 included manuscripts randomized 3,648 patients (1,870 to dexmedetomidine and 1,778 to control) (tables 1 and 2). Clinical heterogeneity was mostly due to setting, control treatment, and follow-up duration. Indeed, 13 trials used dexmedetomidine in a general ICU setting [8], [12], [13], [26]–[29], [31]–[34], [37], ten in cardiac surgery ICU patients [7], [9], [10], [14], [15], [21], [24], [25], [30], [35], four in major non-cardiac surgery ICU patients [11], [22], [36], [38] and one after caesarean section-eclampsia admitted to ICU [23]. Different techniques of dexmedetomidine administration were used: in 18 trials the continuous infusion was preceded by a loading dose that was often 1 mcg/kg [13], [14], [17], [23], [24], [26], [28]–[30], [32], [33], [36] but that varied between 0.1 to 6 mcg/kg in other trials [11], [22], [25], [27], [30], [34], [37], [38]. In other 6 trials only continuous infusion was used and ranged between 0.1 to 2.5 mcg/kg/h [7]–[9], [15], [31], [35] while in one trial only the loading dose was used [10] and one trial gave no details [12]. Study quality appraisal indicated that trials were of medium quality (Table S1); in particular 12of them had a low risk of bias.
Six different comparators were identified: propofol in 11 study arms [8], [11], [17], [22], [24], [25], [27], [29], [34], [36], [38], midazolam in 10 arms [8], [12], [13], [15], [23], [25], [28], [30], [33], [34], placebo in 5 arms [9], [10], [14], [26], [37], morphine in 2 arms [7], [35], haloperidol [32] and lorazepam [31] in one study.
Quantitative Data Synthesis
Effect of dexmedetomidine on ICU stay and time to extubation
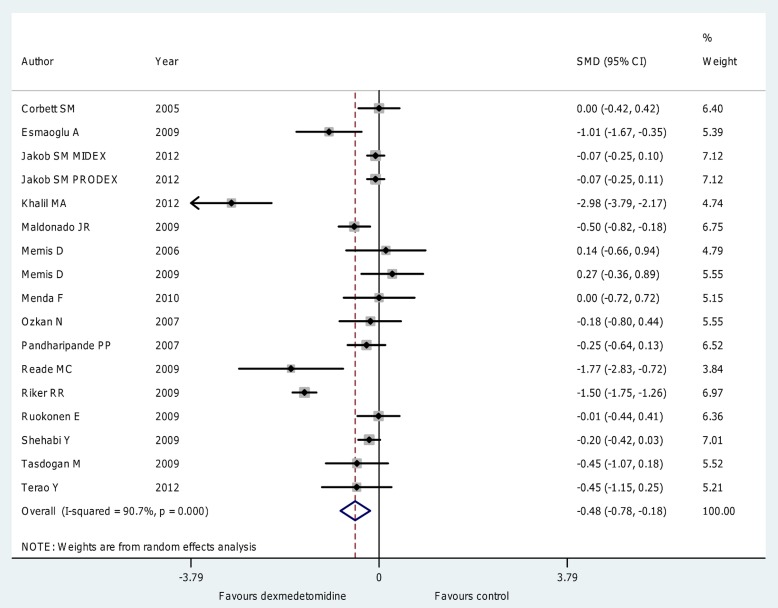
Overall analysis (figure 2; figure S1) showed that the use of dexmedetomidine was associated with a significant reduction in length of ICU stay (WMD = −0.79 [−1.17 to −0.40] days, p for effect <0.001, p for heterogeneity<0.001,I2 = 93%, SMD = −0.48 [−0.78 to −0.18], p for effect = 0.002, p for heterogeneity <0.001, I2 = 91%; with 17 studies and 2,424 patients included) with results confirmed when subanalyses were performed on studies including patients undergoing elective surgery (SMD = −0.60 [−1.05 to −0.15], p for effect = 0.008 with 8 studies included), in those including patients undergoing short term sedation (SMD = −0.45 [−0.81 to −0.09], p for effect = 0.02 with 11 studies included), in those including patients receiving a loading dose (SMD = −0.58 [−1.03 to −0.13], p for effect = 0.01 with 11 studies included) and in those receiving low (<0.7 µg kg−1 h−1) maintenance dose of dexmedetomidine (SMD = −0.62 [−1.04 to −0.20], p for effect = 0.004 with 10 studies included) as detailed in table 3.
Figure 2. Forest plot for the length of ICU stay.
Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction in length of ICU stay (SMD = −0.48 [−0.78 to −0.18] , p for effect = 0.002, p for heterogeneity <0.001, I2 = 91% with 17 studies and 2,424 patients included). ICU = intensive care unit; CI = confidence interval; SMD = standardized mean difference; N = number; SD = standard deviation; Dex = dexmedetomidine.
Table 3. Sensitivity analyses of intensive care unit stay and time to extubation.
| Outcome | Number of included trials | Dex patients | Controlpatients | SMD | 95% CI | P for effect | P for heterogeneity | I2 (%) |
| Overall trials | 28 trials (27 manuscripts) | 1,870 | 1,778 | |||||
| ICU stay | 17 | 1,274 | 1,150 | −0.48 | −0.78 to −0.18 | 0.002 | <0.001 | 91 |
| -Postoperative elective surgery patients | 8 | 373 | 372 | −0.60 | −1.05 to −0.15 | 0.008 | <0.001 | 86 |
| ---- Cardiac surgery | 6 | 337 | 336 | −0.57 | −1.11 to −0.03 | 0.04 | <0.001 | 89 |
| ---- CABG surgery | 4 | 103 | 106 | −0.76 | −1.94 to 0.42 | 0.2 | <0.001 | 93 |
| ---- Non Cardiac surgery | 2 | 36 | 36 | −0.75 | −1.23 to −0.27 | 0.002 | 0.3 | 23 |
| -ICU patients (non elective postoperative) | 9 | 901 | 778 | −0.38 | −0.82 to 0.06 | 0.09 | <0.001 | 93 |
| -excluding outlier studies [14], [32], [33] | 13 | 1438 | 1427 | −0.17 | −0.29 to −0.05 | 0.005 | 0.15 | 28 |
| - Long term sedation | 6 | 849 | 726 | −0.54 | −1.09 to 0.008 | 0.053 | <0.001 | 95 |
| - Short term sedation | 11 | 425 | 424 | −0.45 | −0.81 to −0.09 | 0.02 | <0.001 | 82 |
| - Daily interruption sedation | 5 | 839 | 716 | −0.38 | −0.96 to 0.18 | 0.18 | <0.001 | 96 |
| - High maintenance dose | 7 | 879 | 756 | −0.31 | −0.79 to 0.17 | 0.2 | <0.001 | 95 |
| - Low maintenance dose(<0.7 µg kg−1 h−1) | 10 | 395 | 394 | −0.62 | −1.04 to −0.20 | 0.004 | <0.001 | 85 |
| - Loading dose | 11 | 281 | 282 | −0.58 | −1.03 to −0.13 | 0.01 | <0.001 | 83 |
| - No loading dose | 6 | 993 | 868 | −0.36 | −0.81 to 0.10 | 0.13 | <0.001 | 96 |
| - Loading dose and high maintenance dose | 2 | 140 | 40 | −0.09 | −0.79 to 0.61 | 0.8 | 0.12 | 60 |
| - SENSITIVITY (including only blinded studies) | 8 | 891 | 768 | −0.56 | −1.09 to −0.04 | 0.04 | <0.001 | 95 |
| SENSITIVITY (including only low risk of bias studies) | 10 | 1065 | 940 | −0.44 | −0.86 to −0.02 | 0.04 | <0.001 | 94 |
| SENSITIVITY (removing 1 study at time) | All 95% CIs of SDM<0 and p<0.05 | |||||||
| SMALL STUDY EFFECT (fixed model) | −0.34 | −0.43 to −0.26 | <0.001 | |||||
| Time to extubation | 24 | 1,804 | 1,674 | −0.39 | −0.66 to −0.11 | 0.005 | <0.001 | 93 |
| -Postoperative elective surgery patients | 17 | 954 | 942 | −0.31 | −0.52 to −0.09 | 0.005 | <0.001 | 77 |
| ---- Cardiac surgery | 10 | 558 | 555 | −0.42 | −0.75 to −0.10 | 0.01 | <0.001 | 83 |
| ---- CABG surgery | 7 | 310 | 311 | −0.59 | −1.13 to −0.05 | 0.03 | <0.001 | 89 |
| ---- Non Cardiac surgery (3 studies did not specify the operative setting) | 4 | 76 | 76 | −0.15 | −0.47 to 0.17 | 0.4 | 0.8 | 0 |
| -ICU patients (non elective postoperative) | 7 | 850 | 732 | −0.52 | −1.25 to 0.21 | 0.16 | <0.001 | 97 |
| -excluding outlier studies [14], [32], [33] | 20 | 995 | 993 | −0.16 | −0.26 to −0.05 | 0.003 | 0.04 | 39 |
| - Long term sedation | 6 | 830 | 712 | −0.65 | −1.44 to 0.15 | 0.11 | <0.001 | 98 |
| - Short term sedation | 18 | 974 | 962 | −0.28 | −0.49 to −0.07 | 0.009 | <0.001 | 76 |
| - Daily interruption sedation | 4 | 785 | 664 | −0.69 | −1.70 to 0.32 | 0.18 | <0.001 | 99 |
| - High maintenance dose | 7 | 859 | 737 | −0.42 | −1.13 to 0.30 | 0.3 | <0.001 | 76 |
| - Low maintenance dose(<0.7 µg kg−1 h−1) | 16 | 843 | 839 | −0.30 | −0.53 to −0.07 | 0.009 | <0.001 | 76 |
| - Loading dose | 16 | 734 | 731 | −0.23 | −0.47 to 0.001 | 0.051 | <0.001 | 75 |
| - No loading dose | 7 | 968 | 845 | −0.60 | −1.25 to 0.05 | 0.07 | <0.001 | 97 |
| - Loading dose and high maintenance dose | 3 | 74 | 73 | −0.08 | −0.44 to 0.27 | 0.3 | 0.3 | 11 |
| SENSITIVITY (including only blinded studies) | 10 | 1241 | 1112 | −0.56 | −1.06 to −0.05 | 0.03 | <0.001 | 97 |
| SENSITIVITY (including only low risk of bias studies) | 8 | 1023 | 899 | −0.72 | −1.34 to −0.10 | 0.02 | <0.001 | 97 |
| SENSITIVITY (removing 1 study at time) | All 95% CIs of SDM<0 and p<0.05 | |||||||
| SENSITIVITY(Jakob study [8] included as time on mechanical ventilation) * | 24 | 1,804 | 1,674 | −0.38 | −0.66 to −0.10 | 0.007 | <0.001 | 93 |
| SMALL STUDY EFFECT (fixed model) | −0.31 | −0.38 to 0.24 | <0.001 | |||||
The overall analyses using weighted mean differences showed a reduction in intensive care unit stay of −0.79 [−1.17 to −0.40] days and a reduction in time to extubation of −2.74 [−3.80 to −1.65] hours in the dexmedetomidine group. It should be noted that the standard mean differences used in this table is not expressed in days or hours.
Dex: dexmedetomidine; SMD: standardized mean difference; CI: confidence interval; P: p-value; CABG: coronary artery bypass grafting; ICU: intensive care unit; NIV: non invasive ventilation.
duration of mechanical ventilation from randomization until patients were free of mechanical ventilation(including noninvasive).
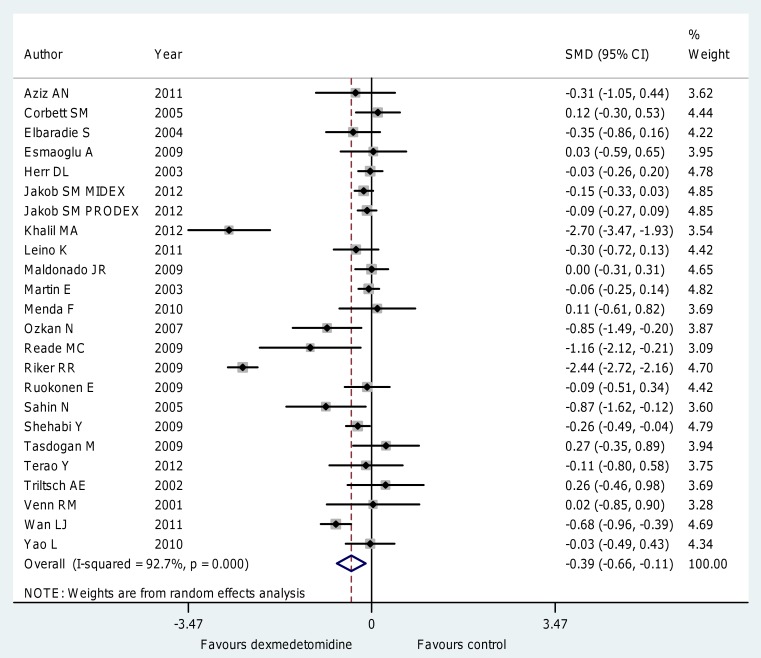
The use of dexmedetomidine was also associated (figure 3; figure S2) with a significant reduction of time to extubation (WMD = −2.74 [−3.80 to −1.65] hours, p for effect <0.001, p for heterogeneity<0.001,I2 = 96%, SMD = −0.39 [−0.66 to −0.11], p for effect = 0.005, p for heterogeneity <0.001, I2 = 93% with 24 studies and 3,478 patients included). Further subanalyses, detailed in table 3, confirmed these findings in patients receiving short term sedation (SMD = −0.28 [−0.49 to −0.07], p for effect = 0.009 with 18 studies included), in those receiving a low (<0.7 µg kg−1 h−1) maintenance dose (SMD = −0.30 [−0.53 to −0.07], p for effect = 0.009 with 16 studies included) and in those undergoing elective surgery (SMD = −0.31 [−0.52 to −0.09], p for effect = 0.005 with 17 studies included) with most of the positive finding coming from the cardiac surgery setting (SMD = −0.42 [−0.75 to −0.10], p for effect = 0.01 with 10 studies included). The largest study [8] included in this meta-analysis was also the only one to report both median and mean values for mechanical ventilation. Since these data were skewed, we repeated the analyses including median instead of mean values and didn't find differences in pooled estimate results (SMD = −0.39, 95% CI −0.66 to −0.12, I-square = 93%).
Figure 3. Forest plot for the time to extubation.
Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction of time to extubation (SMD = −0.39 [−0.66 to −0.11], p for effect = 0.005, p for heterogeneity <0.001, I2 = 93% with 24 studies and 3,478 patients included). CI = confidence interval; SMD = standardized mean difference; N = number; SD = standard deviation; Dex = dexmedetomidine.
Further subanalyses with the different comparators (propofol, midazolam, placebo and morphine) are detailed in supplemental material (TableS2 Table S3, Table S4 and Table S5) but were not informative with respect to ICU stay or time to extubation due to the paucity of trials included.
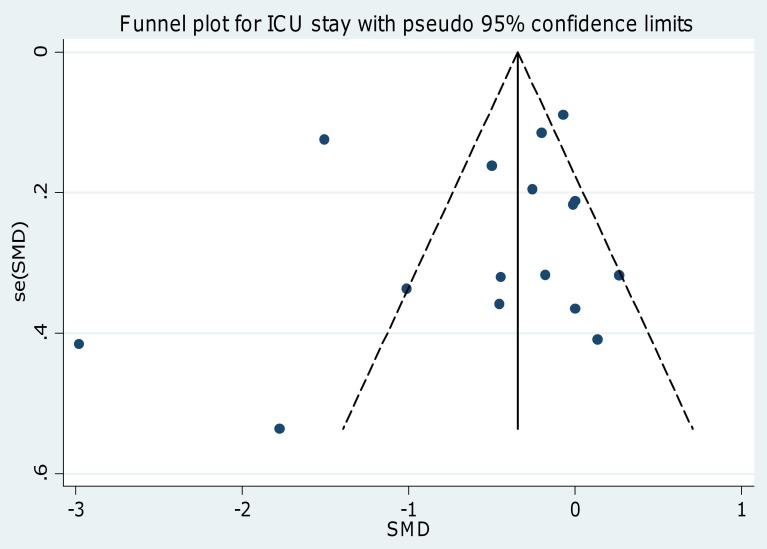
Visual inspection of funnel and scatter plots (figures 4 and 5; figures S3 and S4) did not identify a skewed or asymmetrical shape for the co-primary endpoints. Quantitative evaluation did not suggest a presence of publication bias, as measured by the Egger's test (p = 0.4 for the length of ICU stay and p = 0.5 for time to extubation) and Peters' test (p = 0.6 for the length of ICU stay and p = 0.9 for time to extubation). Since the funnel plots identified three outlier studies [14], [32], [33] we repeated the analyses removing them and found that the statistically significant difference in ICU stay and time to extubation was maintained (p = 0.005 and p = 0.003 respectively ) and the heterogeneity reduced (I2 = 28% and I2 = 39% respectively ) (table 3).
Figure 4. Funnel plot for the length of ICU stay.
Visual inspection of funnel plots did not identify a skewed or asymmetrical shape for the co-primary endpoints. Quantitative evaluation did not suggest a presence of publication bias, as measured by the Egger's test (p = 0.4) and Peters' test (p = 0.6). ICU = intensive care unit; SE = standard error; SMD = standardized mean difference.
Figure 5. Funnel plot for the time to extubation.
Visual inspection of funnel plots did not identify a skewed or asymmetrical shape for the co-primary endpoints. Quantitative evaluation did not suggest a presence of publication bias, as measured by the Egger's test (p = 0.5) and Peters' test (p = 0.9). SE = standard error; SMD = standardized mean difference.
Effect of dexmedetomidine on rescue doses of analgesic drugs, incidence of bradycardia, hypotension and mortality
Rescue doses of sedative or analgesic drugs were required less in the dexmedetomidine patients (892/1,459 [61%] in the dexmedetomidine group versus 977/1,366 [72%] in the control arm, p = 0.01 with 14 studies included). A subanalysis showed that dexmedetomidine was associated with a significant reduction in the number of patients requiring rescue doses of analgesic drugs (691/927 [67%] in the dexmedetomidine group versus 624/802 [78%] in the control arm, RR = 0.80 [0.66 to 0.98], p = 0.03) with no differences in the number of patients requiring rescue doses of sedative drugs (271/532 [51%] in the dexmedetomidine group versus 353/564 [63%] in the control arm, p = 0.3) (Table 4).
Table 4. Secondary Outcomes.
| Outcome | Number of included trials | Dex patients | Control patients | RR | 95% CI | P for effect | P for heterogeneity | I2 (%) |
| Overall trials | 28 trials (27 manuscripts) | 1,870 | 1,778 | |||||
| Mortality | 20 | 200/1,499 [13%] | 173/1,409 [12%] | 1.00 | 0.84 to 1.21 | 0.9 | 0.9 | 0 |
| Hypotension | 19 | 424/1,389 [31%] | 279/1,266 [22%] | 1.27 | 1.00 to 1.61 | 0.052 | <0.001 | 62 |
| Bradycardia | 17 | 220/1,374 [16%] | 64/1,246 [5%] | 2.43 | 1.88 to 3.14 | <0.001 | 0.9 | 0 |
| Patients requiring rescue doses of either sedatives or analgesics | 14 | 892/1,459 [61%] | 977/1,366 [72%] | 0.81 | 0.70 to 0.95 | 0.01 | <0.001 | 84 |
| ---requiring sedative drugs | 8 | 271/532 [51%] | 353/564 [63%] | 0.84 | 0.62 to 1.14 | 0.3 | <0.001 | 82 |
| ---requiring analgesic drugs | 6 | 621/927 [67%] | 624/802 [78%] | 0.80 | 0.66 to 0.98 | 0.03 | <0.001 | 88 |
| Number of patients completely comfortable | 3 | 112/253 [44%] | 103/254 [40.6%] | 1.07 | 0.49 to 2.49 | 0.9 | 0.003 | 82 |
Dex: dexmedetomidine; RR: relative risk; CI: confidence interval; P: p-value.
Dexmedetomidine was associated with an increased rate of bradycardia (220/1,374 [16%] in the dexmedetomidine group vs 64/1,246 [5%] in the control group, RR = 2.43[1.88 to 3.14], p for effect <0.001, p for heterogeneity = 0.9, I2 = 0% with 17 studies included) and with a trend towards an increased rate of hypotension (424/1,389 [31%] in the dexmedetomidine group vs 279/1,266 [22%] in the control group, RR = 1.27[1.00 to 1.61], p for effect 0.052, p for heterogeneity <0.001, I2 = 62% with 19 studies included) (Table 4).
No difference in mortality was recorded at the longest follow-up available (200/1,499 [13%] in the dexmedetomidine group vs 173/1,409 [12%] in the control group, RR = 1.00 [0.84 to 1.21], p for effect = 0.9 with 20 studies included). The univariate meta-regression of average follow-up against log-risk mortality showed no significant effects for time on mortality (n = 20, slope coefficient = −0.001 [−0.003 to 0.001], p = 0.31) (Table 4).
Sensitivity analyses
Estimate results from both random and fixed effect models were extremely similar (table 3); hence we excluded a considerable small study effect. Sensitivity analyses performed by sequentially removing each study and reanalysing the remaining dataset (producing a new analysis for each study removed), did not determine major changes in direction or magnitude of statistical findings, confirming the pooled effect of each co-primary endpoints (all SWD<1) and the statistical significance (all p of effect <0 .05). Sensitivity analyses carried out with studies with low risk of bias confirmed the overall results of our work showing a reduction in length of ICU stay in dexmedetomidine versus control group (SMD = −0.44 [−0.86 to −0.02] p for effect = 0.04, p for heterogeneity <0.001, I2 = 94% with 10 studies and 2,005 patients included) and in time to extubation (SMD = −0.72 [−1.34 to −0.10], p for effect = 0.02, p for heterogeneity <0.001, I2 = 97% with 8 studies and 1,922 patients included). Sensitivity analyses carried out with blinded studies confirmed the overall results of our work showing a reduction in length of ICU stay in dexmedetomidine versus control group (SMD = −0.56 [−1.09 to −0.04], p for effect = 0.04, p for heterogeneity <0.001, I2 = 95% with 8 studies and 1,659patients included) and a reduction in time to extubation (SMD = −0.56 [−1.06 to 0.05], p for effect = 0.03, p for heterogeneity <0.001, I2 = 97% with 10 studies and 2,353 patients included).
Discussion
Our meta-analysis confirmed that dexmedetomidine is associated with a reduction in ICU stay and suggested that it might reduce the time of extubation when compared to other sedative or hypnotic agent. Even if dexmedetomidine is associated with an increase in the risk of bradycardia and with a trend toward an increased risk of hypotension, no detrimental effects on mortality were detected.
The ideal sedative agent should provide anticipated, predictable effects, rapid onset, and quick recovery. It should be easy to administer with no adverse events, no interaction with other drugs, no accumulation of metabolites and no withdrawal effects at the end of infusion. Unluckily an ideal sedative agent that can suit the need of all patients does not yet exist.
Dexmedetomidine is one of the most recently released intravenous agents for sedation in the ICU, though the drug started to be investigated more than 20 years ago. It was introduced in clinical practice in the United States in 1999 while the European Medicine Agency authorised its use for all 27 European member states in September 2011. It is an alpha2-agonist and produces sedation acknowledged as “cooperative” or “arousable”, which is different from the sedation “clouding of consciousness” induced by drugs acting on GABA receptors, such as midazolam or propofol [39]. Tan and Ho, in a previous meta-analysis updated on December 2009 [6] reported that when dexmedetomidine was compared with alternative sedative agents it was associated with a statistically significant reduction in length of ICU stay, but not in duration of mechanical ventilation. We updated their findings on February 2013 identifying eight recently published manuscripts [7]–[14] and one trial that was not identified in their systematic search [15], thus increasing the number of patients by 50% (up to 3,648 overall randomized patients included in our meta-analysis) and providing more robust safety data. By adding more patients data we were able to show, for the first time in a meta-analysis, that dexmedetomidine increases the rate of bradycardia when all trials are pooled together and also shows a trend towards an increase rate of hypotension. However, these side effects were not associated with differences in mortality (200/1499 [13%] in the dexmedetomidine group vs 173/1409 [12%] in the control group, p = 0.9 with 20 studies included).
Dexmedetomidine decreases sympathetic nervous system activity and is therefore associated with an increase in cardiovascular adverse events. These effects may be most pronounced in patients with decreased autonomic nervous system response such as the elderly, diabetic patients, patients with chronic hypertension or severe cardiac disease such as valve stenosis or regurgitation, advanced heart block, severe coronary artery disease, or in patients who are already hypotensive and/or hypovolemic [40]. Therefore, in patients who depend on a high level of sympathetic tone or in patients with reduced myocardial function who cannot tolerate the decrease in sympathetic tone, loading doses of dexmedetomidine should be avoided. On the other side, the characteristics of dexmedetomidine to provide an ongoing sedation and sympathetic block could be beneficial in reducing early postoperative ischemic events in high-risk patients [41]–[42].
Intravenous administration of dexmedetomidine exhibits the following pharmacokinetic parameters: a rapid distribution phase with an half-life (t 1/2 α) of 6 min, a terminal elimination half-life (t 1/2 β) of 2 hours, and a steady-state volume of distribution (Vss) of 118 litres. It presents linear kinetics when infused in the range of 0.2–0.7 µg/kg/h for no more than 24 hours and undergoes almost complete biotransformation through direct glucuronidation and cytochrome P450 metabolism. Consequently it can accumulate in patients who are on P450 enzyme inhibitors, some of which are commonly used in ICU. Metabolites of biotransformation are excreted in the urine (95%) and faeces [43].
Limitations
We acknowledge that this study has several limitations. The quality of the included studies is not high since only 13 of them were blind. Moreover we noted high heterogeneity between the included studies. The heterogeneity remained when sensitivity analyses on studies with low risk of bias where performed. It was abolished only removing three outliers studies cited above. Nonetheless we excluded the possible influence of small-study effects on the results of our meta-analysis comparing the fixed- and random-effects estimates of the treatment effect (table 3). The overall reduction in ICU stay and time to extubation may appear clinically modest, but it should be acknowledged that the largest study [8] had very conservative imputation rules (to worst outcome) and this might have softened our results.
Conclusions
Dexmedetomidine for sedation in mechanically ventilated critically ill adult patients seems to help to reduce time to extubation and ICU stay. The known side effects (increased incidence of bradycardia and a trend toward an increased risk of hypotension) had no effect on the overall mortality in this meta-analysis of all the RCTs published so far.
Larger, multicentre, randomized clinical trials, especially in long term sedated patients requiring mechanical ventilation, would be welcome to confirm these findings.
Supporting Information
PRISMA checklist.
(DOC)
Forest plot for the length of ICU stay using standard mean difference (days) instead of weighted mean difference (absolute value with no units of measurement). Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction in length of ICU stay (SMD = −0.48 [−0.78 to −0.18], p for effect = 0.002, p for heterogeneity <0.001, I2 = 91% with 17 studies and 2,424 patients included). ICU = intensive care unit; CI = confidence interval; SMD = standardized mean difference; N = number; SD = standard deviation.
(TIF)
Forest plot for the time to extubation using standard mean difference (days) instead of weighted mean difference (absolute value with no units of measurement).. Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction of time to extubation (SMD = −0.39 [−0.66 to −0.11], p for effect = 0.005, p for heterogeneity <0.001, I2 = 93% with 24 studies and 3,478 patients included). CI = confidence interval; SMD = standardized mean difference; N = number; SD = standard deviation
(TIF)
Scatter plot for ICU stay
(TIF)
Scatter plot for time to extubation
(TIF)
Methodological quality summary: review authors' judgments about each methodological quality item for each included study.
(DOCX)
Subanalysis with propofol as comparator drug
(DOCX)
Subanalysis with midazolam as comparator drug
(DOCX)
Subanalysis with morphine as comparator drug
(DOCX)
Subanalysis with placebo as comparator drug
(DOCX)
Full PubMed search strategy
(DOCX)
Major exclusions
(DOCX)
References of the excluded studies
(DOCX)
Funding Statement
The study was conducted exclusively with departmental sources. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Paris A, Tonner PH (2005) Dexmedetomidine in anaesthesia. CurrOpinAnaesthesiol 18: 412–8. [DOI] [PubMed] [Google Scholar]
- 2. Huupponen E, Maksimow A, Lapinlampi P, Särkelä M, Saastamoinen A, et al. (2008) Electroencephalogram spindle activity during dexmedetomidine sedation and physiological sleep. Acta Anaesthesiol Scand 52: 289–94. [DOI] [PubMed] [Google Scholar]
- 3. Guo TZ, Jiang JY, Buttermann AE, Maze M (1996) Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology 84: 873–81. [DOI] [PubMed] [Google Scholar]
- 4. Iirola T, Aantaa R, Laitio R, Kentala E, Lahtinen M, et al. (2011) Pharmacokinetics of prolonged infusion of high-dose dexmedetomidine in critically ill patients. Crit Care 15: R257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morsch RD, Ferri MB, Vasconcelos CP, Capone Neto A, Akamine N, et al. (2005) Dexmedetomidine as a sedative agent for more than 24 hours in acutely ill patients. Critical Care 9: P111. [Google Scholar]
- 6. Tan JA, Ho KM (2010) Use of dexmedetomidine as a sedative and analgesic agent in critically ill adult patients: a meta-analysis. Intensive Care Med 36: 926–39. [DOI] [PubMed] [Google Scholar]
- 7. Abd Aziz N, Chue MC, Yong CY, Hassan Y, Awaisu A, et al. (2011) Efficacy and safety of dexmedetomidine versus morphine in post-operative cardiac surgery patients. Int J Clin Pharm 33: 150–4. [DOI] [PubMed] [Google Scholar]
- 8. Jakob SM, Ruokonen E, Grounds RM, Sarapohja T, Garratt C, et al. (2012) Dexmedetomidinevs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA 307: 1151–60. [DOI] [PubMed] [Google Scholar]
- 9. Leino K, Hynynen M, Jalonen J, Salmenperä M, Scheinin H, et al. (2011) Renal effects of dexmedetomidine during coronary artery bypass surgery: a randomized placebo-controlled study. BMC Anesthesiol 11: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Menda F, Köner O, Sayin M, Türe H, Imer P, et al. (2010) Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth 13: 16–21. [DOI] [PubMed] [Google Scholar]
- 11. Terao Y, Ichinomiya T, Higashijima U, Tanise T, Miura K, et al. (2012) Comparison between propofol and dexmedetomidine in postoperative sedation after extensive cervical spine surgery. J Anesth 26: 179–86. [DOI] [PubMed] [Google Scholar]
- 12. Wan LJ, Huang QQ, Yue JX, Lin L, Li SH (2011) Comparison of sedative effect of dexmedetomidine and midazolam for post-operative patients undergoing mechanical ventilation in surgical intensive care unit. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 23: 543–6. [PubMed] [Google Scholar]
- 13. Yao L, Zhou XM, Zhao JJ (2010) The role of dexmedetomidine in treatment of serious patients in intensive care unit. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 22: 632–4. [PubMed] [Google Scholar]
- 14. Khalil MA, Abdel Azeem MS (2013) The impact of dexmedetomidine infusion in sparing morphine consumption in off-pump coronary artery bypass grafting. Semin CardiothoracVasc Anesth 17: 66–71. [DOI] [PubMed] [Google Scholar]
- 15. Sahin N, Kabukcu H, Ozkan N, Titiz T (2005) The effects of postoperative dexmedetomidine and midazolam infusion on haemodynamics and sedation in patients after coronary artery bypass grafting. Eur J Anaesthesiol 22: 40.15816572 [Google Scholar]
- 16.Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Available: http://handbook.cochrane.org/ Accessed October 2013.
- 17. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–101. [PubMed] [Google Scholar]
- 18. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2006) Comparison of two methods to detect publication bias in meta-analysis. JAMA 295: 676–80. [DOI] [PubMed] [Google Scholar]
- 19. Biondi-Zoccai G, Lotrionte M, Landoni G, Modena MG (2011) The rough guide to systematic reviews and meta-analyses. HSR Proceedings in Intensive Care and Cardiovascular Anesthesia 3: 161–173. [PMC free article] [PubMed] [Google Scholar]
- 20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339: b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Corbett SM, Rebuck JA, Greene CM, Callas PW, Neale BW, et al. (2005) Dexmedetomidine does not improve patient satisfaction when compared with propofol during mechanical ventilation. Crit Care Med 33: 940–5. [DOI] [PubMed] [Google Scholar]
- 22. Elbaradie S, El Mahalawy FH, Solyman AH (2004) Dexmedetomidine vs. propofol for short-term sedation of postoperative mechanically ventilated patients. J Egypt Natl CancInst 16: 153–8. [PubMed] [Google Scholar]
- 23. Esmaoglu A, Ulgey A, Akin A, Boyaci A (2009) Comparison between dexmedetomidine and midazolam for sedation of eclampsia patients in the intensive care unit. J Crit Care 24: 551–5. [DOI] [PubMed] [Google Scholar]
- 24. Herr DL, Sum-Ping ST, England M (2003) ICU sedation after coronary artery bypass graft surgery: dexmedetomidine-based versus propofol-based sedation regimens. J Cardiothorac Vasc Anesth 17: 576–84. [DOI] [PubMed] [Google Scholar]
- 25. Maldonado JR, Wysong A, van der Starre PJ, Block T, Miller C, et al. (2009) Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics 50: 206–17. [DOI] [PubMed] [Google Scholar]
- 26. Martin E, Ramsay G, Mantz J, Sum-Ping ST (2003) The role of the alpha2-adrenoceptor agonist dexmedetomidine in postsurgical sedation in the intensive care unit. J Intensive Care Med 18: 29–41. [DOI] [PubMed] [Google Scholar]
- 27. Memis D, Dökmeci D, Karamanlioglu B, Turan A, Türe M (2006) A comparison of the effect on gastric emptying of propofol or dexmedetomidine in critically ill patients: preliminary study. Eur J Anaesthesiol 23: 700–04. [DOI] [PubMed] [Google Scholar]
- 28. Memiş D, Hekimoğlu S, Vatan I, Yandim T, Yüksel M, et al. (2007) Effects of midazolam and dexmedetomidine on inflammatory responses and gastric intramucosal pH to sepsis, in critically ill patients. Br J Anaesth 98: 550–2. [DOI] [PubMed] [Google Scholar]
- 29. Memiş D, Kargi M, Sut N (2009) Effects of propofol and dexmedetomidine on indocyanine green elimination assessed with LIMON to patients with early septic shock: a pilot study. J Crit Care 24: 603–8. [DOI] [PubMed] [Google Scholar]
- 30. Ozkan N, Sahin N, Karakaya Kabukcu H, Celikbilek G, Aydogdu Titiz T (2007) Comparison of the effects of dexmedetomidine with midasolam on haemodynamics and oxygen profile in patients undergoing coronary artery bypass grafting. Gogus-Kalp-Damar Anestezive Yogun Bakim Dernegi Dergisi 13: 161–168. [Google Scholar]
- 31. Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, et al. (2007) Effect of sedation with dexmedetomidinevslorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 298: 2644–2653. [DOI] [PubMed] [Google Scholar]
- 32. Reade MC, O'Sullivan K, Bates S, Goldsmith D, Ainslie WR, et al. (2009) Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial. Crit Care 13: R75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, et al. (2009) Dexmedetomidinevs midazolam for sedation of critically ill patients: a randomized trial. JAMA 301: 489–99. [DOI] [PubMed] [Google Scholar]
- 34. Ruokonen E, Parviainen I, Jakob SM, Nunes S, Kaukonen M, et al. (2009) Dexmedetomidine versus propofol/midazolam for long-term sedation during mechanical ventilation. J Intensive Care Med 35: 282–90. [DOI] [PubMed] [Google Scholar]
- 35. Shehabi Y, Grant P, Wolfenden H, Hammond N, Bass F, et al. (2009) Prevalence of delirium with dexmedetomidine compared with morphine based therapy after cardiac surgery: a randomized controlled trial (DEXmedetomidineCOmpared to Morphine-DEXCOM Study). Anesthesiology 111: 1075–84. [DOI] [PubMed] [Google Scholar]
- 36. Tasdogan M, Memis D, Sut N, Yuksel M (2009) Results of a pilot study on the effects of propofol and dexmedetomidine on inflammatory responses and intraabdominal pressure in severe sepsis. J Clin Anesth 21: 394–400. [DOI] [PubMed] [Google Scholar]
- 37. Triltsch AE, Welte M, von Homeyer P, Grosse J, Genähr A, et al. (2002) Bispectral index-guided sedation with dexmedetomidine in intensive care: a prospective, randomized, double blind, placebo-controlled phase II study. Crit Care Med 30: 1007–14. [DOI] [PubMed] [Google Scholar]
- 38. Venn RM, Grounds RM (2001) Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth 87: 684–90. [DOI] [PubMed] [Google Scholar]
- 39. Aho M, Erkola O, Kallio A, Scheinin H, Korttila K (1993) Comparison of dexmedetomidine and midazolam sedation and antagonism of dexmedetomidine with atipamezole. J Clin Anesth 5: 194–203. [DOI] [PubMed] [Google Scholar]
- 40. Gertler R, Brown HC, Mitchell DH, Silvius EN, Mitchell DH (2001) Dexmedetomidine: a novel secative-analgesic agent. Proc (Bayl Univ Med Cent) 14: 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Talke P, Li J, Jain U, Leung J, Drasner K, et al. (1995) Effects of perioperative dexmedetomidine infusion in patients undergoing vascular surgery. The Study of Perioperative Ischemia Research Group. Anesthesiology 82: 620–633. [DOI] [PubMed] [Google Scholar]
- 42. Chorney SR, Gooch ME, Oberdier MT, Keating D, Stahl RF (2013) The safety and efficacy of dexmedetomidinefor postoperative sedation in the cardiac surgery intensive care unit. HSR Proc Intensive Care Cardiovasc Anesth 5 (1) 17–24. [PMC free article] [PubMed] [Google Scholar]
- 43. Yazbek-Karam VG, Aouad MM (2006) Perioperative uses of dexmedetomidine. Middle East J Anesthesiol 18: 1043–58. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)
Forest plot for the length of ICU stay using standard mean difference (days) instead of weighted mean difference (absolute value with no units of measurement). Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction in length of ICU stay (SMD = −0.48 [−0.78 to −0.18], p for effect = 0.002, p for heterogeneity <0.001, I2 = 91% with 17 studies and 2,424 patients included). ICU = intensive care unit; CI = confidence interval; SMD = standardized mean difference; N = number; SD = standard deviation.
(TIF)
Forest plot for the time to extubation using standard mean difference (days) instead of weighted mean difference (absolute value with no units of measurement).. Overall analysis showed that the use of dexmedetomidine was associated with a significant reduction of time to extubation (SMD = −0.39 [−0.66 to −0.11], p for effect = 0.005, p for heterogeneity <0.001, I2 = 93% with 24 studies and 3,478 patients included). CI = confidence interval; SMD = standardized mean difference; N = number; SD = standard deviation
(TIF)
Scatter plot for ICU stay
(TIF)
Scatter plot for time to extubation
(TIF)
Methodological quality summary: review authors' judgments about each methodological quality item for each included study.
(DOCX)
Subanalysis with propofol as comparator drug
(DOCX)
Subanalysis with midazolam as comparator drug
(DOCX)
Subanalysis with morphine as comparator drug
(DOCX)
Subanalysis with placebo as comparator drug
(DOCX)
Full PubMed search strategy
(DOCX)
Major exclusions
(DOCX)
References of the excluded studies
(DOCX)