Abstract
Comprehensive interventions that address both individual and structural determinants associated with HIV/STI risk are gaining increasing attention over the past decade. Microenterprise development offers an appealing model for HIV prevention by addressing poverty and gender equality. This study systematically reviewed the effects of microenterprise development interventions on HIV/STI incidence and sexual risk behaviors. Microenterprise development was defined as developing small business capacity among individuals to alleviate poverty. Seven eligible research studies representing five interventions were identified and included in this review. All of the studies targeted women, and three focused on sex workers. None measured biomarker outcomes. All three sex worker studies showed significant reduction in sexual risk behaviors when compared to the control group. Non-sex worker studies showed limited changes in sexual risk behavior. This review indicates the potential utility of microenterprise development in HIV risk reduction programs. More research is needed to determine how microenterprise development can be effectively incorporated in comprehensive HIV control strategies.
Keywords: HIV/AIDS, Sexually transmitted diseases, Prevention and control, Entrepreneurship, Small business
Introduction
Poverty and gender inequality are two of the most commonly recognized social determinants driving HIV/STI disease risk among most-at-risk populations [1–4]. However, the majority of HIV prevention efforts to date have focused on decreasing individual-level risk [5, 6] without adequate treatment of the broader economic and social drivers of HIV risk and vulnerability [5, 7]. Advances in multidisciplinary HIV research over the past decade have facilitated a shift toward testing more comprehensive HIV prevention programs that address both individual and structural factors facilitating HIV transmission [5–8].
In recent years, microenterprise development is increasingly included in comprehensive HIV/STI interventions, however the number has remained small [9, 10]. The microenterprise development process often includes development of viable products and/or services, access to markets, financial skills training, and financial support or microfinance [4, 9]. For the purposes of this review, we define microenterprise development as expanding small business capacity among individuals in order to alleviate poverty [11], including microcredit, defined as the provision of small loans to low-income entrepreneurs; microfinance, defined as banking or financial services such as savings and insurance targeted to low- and moderate-income businesses/households; income-generating activities; or a combination of the above [12]. Although the links are complex and multi-dimensional, HIV/STI risk can be strongly influenced by poverty and gender inequality. The improvement in these two socio-economic factors might serve as underlying mechanisms by which microenterprise development can contribute to reducing HIV/STI vulnerability [4, 10]. However, the evidence supporting microenterprise development as an effective poverty reduction strategy among poor women has so far been mixed [11, 13, 14]. Although the promise of microfinance suggests that it can enable households to invest in productive assets, start new businesses, and generate increases in income and consumption, evidence of economic improvements as indicated by savings, asset holdings, and yearly returns are modest at best, particularly for the extreme poor [13–16]. From a gender perspective, microenterprise development interventions often seek to overcome structural obstacles faced by women, such as the perception or reality of men as the primary controllers of financial resources, unequal pay for women, social norms that limit women’s mobility, and unequal legal rights focused on household assets [17]. The evidence to date on whether such transformations happen as a result of microenterprise development interventions is also mixed [15].
More HIV/STI control strategies are using a comprehensive approach that integrates behavioral interventions, community involvement, and microenterprise development to create sustainable change [5, 6, 18–20]. The goal of this literature review is to examine the effect of microenterprise development interventions on sexual risk behavior and HIV/STI infection. The findings may guide the process of designing and planning of programs to reduce HIV/STI risk and transmission.
Methods
Search Strategy
We searched PubMed, SSRN, Cochrane, JSTOR, the International AIDS Society abstract database, Social Edge, Duke Center for the Advancement of Social Entrepreneurship, Ashoka Fellows database, and Proquest Entrepreneurship database for articles indexed on or before April 2, 2013. The search terms included medical subject headings (MeSH) and keywords for HIV or sexually transmitted infections and keywords relating to microenterprise development (“microenterprise” or “microfinance” or “microcredit” or “income generation”). We included both micro-lending interventions as well as small business development.
Criteria for Selecting Studies for This Review
Articles were included in the review if the interventions included a microenterprise development component and measured either: (1) the prevalence or incidence of HIV and/or other STIs; or (2) sexual risk behaviors (i.e. condom use, number of sex partners, etc.). All included manuscript citations were compiled into a single library using citation manager software (EndNote X5, 2012). Duplicate citations were removed. Remaining unique citations were screened by two independent reviewers (RC and RL) based on article title. If the title was unclear, then the reviewers examined the abstract. Disagreements were resolved by a third reviewer (JT) through abstract review. The following exclusion criteria were applied: (1) review papers, (2) non peer-reviewed local/government reports, (3) editorials, (4) dissertations, and (5) descriptive studies. No publications were excluded on the basis of study design. There were no language restrictions to the search. Comprehensive interventions in which microenterprise development was included with sexual risk behavioral interventions were included. The reference lists of recent reviews on microenterprise development and sexual health were hand-searched to identify other possible articles.
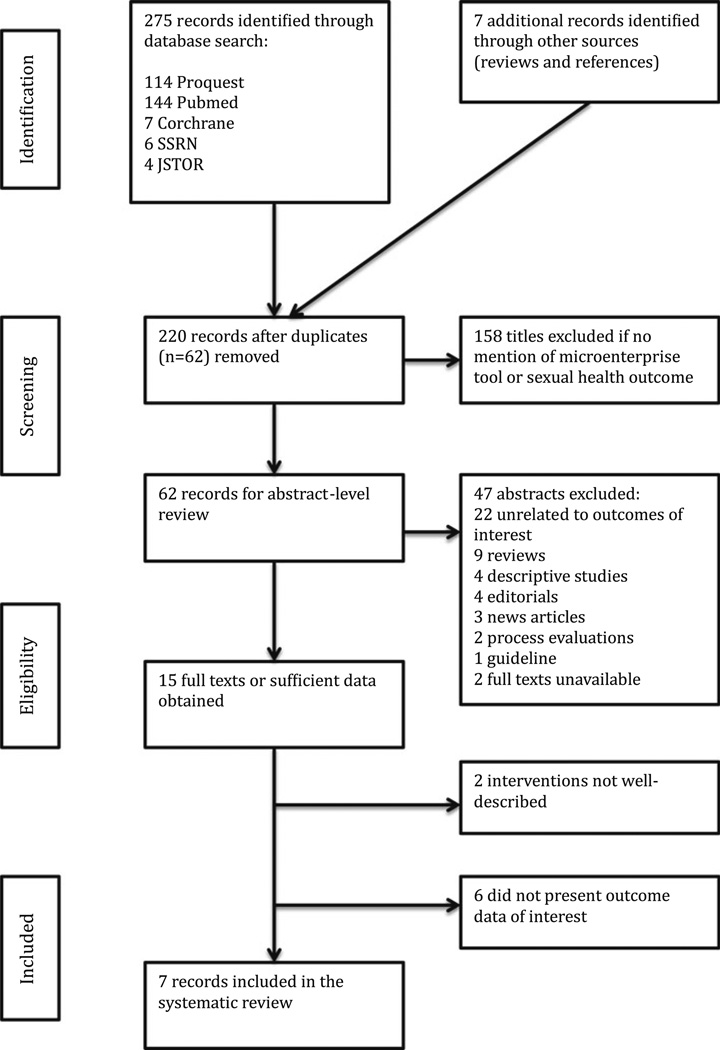
The literature search of articles identified 282 citations for microenterprise development interventions and HIV and/or sexual health. After removing duplicates, 220 unique citations remained, of which 158 were excluded based on title (Fig. 1). Our search and screening algorithm produced 62 citations for abstract-level review. Reasons for abstract exclusion are detailed in Fig. 1. The excluded non-peer reviewed studies were not directly relevant to microenterprise development and/or HIV/STI risk reduction. The methods sections of the remaining 15 articles were examined and studies in which the outcomes did not include HIV/STI incidence or behavioral markers of interest were excluded. Articles in which the intervention was not explicitly described were also excluded. Seven studies describing five interventions met inclusion criteria for this review.
Fig. 1.
Flow chart of research study selection (original search completed April 2, 2013)
Data Extraction
The following study details were extracted by a single investigator (RC) into an Excel database: type of microenterprise development, study location, sampling period, study design, study population, sample size, median length of follow up, and community based organization involvement. Of the seven studies, one was a randomized control trial [21] and two were secondary analyses based off the same study [22, 23]. Community-based organization involvement was defined as the inclusion of a public or private non-profit that is representative of the community and is engaged in meeting the needs of the community. Extracted study data included the intervention condition, comparison condition, sexual health outcomes, non-sexual health outcomes, and multi-sectoral involvement, which is defined by collaborative efforts between different sectors (e.g. partnerships between microfinance institutions and academic research institutions). The primary outcome variable was HIV/STI prevalence or incidence and sexual risk behaviors.
Study Quality Assessment
The quality of the studies was assessed using a validated quality assessment tool adapted from the AHRQ [24]. The following eight items were assessed to calculate a total quality score: (1) clear definition of target population, (2) representative ness of probability sampling, (3) sample characteristics matching the overall population, (4) adequate response rate, (5) standardized data collection methods, (6) reliability of survey measures/instruments, (7) validity of survey measures/instruments, (8) appropriate statistical methods. Answers were scored 0 and 1 for ‘no’ and ‘yes’, respectively. The total quality score varied between 0 and 8 for each study, with a higher number corresponding to higher quality.
Analysis
Due to the small number of interventions identified and the diversity of the study populations and microenterprise development interventions, a meta-analysis was not performed. This review presents descriptive information about each individual study.
Results
Study Selection
As seen in Fig. 1, 62 abstracts were examined and 15 research studies met inclusion criteria of having a microenterprise development intervention and HIV/STI measures. A total of seven studies describing five unique interventions were identified for review. One of the microenterprise development interventions was analyzed in two separate articles, both of which were secondary analyses of the index participants [22, 23]. One study was an observational study that examined the association between the length of exposure to a microfinance intervention and the participants’ sexual health behaviors [25]. Study descriptions and designs are outlined in Table 1. Intervention conditions, outcome measures, and quality assessments are described in Table 2.
Table 1.
Study characteristics
| First author (year) |
Type of microenterprise development |
Study location |
Sampling period |
Study design | Study population | Sample size |
Median length of follow up (months) |
CBO involvement |
|---|---|---|---|---|---|---|---|---|
| [26] | Microfinance | Kibera slums in Nairobi, Kenya |
1/2002–8/ 2005 |
Non-experimental study with pre- and post-test measures without controls |
Female sex workers who have participated in STI/HIV peer education program for at least 6 months |
227 | 20 | Yes |
| [27] | Small business/ skills training |
Baltimore, MD USA |
1/2002–6/ 2003 |
Non-experimental study with pre- and post-test measures without controls |
Female sex workers ages 18–45 who have used heroin and/or cocaine at least weekly in past month |
50 | 3 | Yes |
| [21] | Small business/ skills training |
Chennai, India |
8/ 2008–2009 |
Randomized control trial |
Female sex workers | 100 | 3 | Yes |
| [22] | Microfinance | Limpopo Province, South Africa |
6/2001–2/ 2006 |
Cluster randomized trial |
Women enrolled in combined microfinance and HIV education program |
1409 | 24 | Yes |
| [23] | Microfinance | Limpopo Province, South Africa |
6/2001–3/ 2005 |
Cluster randomized trial |
Young women ages 14–35 enrolled in combined microfinance and HIV education program |
262 | 24 | Yes |
| [25] | Microfinance | Limbe, Haiti | 6/2009–8/ 2009 |
Cross-sectional survey |
Women ages 18–49 enrolled in the Fonkoze micro-lending program |
192 | N/A | Yes |
| [28] | Microfinance and small business/skills training |
Chitungwiza and Epworth, Zimbabwe |
2004 | Non-experimental study with pre- and post-test measures without controls |
Adolescent female orphans |
50 | 6 | Yes |
CBO community based organization
Table 2.
Study outcomes
| First author (year) |
Intervention condition | Comparison condition |
Sexual health outcomes |
Major findings | Major limitations | Total QA scorea |
|---|---|---|---|---|---|---|
| [26] | Mixed intervention consisting of a STI/HIV education program and a group micro- lending model that also includes business skills training and promotion of a savings culture |
Baseline (peer- mediated STI/HIV education only) |
O.1) Number of sexual partners (total, casual, regular) O.2) Condom use with all, casual, and regular sexual partners O.3) Exit from sex work |
O.1) Decreased number of total partners and regular sex partners (P< 0.001 for both). No difference in the mean number of casual partners O.2) Increased condom use with regular partners (P = 0.031) O.3) 45.4 % reported exit from sex work |
L.1) Non-experimental study with no control group L.2) Self-selection bias into MF initiative L.3) Mean age of women was 41 years, older than peak age of initial HIV infection in Kenya, which may affect motivation to exit sex work. Limited external validity |
5 |
| [27] | Mixed intervention consisting of 6 training sessions that covered HIV prevention and jewelry making and marketing skills. 50 % of final proceeds from sales given to jeweler |
Baseline data | O.1) Median number of sexual partners (total, regular, and casual) per month O.2) Condom use with regular partners, casual partners, and clients O.3) Median number of clients per month |
O.1) Decreased total number of sexual contacts per month in IG (10.0 vs. 3.0, p = 0.01) O.2) Increased condom use with clients in IG (53.0 % vs. 75.0 %, p = 0.03) O.3) Decreased median number of monthly clients in IG (9.0 vs. 3.0, p = 0.025) |
L.1) Non-experimental study with no control group L.2) Small sample size of pilot study was used to assess the feasibility L.3) Short-term follow up (3 months) limits external validity |
5 |
| [21] | Mixed intervention consisting of 100 h of bag tailoring trainings plus 8 h of HIV prevention trainings. Participants were also paid 100 Rs for each bag sold. |
8 h of HIV prevention trainings only |
O.1) Mean number of sex partners (total and clients) O.2) Condom use at last sex exchange O.3) Regular use of condoms with clients |
O.1) Decreased number of sex partners at 6 months follow- up (total and clients) O.2) No difference in condom use at last exchange O.3) No difference in regular condom use with clients |
L.1) Short-term follow up (3 months) limits external validity |
7 |
| [22] | Intervention 1: combined MF program and 10 training sessions involving HIV education, gender roles, and community mobilization Intervention 2: MF program only |
Matched villages with no intervention |
O.1) Condom use at last sex with all non-spousal partners O.2) Combined MF vs. control: economic well- being, empowerment, HIV-related risk behavior O.3) MF only vs. control: economic well being, empowerment, HIV-related risk behavior O.4) Combined MF vs. MF only: economic well being, empowerment, HIV-related risk behavior |
O.1) No differences condom use between groups O.2) Pattern of improved economic well-being, empowerment, and HIV- related risk behavior (excluding condom use) O.3) Pattern of improved economic well-being (aRRs 1.22–3.38, CI excluding 1 for most indicators). Inconsistent findings for empowerment and HIV-related variables O.4) Similar improvements in economic well-being. Combined MF group showed greater effects on empowerment and HIV- related variables |
L.1) Self-selection bias into intervention groups |
7 |
| [23] | Mixed intervention consisting of a group-based MF program and training sessions focused on HIV education, gender roles, and community mobilization |
Women ages 14–35 from pair matched villages with no intervention |
O.1) More than one sexual partner in past 12 months O.2) Unprotected sex during last intercourse with non-spousal partner in past 12 months O.3) Communication with household members about sex matters in past 12 months |
O.1) No differences in having more than one sexual partner in past 12 months between IG and CG O.2) IG less likely to have unprotected sex with non- spousal partner (aRR = 0.76, 95 % CI 0.60–0.96) O.3) IG had higher levels of household HIV-related communication (aRR = 1.46, 96 % CI 1.01–2.12) |
L.1) Self-selection bias into intervention group L.2) Higher level of non- response from comparison group at follow-up L.3) Low numbers of new HIV infections during intervention period prevented examination of differences in HIV incidence |
7 |
| [25] | Mixed intervention consisting of group-based MF programs and 1 year educational trainings on basic literacy, business skills, and health education; IG defined as participation in program for more than 12 months |
Women enrolled in the MF program for less than 12 months |
O.1) More than one sexual partners in previous 12 months O.2) Ever used a condom in previous 12 months O.3) Condom use with unfaithful partner |
O.1) Numbers too small to calculate statistics, O.2) No differences found in condom use in previous 12 months between IG and CG, O.3) Trend towards increased condom use with unfaithful partner (OR = 3.95, 95 % CI 0.93–16.85) |
L.1) Observational study with no experimental group, limited assessment of directionality of association L.2) Self-selection bias, as study population only included women who were current MF clients and thus more inclined to participate in MF activities |
5 |
| [28] | Mixed intervention consisting of HIV and gender education, business training and mentorship (including workshops on soap making, tie-dye, and candle making), microcredit loans |
Baseline data | Condom use with primary partner |
No differences in condom use with primary partner between intervention and baseline data |
L.1) Small sample size of pilot study was used to inform research design and study interventions with no intention to assess quantitative outcomes for evaluation L.2) Non-experimental study with no control group L.3) Use of modified group- lending model that paid loans in lump sum rather than installments after repayment L.4) Threats to personal safety and security of goods may have influenced business management and perceived benefits of MF |
4 |
MF microfinance, QA quality assessment, IG intervention group, CG comparison group, aRR adjusted risk ratio
QA score out of 8: (1) clear definition of target population, (2) representativeness of probability sampling, (3) sample characteristics matching the overall population, (4) adequate response rate, (5) standardized data collection methods, (6) reliability of survey measures/instruments, (7) validity of survey measures/instruments, (8) appropriate statistical methods (adapted from AHRQ [13])
Study Characteristics and Quality Assessment
The seven studies included a total of 2,290 participants from six countries (Haiti, India, Kenya, South Africa, United States, Zimbabwe). With the exception of one study [22], all interventions were small studies with less than three hundred participants. All of the studies targeted women; three specifically evaluated the effect of microenterprise development interventions on female sex workers [21, 26, 27] and two targeted adolescent women [23, 28], of which one was a secondary analysis of a sub-population of the index women [23].
Study designs included three non-experimental studies with pre- and post-test measures without controls [26–28], one cluster randomized trial described in two secondary analyses [22, 23], one randomized control trial [21], and one cross-sectional survey [25]. The length of post-intervention follow-up ranged from 3 to 24 months, with a median of 13 months. All studies cooperated with a community-based organization to deliver the microenterprise development interventions. The randomized controlled trial and the two analyses of the cluster randomized trial received a quality assessment (QA) score of 7. Two of the non-experimental pre-post studies and the cross-sectional survey received a QA score of 5 [25–27], and one non-experimental pre-post study received a QA score of 4 [28]. All had threats to external validity: many due to self-selection biases that may mask any unmeasured differences between comparison groups, one due to short length of follow up [21, 27], and one from use of a modified group-lending system [28]. Non-randomization in four studies limited the assessment of directionality of the associations [25–28], and one study had low response rates [28].
Types of Interventions
The identified microenterprise development interventions included four micro-lending programs [22, 23, 25, 26], two business skills training programs [21, 27], and one intervention that provided both [28]. The primary intervention with two secondary analyses contained two intervention arms, of which one was a mixed microenterprise development and education model, and the other was a microenterprise development only model [22, 23]. All lending programs except one used a group financing model with joint liability, where loans were received and repaid in groups to build community and guarantee repayment. Dunbar et al. [28] tailored the microfinance component to adolescent girls by following a modified group-lending model that paid loans in a lump sum rather than interval installments. Given that the loans were small and most participants required the entire amount to start their microenterprises, this model did not follow the solidarity group repayment system. Two interventions provided skills training sessions, one focused on developing jewelry business skills [27], and another focused on developing bag tailoring skills [21]. One study provided both skills training, including soap making, tie-dye of materials, or candle making, in addition to micro-loans that were also received through a group-based model [28]. All studies were mixed interventions comprised of a microenterprise development component and an educational component. The educational component in the intervention by Odek et al. [26] focused on business training skills, and all others focused on HIV prevention and safe sex practices. Most studies also addressed communication skills and violence against women in the interventions [8, 21, 22, 27, 28].
Outcome Measures
All primary sexual health outcomes were based on self-reported HIV-related risk behaviors. One article reported HIV prevalence at baseline without post-intervention bio-marker data [23]. As described in Table 2, outcomes included condom use measures, which ranged from last sex with “all partners”, “non-spousal partners”, “primary partner”, and “regular partners”; regular condom use with sex clients; mean number of sexual partners; exit from sex work; and frequency of unprotected anal, vaginal, and oral sex. Other outcomes included household communication about HIV and sex, economic well-being, self-empowerment, and knowledge about physical and sexual violence. Four studies had both health and economic outcome measures [21, 22, 27, 28], while three had health only outcomes [23, 25, 26].
Female Sex Workers
All three sex worker studies showed reductions in sexual risk comparing the intervention and control groups [21, 26, 27]. All found significant reductions in the total number of sexual partners among sex workers. Small business training skills were associated with fewer sex trade partners per month among sex workers [21, 27]. Odek et al. [26] noted a significant decrease in the number of all regular sexual partners but not casual partners when compared to baseline (1.96 vs. 0.73 p < 0.01 and 1.43 vs. 1.12, p = 0.10, respectively). Condom use increased by nearly 20 % with regular partners during the intervention period. Condom use with sex trade clients was also increased in the intervention groups when compared to baseline data [21, 27].
Non-Sex Workers
Of the four analyses of the three non-sex worker studies, only one found a significant increase in condom use, although the study participants were not the index participants [23]. Pronyk et al. [23] found that unprotected sex at last intercourse with a non-spousal partner was significantly lower among the intervention group when compared to the comparison group. Rosenberg et al. [25] also noted a similar trend towards increased condom use with an unfaithful partner, although the finding was not significant. No differences were found in the number of sexual partners before and after the intervention [23, 25].
Income and Economic Empowerment
The financial gains made by the study participants through the microenterprise development interventions are listed in Tables 3 and 4. Of the three sex worker studies, two included microenterprise development interventions that involved small business training skills [21, 27] and the third was a microfinance program that provided loans to support small businesses [26]. Both small business training interventions resulted in improvements in higher overall income and lower income from selling sex [21, 27]. Higher income from jewelry sales was associated with a reduction in the number of sex trade partners at follow-up [27]. The microfinance intervention did not report income as an economic outcome measure, but noted that the majority (82.5 %) of women used the loans to engaged in trading businesses with food and retail commodities and 65.2 % had operational businesses at end-line survey [26]. Furthermore,45.4 %of the participants reported exiting from sex work at last follow up [26].
Table 3.
Microfinance economic outcomes
| First author (year) |
Use of loans | Multi- sectoral network (Y/N) |
Business training (Y/N) |
Mean number of loans taken per person during study period |
Median loan amount (USD) | Loan repayment scheme |
Loan repayment rate |
Economic outcome (self-report) |
|---|---|---|---|---|---|---|---|---|
| [22] | Loans used to support small businesses like selling fruit and vegetables, second hand clothes, and other products |
Y | Y | Combined microfinance + education group: 3 Microfinance only group: 4 |
Combined microfinance + education group: $150 Microfinance only group: $195 |
Group model: 5 women, fortnightly repayments |
N/A | Both combined intervention group and microfinance only group had improvements in self-reported economic well- being when compared to control. No differences in economic well-being between the two intervention groups |
| [26] | 1) 82.5 % of women used loans to support small businesses (selling fruits, cereals, vegetables, second hand clothes, retail shop merchandise) |
Y | Y | 1 | $200 | Group model: 5–15 women, weekly loan |
65 % | 65.2 % of women had operational businesses at end- line survey repayments |
| 2) 10 % of women used loans to sewing new clothes and produce fruit juices |
||||||||
| 3) 7 % of women used loans to support service businesses (hair salons, food kiosks) |
||||||||
| [23] | Loans used to support small businesses (selling fruits, vegetables, and second hand clothes) |
Y | Y | 4 (over 3 year period) | $386 | Group model: 5 women, biweekly loan repayments |
99.70 % | N/A |
| [25] | N/A | Y | Y | N/A | Initial loan: $75, each progressive loan is larger based on full repayment of previous loan, amount of money in savings account, and attendance at meetings |
Group model: 5 women, 3 month loan repayments |
N/A | No difference in amount of money spent per week between long intervention and short intervention groups |
Table 4.
Small business economic outcomes
| First author (year) |
Type of microenterprise development |
Nature of capacity building |
Multi- sectoral network (Y/N) |
Business training (Y/N) |
Loan repayment rate |
Intervention participation |
Small business profits |
Self-reported economic improvement |
|---|---|---|---|---|---|---|---|---|
| [27] | Small business/ skills training |
Making, marketing, and selling of jewelry |
Y | Y | N/A | 77 % | Median value of jewelry sold: $112.80 per woman |
IG had significantly lower sources of income from trading sex for drugs/ money: 100 vs 71 %, p <0.01 IG had significantly lower sources of income from selling drugs: 35 vs 10.5 %, p <0.01 |
| [21] | Small business/ skills training |
Tailoring and selling bags |
Y | Y | N/A | 75 % | Mean monthly income from bags sold: $85.00 |
IG had 41 % increase in average monthly income ($105.30 vs. $78.60, p <0.01) IG had significantly lower monthly earnings from sex work ($33.90 vs $54.90, p <0.01) |
| [28] | Microfinance and small business/skills training |
Soap making, tie-dye, candle making |
Y | Y | Partial repayment of loans at 6 months: 20 % Full repayment at 6 months: 6% |
80 % | N/A | Significantly more participants with own income than baseline (44 vs. 6 %, p <0.01) |
IG intervention group
Of the four analyses of the three non-sex worker studies, three incorporated microfinance interventions [22, 23, 25], and one was a combined program that included both microfinance and small business training [28]. Economic well-being was analyzed in two of the non-sex worker studies [22, 28], which showed increased income and savings [28] and improved self-reported economic well- being [22]. In one study with two intervention arms consisting of microfinance-only and combined microfinance and gender/HIV education, both programs reported improved economic well-being with no evidence that one type of intervention produced greater improvements [22]. Most of the loans were used to support small businesses such as selling fruits, vegetables, and second hand clothes. Rosenberg et al. [25] found that women with longer participation in the microfinance intervention were four times as likely to use condoms with unfaithful partners.
Gender Equality
Gender equality indicators were reported in four of the seven studies, and included various measures such as self- reported relationship power and level of communication with household members about sex (Table 5). Overall, all four studies reported greater gender equality in the microenterprise development intervention participants. None of the three sex workers studies had gender equality indicators. Of the non-sex worker studies, increased relationship power and communication about sex were recurring themes [22, 23, 25, 28]. The sense of self-empowerment extended to the household and community levels as well, as illustrated by a decrease in partner infidelity [25] and increased solidarity in the face of a crisis [22].
Table 5.
Gender equality indicators
| First author (year) |
Indicator of gender equality | Self-reported outcome | IPV outcome |
|---|---|---|---|
| [26] | N/A | N/A | N/A |
| [27] | N/A | N/A | N/A |
| [21] | N/A | N/A | N/A |
| [22] | O.1) Individual level empowerment (greater self- confidence, financial confidence, challenges gender norms O.2) Household level empowerment (supportive partner relationship, autonomy in decision making, perceived contribution to household) O.3) Community level empowerment (larger social network, community support, increased solidarity) |
Trend of increased empowerment at individual, household, and community level in IG vs. control O.1) No significant changes in individual level empowerment O.2) Increased supportive partner relationship in combined intervention vs. MF only intervention (aRR = 1.37, CI = 1.09–2.71) Increased perceived contribution to household in combined intervention vs. MF and control (aRR = 1.83, CI = 1.35–2.51; aRR = 1.73, CI = 1.19–2.53; respectively) O.3) Increased solidarity in combined intervention vs. MF only intervention (aRR = 1.43; CI = 1.11–1.83) |
Decreased IPV combined intervention vs. control (aRR = 0.51, CI = 0.28–0.93) |
| [23] | O.1) Female headed household O.2) Communication with household members about sex in past 12 months O.3) Qualitative changes in HIV risk behavior |
O.1) No difference proportion of female headed households O.2) Increased communication about sex in household (aRR = 1.46, CI = 1.01–2.12) O.3) Sense of increased bargaining power among intervention participants |
N/A |
| [25] | O.1) Relationship power (mean general power index range 0–10) O.2) Partner infidelity |
O.1) Increased relationship power index in IG compared to baseline (p <0.01) O.2) Decreased partner infidelity in IG compared to baseline (p < 0.01) |
N/A |
| [28] | O.1) Relationship power in sexual relationship O.2) Relationship power in nonsexual romantic relationship |
O.1) No difference found in relationship power in sexual relationship between IG and baseline (p = 0.16) O.2) Increased relationship power in non-sexual romantic relationship between IG and baseline (p = 0.04) |
Baseline: 20 % reported violence, 14 % reported sexual violence or rape IG: 16 % reported violence, 8 % reported sexual or rape |
MF microfinance, IG intervention group, IPV intimate partner violence
Intimate partner violence (IPV) was measured in two studies. Kim et al. [22] found a general trend towards decreased IPV experience in both the combined intervention and microfinance-only intervention groups, but only the combined intervention effect was statistically significant when compared to control. Dunbar et al. [28] noted that participants experienced IPV at both baseline and during the intervention, although no statistical tests were performed due to the different reporting timeframes.
Multi-Sectoral Involvement
Multi-sectoral collaboration was present in all seven studies. All micro-lending studies in this review worked with local non-governmental organizations (NGOs) that acted as partner microfinance institutions. The small business skills training interventions also involved multi-sectoral partnerships with local community-based organizations that had varying roles in the implementation and assessment phases. A non-profit foundation was created solely to manage the sale of bags created by female sex workers in India to ensure sustainability [21]. Multiple NGOs, including the Baltimore Syringe Exchange Program, were engaged in the recruitment of sex workers for the jewelry-making program [27]. Three studies also incorporated peer-education schemes and encouraged community mobilization [22, 23, 26].
Discussion
Historically, microenterprise development interventions have been primarily used as poverty reduction tools through the creation of new businesses. Increasingly, researchers are investigating the application of microenterprise development to HIV prevention efforts by boosting women’s economic independence and increasing their negotiating power in conditions that may increase HIV risk and through a direct income effect, reduce their need to rely on transactional sex. Indeed, several studies have found positive effects of microfinance on household economic outcomes, such as per-capita consumption, ownership of durable goods, creation of new businesses, and labor supply [15]. However, the effects of microenterprise development have been critically challenged in recent literature [13, 15, 16], and the effects of microenterprise development on HIV/STI prevention have not been systematically documented. To our knowledge, this is the first systematic review of the effect of microenterprise development interventions on HIV/STIs. Our review extends previous research [3, 4, 9] by including quantitative data, assessing study quality, exploring implementation, and community-based organization involvement.
Microenterprise development interventions show promise for reducing sexual risk behaviors among female sex workers. All sex worker studies showed significant reductions in number of sex partners, and two of the three studies showed reductions in unsafe sex. The exception was the randomized controlled trial by Sherman et al. [21], which showed no difference in condom use between the control and intervention arms. This may be attributed to the concurrent comprehensive HIV prevention programs targeting female sex workers in Chennai, India at the time of intervention. Risk reduction can be the result of increased women’s empowerment secondary to greater decision-making authority or better labor market outcomes for women as well as increased economic security. For some women, microenterprise development can bring about positive changes in these domains and reduce their HIV vulnerability. The mechanism underlying the microenterprise development models that included combinations of credit-led and training-led programs likely revolved around increased income through increased opportunities, income diversification, and non-monetary benefits, such as wider social networks and a sense of self-worthiness [4]. Increased monthly income was reported in both small business skills training studies, and participants in the microfinance intervention reported greater job self-efficacy. Given that economic disadvantage may create a setting that promotes risky sexual behaviors such as transactional sex [4, 9], alternative income opportunities may empower female sex workers to engage in less risky sexual behaviors or stop or reduce selling sex [26]. None of the sex worker studies included gender equality indicators, but several studies have documented that microenterprise development increased bargaining ability and control over financial and non-financial assets in women [29].Of note, the interventions comprised of education- and microenterprise development-related components, which underscores the multi-dimensionality of the mechanisms underlying HIV/ STI risk reduction.
Among non-sex workers, the evidence for microenterprise development in decreasing risky sexual health behaviors is more limited. Despite increased self-reported sense of empowerment and gender equality in all the studies, only one study found reductions in unsafe sex [23] and none found evidence for decreased number of sex partners. There is no clear direct relationship between empowerment and reductions in sexual risk behavior, and this may be partly driven by the negative consequences of participation, such as gender-based violence [28]. The nature of the relationship between sex partners of non-sex workers is likely to be different than that of sex workers, thus accounting for the difference in the observed outcomes. However, because only a small percentage of non-sex workers reported having more than one sexual partner, the lack of significance may be the result of underpowered studies [23, 25]. Notably, the women who had longer participation in the microenterprise development intervention reported increased relationship power and less partner infidelity, suggesting that long-term exposure to microfinance may allow women to negotiate equality in relationships [25]. These women were also more likely to use condoms when their partners were perceived to be unfaithful [25]. It is possible that the women who have longer exposure to microfinance also have qualities that enable them to more freely exercise their relationship power and control over reproductive health decisions. Women who self-select into the microfinance initiatives also may be more self-sufficient and empowered, thus minimizing the effects on length of intervention exposure on sexual health behavior. Indeed, Rosenberg et al. noted a high one-year client retention rate of over 93 %, suggesting the possibility that any observed differences may be due to underlying traits of the participants in addition to length of experience [25]. Given the lack of consistent validated gender equality measures in the reviewed interventions, it is not surprising that the mechanisms leading to reduced sexual health risk remain unclear. This above highlights the need for validated measures of women’s empowerment such as the Sexual Relationship Power Scale (SRPS) [30] in future HIV/STI prevention studies to improve our understanding of the role microenterprise development plays in achieving gender equity.
These studies address the critical role of community-based organization collaboration and multi-sectoral input in microenterprise development interventions [7]. Local involvement of most-at-risk populations should be integral to program design to increase community ownership and relevance [5]. The roles of the involved organizations varied greatly depending on program needs and the individualized strengths of the community. Due to the complex structural factors underlying HIV transmission, comprehensive HIV prevention tactics must incorporate approaches at multiple levels of influence and utilize the expertise of different sectors to achieve the maximum reductions in HIV risk.
All of the microenterprise development studies excluded men, consistent with much of the microenterprise development literature [3, 4, 17, 31–33]. Contrary to previous reports on the greater impact of microenterprise development interventions on women than men [11, 34], recent evidence from Sri Lanka suggests that men may have higher returns on capital investments than women [35, 36]. Repayment rates on loans are often higher by women, possibly due to the more risk averse nature and, in the context of group lending, increased susceptibility to pressure from peers in women [37]. However, evaluations of credit programs in rural Bangladesh reveal that over 60 percent of the small loans given to women are controlled by their husbands [38]. In some cases, perceptions of improved economic standing or the intense pressures on loan repayment may spur physical and sexual violence, increasing the risk of HIV transmission [28]. These unintended consequences demonstrate the risks of microcredit development, particularly in the setting of unstable economic environments and poor social support [28], and may contribute to an overestimation of the benefits of microenterprise development. Although most HIV prevention interventions targeting men address gender inequities through education [39–41], there are a few microenterprise development models that also incorporate men [37]. Through a participatory approach, the male household heads can be incorporated into the microenterprise development program design with the female participants. Through partner support education and dual participation in the needs assessment, household frictions may decrease and economic goals may be achieved more easily [37]. However, the effects of incorporating men in microenterprise development interventions on decreasing HIV risk and vulnerability have not been thoroughly examined and merit further research.
There are several limitations to this systematic review. First, the small number of studies included in this literature review warrants careful considerations when drawing conclusions and highlights the necessity for more empirical evidence. The quality assessment measurement allowed comparison of both randomized controlled trials and observational studies, although this comparative metric was not exhaustive. Only one study was a randomized controlled trial that showed limited effects of microenterprise development on sexual risk behaviors, and many of the other studies had self-selection biases. Second, distinguishing the effects of microenterprise development is difficult in the setting of comprehensive interventions. Kim et al. [22] found that microenterprise development alone contributed to a greater sense of economic well-being and self-empowerment as well as increased condom use, although the positive effects were not significant in empowerment and HIV risk-related behavior. Indeed, the addition of the educational component may be necessary to propagate benefits of microenterprise development. Furthermore, the effects of a combined microenterprise development program that includes microfinance, financial literacy training, and education have not been evaluated. Third, the sexual health behavior outcomes were heterogeneous and no studies included biomarker outcomes. Fourth, the individual differences in baseline entrepreneurial inclination may obscure the effect of microenterprise development interventions. The non-experimental studies are subject to selection bias, and it is possible that there are unmeasured differences that may affect the success of microenterprise development between the intervention and control groups.
Microenterprise development has the potential to bring about coordinated impacts in increasing income and savings, empowering women, and reducing intimate partner violence. Although these factors are intricately tied to HIV risk reduction, the current understanding of the mechanisms underlying microenterprise development and its implementation and assessment processes in these efforts is still quite limited. Our study demonstrated how local multi-sectoral networks and community-based organizations helped to implement microenterprise development interventions. To better understand the potential of microenterprise development in reducing HIV/STI risk, future studies must focus on four components. First, randomized control trials are necessary to eliminate selection biases mentioned above. Second, additional biological outcomes such as HIV/STI incidence would allow for a more robust interpretation of the data. Third, we must recognize that successful approaches in one geographic region do not equate success in others. Study designs and evaluations must be replicated in a variety of locations with the appropriate social, cultural, and political contexts. Finally, the conceptual mechanisms underlying microenterprise development in HIV/STI prevention must be explored more thoroughly, as the current understanding of low-income household choices in the face of changing financial incentives is limited. Given the heterogeneity in the types of microenterprise development as well as the individual differences in entrepreneurial proclivity, further research and programs are needed in order to clarify how microenterprise development can be an effective component of a comprehensive HIV control strategy.
Acknowledgments
All authors assisted with analysis and interpretation of the data, reviewed the manuscript for important intellectual content, and provided final approval of the version submitted for publication. Special thanks to the UNC Center for AIDS Research, Guangdong Provincial STD Control Center and UNC Project-China for administrative support. The authors would also like to thank Rebecca Martinez and Oscar Galagarza for the Spanish translation of the abstract.
Footnotes
Conflicts of interest The authors have no conflicts of interest.
Contributor Information
Rosa R. Cui, Email: rrc2126@columbia.edu, Columbia University College of Physicians and Surgeons, UNC Project-China, 60 Haven Ave. Apt 17D, New York, NY 10032, USA.
Ramon Lee, Harvard Medical School Boston, Boston, MA, USA.
Harsha Thirumurthy, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Kathryn E. Muessig, University of North Carolina at Chapel Hill, School of Medicine, UNC Project-China, Chapel Hill, NC, USA
Joseph D. Tucker, University of North Carolina at Chapel Hill, School of Medicine, UNC Project-China, Chapel Hill, NC, USA
References
- 1.Gillespie S, Kadiyala S, Greener R. Is poverty or wealth driving HIV transmission? AIDS. 2007;21(Suppl 7):S5–S16. doi: 10.1097/01.aids.0000300531.74730.72. [DOI] [PubMed] [Google Scholar]
- 2.Greig A, Peacock D, Jewkes R, Msimang S. Gender and AIDS: time to act. AIDS. 2008;22(Suppl 2):S35–S43. doi: 10.1097/01.aids.0000327435.28538.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim JC, Watts CH, Hargreaves JR, et al. Understanding the impact of a microfinance-based intervention on women’s empowerment and the reduction of intimate partner violence in South Africa. Am J Public Health. 2007;97(10):1794–1802. doi: 10.2105/AJPH.2006.095521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stratford D, Mizuno Y, Williams K, Courtenay-Quirk C, O’Leary A. Addressing poverty as risk for disease: recommendations from CDC’s consultation on microenterprise as HIV prevention. Public Health Reports. 2008;123(1):9–20. doi: 10.1177/003335490812300103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 6.UNAIDS. Combination HIV prevention: tailoring and coordinating biomedical, behavioral, and structural strategies to reduce new HIV infections. A UNAIDS discussion paper. 2010 [Google Scholar]
- 7.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372(9639):669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pronyk PM, Hargreaves JR, Kim JC, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin SL, Blankenship K. Microfinance and HIV/AIDS prevention: assessing its promise and limitations. AIDS Behav. 2009;13(3):462–469. doi: 10.1007/s10461-009-9532-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim J, Pronyk P, Barnett T, Watts C. Exploring the role of economic empowerment in HIV prevention. AIDS. 2008;22(Suppl 4):S57–S71. doi: 10.1097/01.aids.0000341777.78876.40. [DOI] [PubMed] [Google Scholar]
- 11.Khandker S. Microfinance and poverty: evidence using panel data from Bangladesh. Vol 19. Oxford University Press; 2005. [Google Scholar]
- 12.Glossary of Microfinance Related Terms. 2012 http://www.accion.org/page.aspx?pid=257-m.
- 13.Chowdhury A. Microfinance as a poverty reduction tool—a critical assessment. Vol DESA Working Paper No. 892009 [Google Scholar]
- 14.Karlan D, Murdoch J. Access to finance. Vol 52009 [Google Scholar]
- 15.Banerjee AV, Duflo E, Glennerster R, Kinnan C. The miracle of microfinance? [Accessed April 14];Evidence from a randomized evaluation. 2013 [Google Scholar]
- 16.Robinson M. The microfinance revolution: sustainable finance for the poor. Washington DC: The World Bank; 2001. [Google Scholar]
- 17.Johnson S. Gender impact assessment in microfinance and microenterprise: why and how. Dev Pract. 2000;10(1):89–93. doi: 10.1080/09614520052547. [DOI] [PubMed] [Google Scholar]
- 18.Auerbach J. Transforming social structures and environments to help in HIV prevention. Health affairs (Project Hope) 2009;28(6):1655–1665. doi: 10.1377/hlthaff.28.6.1655. [DOI] [PubMed] [Google Scholar]
- 19.Hankins CA, de Zalduondo BO. Combination prevention: a deeper understanding of effective HIV prevention. AIDS. 2010;24(Suppl 4):S70–S80. doi: 10.1097/01.aids.0000390709.04255.fd. [DOI] [PubMed] [Google Scholar]
- 20.Vergidis PI, Falagas ME. Meta-analyses on behavioral interventions to reduce the risk of transmission of HIV. Infect Dis Clin North Am. 2009;23(2):309–314. doi: 10.1016/j.idc.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Sherman SG, Srikrishnan AK, Rivett KA, Liu SH, Solomon S, Celentano DD. Acceptability of a microenterprise intervention among female sex workers in Chennai India. AIDS and behavior. 2010;14(3):649–657. doi: 10.1007/s10461-010-9686-z. [DOI] [PubMed] [Google Scholar]
- 22.Kim J, Ferrari G, Abramsky T, et al. Assessing the incremental effects of combining economic and health interventions: the IMAGE study in South Africa. Bull World Health Organ. 2009;87(11):824–832. doi: 10.2471/BLT.08.056580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pronyk PM, Kim JC, Abramsky T, et al. A combined microfinance and training intervention can reduce HIV risk behaviour in young female participants. AIDS. 2008;22(13):1659–1665. doi: 10.1097/QAD.0b013e328307a040. [DOI] [PubMed] [Google Scholar]
- 24.West S. Systems to rate the strength of scientific evidence. Evidence Report/Technology Assessment No. 47 (Prepared by the Research Triangle Institute- University of North Carolina Evidence-based Practice under Contract No. 290-97-0011) AHRQ Publication No.02-E016. 2002 Apr [Google Scholar]
- 25.Rosenberg MS, Seavey BK, Jules R, Kershaw TS. The role of a microfinance program on HIV risk behavior among Haitian women. AIDS Behav. 2011;15(5):911–918. doi: 10.1007/s10461-010-9860-3. [DOI] [PubMed] [Google Scholar]
- 26.Odek WO, Busza J, Morris CN, Cleland J, Ngugi EN, Ferguson AG. Effects of microenterprise services on HIV risk behaviour among female sex workers in Kenya’s urban slums. AIDS Behav. 2009;13(3):449–461. doi: 10.1007/s10461-008-9485-y. [DOI] [PubMed] [Google Scholar]
- 27.Sherman SG, German D, Cheng Y, Marks M, Bailey-Kloche M. The evaluation of the JEWEL project: an innovative economic enhancement and HIV prevention intervention study targeting drug using women involved in prostitution. AIDS care. 2006;18(1):1–11. doi: 10.1080/09540120500101625. [DOI] [PubMed] [Google Scholar]
- 28.Dunbar MS, Maternowska MC, Kang MS, Laver SM, Mud-ekunye-Mahaka I, Padian NS. Findings from SHAZ!: a feasibility study of a microcredit and life-skills HIV prevention intervention to reduce risk among adolescent female orphans in Zimbabwe. J prev interv community. 2010;38(2):147–161. doi: 10.1080/10852351003640849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Isangula KG. Improving women and family’s health through integrated microfinance, health education and promotion in rural areas. J Sustain Develop. 2012 [Google Scholar]
- 30.Pulerwitz J. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7/8):637–660. [Google Scholar]
- 31.Coppock DL, Desta S, Tezera S, Gebru G. Capacity building helps pastoral women transform impoverished communities in Ethiopia. Science. 2011;334(6061):1394–1398. doi: 10.1126/science.1211232. [DOI] [PubMed] [Google Scholar]
- 32.Isangula KG. Improving women and family’s health through integrated microfinance, health education and promotion in rural areas. J Sustain Develop. 2012;5(5):76–89. [Google Scholar]
- 33.Mayoux L. Women’s empowerment and microfinance programmes: strategies for increasing impact. Dev Pract. 1998;8(2):235–241. doi: 10.1080/09614529853873. [DOI] [PubMed] [Google Scholar]
- 34.Pitt M, Khandker S. The impact of group—based credit programs on poor households in Bangladesh: does the gender of participants matter? J Political Econ. 1998;106(5):958–996. [Google Scholar]
- 35.de Mel S, McKenzie D, Woodruff C. Are women more credit constrained? Experimental evidence on gender and microenterprise returns. Am Econ J: Appl Econ. 2009;1(3):1–32. [Google Scholar]
- 36.de Mel S, McKenzie D, Woodruff C. Returns to capital in microenterprise: evidence from a field experiment. Q J Econ. 2008;123(4):1329–1372. [Google Scholar]
- 37.Armendariz B. Gender empowerment in microfinance. Harvard University; 2008. [Google Scholar]
- 38.Goetz S, Gupta R. Who takes the credit? gender, power, and control over loan use in rural credit programs in Bangladesh. World Dev. 1996;24(1):45–63. [Google Scholar]
- 39.Jewkes R, Nduna M, Levin J, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ (Clinical research ed.) 2008;337:a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pulerwitz J, Michaelis A, Verma R, Weiss E. Addressing gender dynamics and engaging men in HIV programs: lessons learned from Horizons research. Public health reports. 2010;125(2):282–292. doi: 10.1177/003335491012500219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verma RK, Pulerwitz J, Mahendra V, et al. Challenging and changing gender attitudes among young men in Mumbai, India. Reproductive health matters. 2006;14(28):135–143. doi: 10.1016/S0968-8080(06)28261-2. [DOI] [PubMed] [Google Scholar]