Abstract
Nicotine dependence (ND) and major depression (MD) are highly prevalent disorders that frequently co-occur. Less is known about which aspects of ND are most strongly associated with MD. The present study was designed to determine if subtypes of smokers exist and differ in their risk of MD and lifetime MD symptoms. Latent class analysis was used to identify profiles of DSM-IV ND criteria for 8,842 daily smokers drawn from the larger 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). We found evidence for 4 distinct subtypes of smokers mainly characterized by increasing levels of ND severity, by number of criteria endorsed. We found a dose–response relationship between classes by increasing ND severity and odds of past-year MD and lifetime depression criteria. Class 2 was characterized by higher symptom endorsement probabilities (SEPs) for wider range of ND criteria and a higher odds of MD (OR = 3.66) compared to class 3, which was characterized by higher SEPs for physiological ND criteria, higher prevalence of ND (class 2, 71.50% vs. class 3, 81.57%), and a lower odds of MD (OR = 2.15). A post hoc contrast showed these two distinct classes of respondents with mild to moderate ND significantly differed in their likelihood of MD comorbidity (F = 12.25, 1 df, p = 0.0008). ND severity mainly characterized the classes, but unique differences may exist between smokers with mild to moderate ND. Individuals with symptom profiles not characterized by physiological dependence endorse wider range of ND criteria and have a higher likelihood of MD.
Keywords: Latent class analysis, Co-occurring disorders, Nicotine dependence, Major depression, Psychiatric epidemiology
1. Introduction
The frequent co-occurrence of nicotine dependence (ND) and major depression (MD) over the life-span has been well established (Grant et al., 2004; Jorm, 1999; Kessler et al., 2005). The national estimate from the NESARC of current MD among those with current ND is 30.01% (Grant et al., 2004), which is much higher than the estimated prevalence (5.8%) of current MD in the general population (Hasin et al., 2005). Despite a large literature on the co-occurrence of ND and MD, the etiologic relationship between these disorders remains under investigation and the precise nature of this comorbidity has not been agreed upon by researchers. Elucidation of this connection is crucial for developing effective strategies for prevention efforts and interventions.
The present analysis was designed to explore the association between ND and MD by examining the criteria for each disorder, in order to identify which aspects of ND are most strongly associated with MD. DSM-IV defined ND and MD (APA, 1994) are syndromal disorders and individuals who meet criteria for these disorders can have unique symptom configurations. As such, there may be specific ND symptom profiles that increase the odds of MD and the likelihood of experiencing specific MD symptoms. While this has not been empirically established, related research points to possible explanations for symptom level associations between the disorders (Madden et al., 1997; Xian et al., 2007, 2005).
First, it may be the behavioral symptoms of DSM-IV defined ND that underlie the well-established association between ND and MD (Breslau and Johnson, 2000). Breslau and Johnson (2000) found that the association between ND and MD differed for ND as defined by the Fagerstrom Test for Nicotine Dependence (FTND) (Heatherton et al., 1991) and the DSM-III-R, finding a three-fold risk for depression among dependent persons using DSM-III-R criteria, but no association using the FTND criteria. The two measures differ on symptom emphasis and may diagnose different types of smokers (Moolchan et al., 2002); the FTND highlights symptoms of physiological dependence, whereas 6 of the 9 DSM-III-R criteria (definition assessed in the 2000 Breslau & Johnson study) are behavioral and focused on psychological indicators of diminished control over smoking. While the physiological and behavioral symptoms cannot be examined separately, latent class analysis (LCA) allows for the investigation of which configurations of ND symptoms are most strongly associated with MD. Using LCA, empirically derived distinct subgroups of smokers are formed based on common configurations of ND symptoms; these subgroups may have different associations with MD.
Rather than being characterized qualitatively by behavioral symptoms, it is also possible that the association between ND and MD is quantitatively characterized by increasing severity; with increasing ND severity comes an increase in the likelihood of MD comorbidity. Previous latent class analyses of ND have found 3 and 4 class solutions characterized by a quantitative continuum of increasing severity (Storr et al., 2004a,b; Xian et al., 2007), with severity defined by number of criteria endorsed. The results of these studies suggest that there are identifiable latent subtypes of ND and that these can be characterized quantitatively by a severity index, with one class representing those endorsing almost no dependence criteria and the third or fourth class representing those endorsing all seven DSM-IV dependence criteria. The only study that we are aware of that examined the association between classes of lifetime dependence criteria and MD found a dose–response relationship between 4 classes of increasing ND severity and MD (Xian et al., 2007). The samples for these past studies were comprised of young adults or middle-aged men; it is unknown whether this quantitative class characterization exists for the broader U.S. adult population.
Past-year DSM-IV ND criteria data for past-year smokers who reported ever smoking daily from the 2001–2002 NESARC sample (n = 8,842) were utilized for the analyses. The NESARC data allow for the construction of DSM-IV diagnoses and contains detailed and extensive tobacco use (including ND symptoms) and low mood sections (including MD symptom assessment). These data allowed us to explore the following research questions on the relationship between DSM defined ND and MD: (1) do empirically derived and meaningful subtypes of smokers exist? (2) If so, are these classes characterized quantitatively, by increasing severity, or do they differ qualitatively, with different configurations of ND criteria? To explore the concurrent and predictive validity of these subtypes of smokers, we asked: (3) do respondents in these latent classes differ with respect to prevalence of MD and ND and related characteristics? And, (4) do certain classes have higher odds of MD and lifetime MD criteria?
2. Method
2.1. Study population and data collected
The 2001–2002 National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) consists of cross-sectional data obtained through a survey administered to a nationally representative sample of 43,093 U.S. adults. The NESARC was sponsored and conducted by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and has detailed assessments of alcohol use disorders, other substance abuse and dependence, and a wide range of Axis I and II psychiatric disorders.
The target population for the NESARC sample was the civilian non-institutionalized population, aged 18 years and older, residing in the United States and District of Columbia (including Alaska and Hawaii). Additionally, the following non-institutional group quarters housing units were included as part of the sample: boarding houses, rooming houses, non-transient hotels and motels, shelters, facilities for housing workers, college quarters, and group homes. Blacks and Hispanics were oversampled so that there were sufficient sample sizes from which to form national estimates of groups defined by race and ethnicity. Young people aged 18–24 were also oversampled for the NESARC survey, as accurate estimates from this demographic group were of particular interest and this population is particularly vulnerable with respect to alcohol use and abuse/dependence. The study population for the present analyses is a subpopulation of the whole NESARC sample, i.e. respondents who reported having ever smoked daily, having smoked cigarettes in the past year, and had no missing data on any ND and MD criteria (N = 8,842). We limited the analyses to past-years smokers and analyzed past year diagnoses for ND and MD in order to make the smoking behavior and diagnoses for ND and MD time-congruent.
2.2. Assessment and measures
This survey employed a multi-stage sampling design to yield data for establishing national estimates for mental and physical health conditions and risk factors. The NESARC data were collected over a 2-year period via computer assisted personal interviewing (CAPI), and the survey software included built-in skip patterns and logic and consistency checks. The overall response rate for the NESARC was 81%. Additional information about the sampling methodology and administration of the NESARC has been reported elsewhere (Grant et al., 2003b).
The survey instrument for the NESARC is the Alcohol Use Disorder and Associated Disability Interview Schedule–DSM-IV version (AUDADIS-IV). The AUDADIS-IV utilizes DSM-IV diagnostic criteria to identify a wide range of Axis I and II disorders. To receive a formal DSM-IV diagnosis of ND or MD a respondent needed to endorse a requisite number of criteria for the disorders and, for MD, report the presence of social and/or occupational dysfunction. In addition to diagnostic variables for the two disorders of primary interest, the AUDADIS-IV contains extensive data on tobacco use. All respondents answered questions in these sections, and none were ‘screened out’, as is the practice with some similar surveys (Kessler et al., 2004).
The test–retest reliability of the AUDADIS-IV was examined in a sub-sample of 2657 NESARC respondents in groups of 400 respondents for each test (Grant et al., 2003a). The reliability was found to be excellent for alcohol and other substance use, abuse and dependence (kappa = 0.74) assessment. Tobacco use items had good to excellent reliability with high intraclass correlation coefficients (ICC range: 0.60–0.92), and the tobacco dependence diagnoses for lifetime (kappa = 0.60) and past year (kappa = 0.63) were somewhat lower. The reliabilities associated with past year and lifetime withdrawal and dependence criteria were very good, with intraclass correlation coefficients ranging from 0.75 to 0.77 (Grant et al., 2003a). The reliability of DSM-IV MD diagnoses was similar, with good reliability for lifetime (kappa = 0.65) and past year (kappa = 0.59) diagnoses.
The central dependent variables of interest for multivariate analyses were current (i.e. past-year) MD and lifetime MD symptoms; these are represented as dichotomous presence/absence variables, allowing us to explore the association between the empirically derived latent classes of ND and facets of MD. We utilized the hierarchical MD diagnosis for analyses, which excluded depression that was substance-induced or due to a general medical condition (APA, 1994). The MD criteria analyzed for the present study are lifetime symptoms, as temporally specific information linking MD symptom configurations to specific depressive episodes was unavailable.
The seven criteria of DSM-IV ND were used as the manifest variables for the latent class analyses. Scoring algorithms for grouping the AUDADIS-IV items into dependence symptoms, and the symptoms into criteria for ND diagnoses, were obtained from the NIAAA group that developed and conducted the NESARC (B.F. Grant, April 20, 2007). ND criteria were constructed from 23 items in the ‘tobacco use’ section of the AUDADIS-IV. These items operationalized the following DSM-IV substance dependence criteria: tolerance, withdrawal, unintended increased use, inability to decrease or cease use, a large amount of time spent using tobacco, activities given up because of tobacco use, and continuing tobacco use in spite of having health problems due to the substance. For example, the symptom ‘a large amount of time spent obtaining, using, or recovering from the effects of tobacco’ was operationalized by a single item, ‘find yourself chain smoking one right after another?’, and the tolerance criteria was operationalized by two items, ‘find that you had to use much more tobacco than you once did to get the effect you wanted?’ and ‘increase your use of tobacco by at least 50%?’. Respondents needed to endorse at least 3 of the 7 criteria, occurring at any time in the same 12-month period, to be assigned a diagnosis of ND. Although the tolerance and withdrawal criteria can be each be defined or manifested by two different symptoms, the other five criteria each correspond directly with one symptom.
2.3. Statistical methods
Design effects of the NESARC require the use of special variance estimation procedures to accurately derive standard errors. Statistical analyses were conducted using SUDAAN (RTI, 2004), and Mplus software (Muthén and Muthén, 1998–2004). SUDAAN was used for the cross-tabulations, analyses of variance (ANOVA), and logistic regression analyses; latent class models were built with Mplus. SUDAAN and Mplus take into account the complex sampling design of the NESARC. The sample results are weighted to represent national sample estimates obtained from the 2000 Census and to account for the survey design characteristics, such as stratification and non-response.
2.4. Latent class analysis
We employed LCA (Hagenaars and McCutcheon, 2002; McCutcheon, 1987) to determine whether empirically derived typologies of ND symptoms exist among daily smokers, given respondents’ response profiles for the presence/absence of the seven DSM-IV ND criteria. This statistical method uses manifest variables (e.g. ND criteria) as indicators of a latent variable, of which the produced classes represent different levels. LCA uses an iterative process based on maximum likelihood estimation. First, a one class solution is fit, which corresponds with the null hypothesis that all respondents belong to the same latent class and that there are no distinct latent subtypes. Then, more classes are added until a solution is found that describes the data well. To identify the best model we used a conventional evaluation technique of comparing Bayesian Information Criteria (BIC) statistics, which provides an optimal combination of a low number of classes with a good fit. The class solution with the smallest BIC statistic is chosen as the most parsimonious yet well-fit solution. Upon selection of a satisfactory class solution, respondents were assigned class memberships based on the probability of their response profile to the seven ND criteria.
We examined the two sets of parameter estimates that were generated for the final model: (1) class membership probabilities, which are analogous to prevalence, and (2) symptom endorsement probabilities (SEPs), which are endorsement probabilities for symptoms by an individual respondent, given the respondent’s membership in that class.
2.5. LCA validators
To obtain validity estimates of the latent class structure the latent classes were analyzed for significant differences with respect to related variables. The following variables were selected as validators: prevalence of past-year ND, average age of onset of daily smoking, average number of cigarettes smoked when a daily smoker, average age of onset of ND, and prevalence of past-year MD. The significance level was set at p < 0.05; significance tests were then conducted using the chi-square test for the association between assigned class and prevalence of past-year MD and ND, and overall F-tests for mean differences across classes for the continuous validators.
2.6. Multivariable modeling
Adjusted logistic regression models were fit to examine the association between the identified classes and endorsement of lifetime MD criteria using indicator variables for each of the latent classes. Binary logistic regression models were adjusted for the following sociodemographic characteristics: age, sex, education (less than high school, completed high school, some college, and completed college or higher), and race (White, Black, Native American, Asian, and Hispanic). Odds ratios for MD characteristics based on class membership status were generated, along with the reporting of 95% confidence intervals.
3. Results
3.1. Sociodemographic characteristics
Table 1 depicts frequencies of sociodemographic characteristics, ND criteria, and past-year psychopathology for the NESARC sample and for the subpopulation used for analyses in the present study. Respondents with valid data for all ND and MD criteria were included in the analyses. The conditional probability of past-year MD among the selected subpopulation of daily smokers was 12.03%, whereas the prevalence was 7.06% for the larger NESARC sample; of past-year ever-daily smokers, 52.83% met diagnostic criteria for past-year ND. Among the sample selected for the latent class analyses, the most commonly reported clinical features of ND experienced in the past 12-months were withdrawal (76.08%) and desire or unsuccessful efforts to cut down or control smoking (65.38%). A majority of these respondents (53.97%) also reported continuing smoking despite physical or psychological problems that were caused by or worsened by their tobacco use.
Table 1.
Sociodemographic characteristics and prevalence of nicotine dependence-related items.
| Total Sample (N = 43, 093)
|
Past-Year Ever Daily Smokers (n = 8,842)
|
|||
|---|---|---|---|---|
| % | S.E. | % | S.E. | |
| Sex | ||||
| Male | 47.92 | 0.31 | 53.18 | 0.63 |
| Female | 52.08 | 0.31 | 46.82 | 0.63 |
| Age | ||||
| 18–32 | 27.69 | 0.42 | 33.29 | 0.65 |
| 33–44 | 25.00 | 0.31 | 27.50 | 0.58 |
| 45–59 | 25.70 | 0.29 | 27.13 | 0.60 |
| 60+ | 21.61 | 0.36 | 12.08 | 0.38 |
| Race | ||||
| White | 70.89 | 1.59 | 76.25 | 1.11 |
| Black | 11.07 | 0.64 | 10.14 | 0.65 |
| Native American | 2.12 | 0.16 | 3.18 | 0.29 |
| Asian | 4.36 | 0.53 | 2.46 | 0.43 |
| Hispanic | 11.56 | 1.23 | 7.97 | 0.72 |
| Past 12-month Major Depression | 7.06 | 0.20 | 12.03 | 0.45 |
| Past 12-month Nicotine Dependence | 12.76 | 0.39 | 52.83 | 0.73 |
| Past-Year Nicotine Dependence Criteria | ||||
| Tolerance | 4.09 | 0.16 | 17.00 | 0.54 |
| Withdrawal | 18.52 | 0.52 | 76.08 | 0.75 |
| Smoked more or over a longer period than intended | 6.43 | 0.24 | 26.21 | 0.69 |
| Desire or unsuccessful efforts to cut down or control smoking | 16.55 | 0.42 | 65.38 | 0.66 |
| Great deal of time spent smoking | 5.85 | 0.22 | 23.67 | 0.60 |
| Activities given up or reduced because smoking is not allowed | 2.20 | 0.11 | 9.26 | 0.39 |
| Continued smoking despite physical or psychological problem caused or worsened by smoking | 13.24 | 0.37 | 53.97 | 0.74 |
Note: N is based on unweighted data; % represents weighted percentages. Percentages may not sum to 100 due to rounding.
3.2. Model selection and latent class descriptions
The model results are displayed in Table 2, with the selected model indicated in bold. We identified a four-class solution as the best-fitting latent class structure, as indicated by the smallest BIC value (BIC = 59,139.908) among the fitted models and the greatest reduction in value from the null one-class solution (ΔBIC = 7649.047). Fig. 1 shows the SEPs for each of the seven past-year DSM-IV ND criteria, charted for the four identified classes. 37.69% of past-year ever-daily smokers were assigned to class 1, 7.41% to class 2; class 3 was the largest, with 39.97% of respondents included for analysis assigned to that class, and class 4 comprised 14.93% of the sample. The symptom ‘withdrawal’ was the most prevalent and had the highest SEPs across the classes, ranging from 0.459 for class 1 to 0.998 for class 2. Similar to previous latent class research on ND criteria (Xian et al., 2007), the least endorsed symptom across the classes was ‘giving up or reducing activities because of smoking.’ Class 1, the low dependence subtype, was characterized by low SEPs for each of the criteria, with only moderate probabilities for ‘withdrawal’ and ‘desire or unsuccessful efforts to cut down’. Descriptively, this is the class without any past-year ND, and a lower prevalence of prior-to-past-year ND than the other classes. Classes 2 and 3 had high SEPs for the criteria ‘withdrawal’ and ‘desire or unsuccessful efforts to cut down’. Class 2, the moderate-behavioral subtype, was distinguished from class 3 by moderate SEPs on a wider range of criteria that are behavioral, e.g. ‘increased use’. Although similar to the moderate-behavioral subtype (class 2), class 3, the physiological dependence subtype, was characterized by a high SEPs for a criterion that emphasizes physiological dependence, ‘withdrawal’, and high SEPs on only two behavioral criteria. Class 4, the high dependence subtype, had the highest SEPs for the greatest number of criteria, with probabilities over 0.80 for ‘withdrawal’, ‘increased use’, ‘desire or unsuccessful efforts to cut down’, and ‘continued use despite health problems.’ The high SEPs characterize this class as containing the highest proportion of respondents with prior-to-past-year and past-year ND.
Table 2.
LCA model assessment of ND criteria among ever daily, past-year smokers (n = 8,842).
| Model: Number of Classes | −2 log likelihood | BICa | Δ in BIC |
|---|---|---|---|
| 1 | 66,707.170 | 66,788.955 | |
| 2 | 59,929.708 | 60,102.366 | 6686.589 |
| 3 | 58,967.002 | 59,230.533 | 7558.422 |
| 4 | 58,785.504 | 59,139.908 | 7649.047 |
| 5 | 58,723.192 | 59,168.469 | 7620.486 |
| 6 | 58,675.946 | 59,212.094 | 7576.861 |
| 7 | 58,660.058 | 59,287.080 | 7501.875 |
| 8 | 58,646.616 | 59,364.511 | 7424.444 |
Note: Selected model in bold.
Bayesian Information Criterion.
Fig. 1.
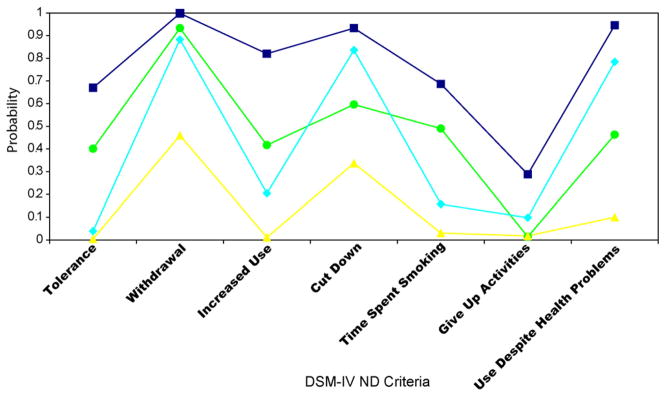
–■– Class 4, High Dependence, 14.93%; –●– Class 2, Moderate-behavioral, 7.41%; –▲– Class 1, Low Dependence, 37.69%; –◆– Class 3, Physiological Dependence, 39.97%.
3.3. Validation of classes
Table 3 presents prevalence rates of disorders and means for each of the identified classes. The latent classes significantly differed on all of the variables employed as validators, lending strength to the selection of the presented class solution. Chi-square analyses of the associations between the latent classes and ND for the total sample revealed significant associations (p < 0.0001). As expected, the low dependence subtype (class 1) had no respondents with past-year ND, but a conditional probability of 10.29% for prior-to-past-year ND. The high dependence subtype (class 4), with the highest SEPs across criteria, had a high prevalence of lifetime ND. Consistent with the categorical validators, respondents belonging to the high dependence class 4 had the most extreme values for the continuous smoking characteristic validators. Compared to the other classes, these respondents had the greatest mean number of ND criteria, started smoking daily at a younger age, smoked a larger quantity of cigarettes as daily smokers, and had the youngest age of onset of ND. Respondents in the behavioral-moderate (class 2) and physiological dependence (class 3) classes had a higher prevalence of lifetime ND as compared to the low dependence subtype (class 1), but were very similar to each other with respect to mean number of ND criteria. The physiological dependence respondents displayed a higher prevalence than the behavioral-moderate subtype for past-year and prior-to-past-year ND and higher mean values for the other continuous validators.
Table 3.
LCA validators by assigned class membership of ever-daily, past-year smokers (n = 8842).
| Class 1 Low dependence’ (n = 3,477) % or Mean (S.E.) |
Class 2 ‘Moderate-behavioral’ (n = 632) % or Mean (S.E.) |
Class 3 ‘Physiological dependence’ (n = 3,453) % or Mean (S.E.) |
Class 4 High dependence’ (n = 1,280) % or Mean (S.E.) |
p-value | |
|---|---|---|---|---|---|
| Prevalence of Past-Year ND | 0.00 (0.00) | 71.50 (2.15) | 81.57 (0.76) | 100.00 (0.00) | <0.0001 |
| Prevalence of Prior to Past-Year ND | 10.29 (0.68) | 70.72 (2.18) | 79.34 (0.82) | 95.86 (0.62) | <0.0001 |
| Prevalence of Past-Year MD | 6.21 (0.49) | 21.43 (2.17) | 12.83 (0.72) | 29.46 (1.39) | <0.0001 |
| Prevalence of Prior to Past-Year MD | 13.80 (0.69) | 30.29 (2.30) | 24.72 (0.93) | 43.01 (1.81) | |
| Mean Age Started Smoking Daily (in years) | 20.32 (0.23) | 18.51 (0.52) | 18.89 (0.17) | 17.50 (0.22) | <0.0001 |
| Mean Quantity Smoked When Smoked Daily (in # of cigarettes) | 15.18 (0.24) | 19.19 (0.60) | 17.52 (0.20) | 20.98 0.40) | <0.0001 |
| Mean Age of Onset of ND (in years) | 34.55 (1.79) | 32.38 (1.03) | 36.58 (0.41) | 31.88 (0.66) | <0.0001 |
The high dependence subtype had the highest prevalence of past-year and prior-to-past-year MD among the classes. The prevalence rate ratio (PRR) for prior-to-past-year MD was 2.99 for high dependence class 4 compared to low dependence class 1; this high PRR was also found for past-year MD (PRR = 4.92). A differential pattern was observed for the behavioral-moderate and physiological dependence subtypes (classes 2 and 3), with a higher prevalence of past-year and prior-to past-year MD in the behavioral-moderate class than in the physiological dependence class.
3.4. Multivariable models for major depression outcomes
Table 4 presents the results of logistic regression models that predict past-year MD and lifetime MD criteria by class membership. The odds ratios presented in the table represent the odds of meeting criteria for past-year MD or endorsement of a DSM-IV MD symptom among those in classes 2, 3, and 4, as compared to respondents belonging to class 1 (no past-year ND). These models were adjusted for the sociodemographic characteristics sex, age, race/ethnicity, and education, as outlined above in Section 2.
Table 4.
Odds ratios for major depression (MD) and depressive criteria (n = 8,842).
| Moderate-behavioral vs. Low dependencea (n = 632) OR (95% CI) |
Physiological vs. Low dependenceb (n = 3,453) OR (95% CI) |
High vs. Low dependencec (n = 1,280) OR (95% CI) |
p-value | |
|---|---|---|---|---|
| Past-Year MD | 3.66 (2.62–5.11) | 2.15 (1.73–2.69) | 5.81 (4.64–7.27) | <0.0001 |
| MD criteria | ||||
| Depressed mood | 2.17 (1.72–2.75) | 1.71 (1.51–1.93) | 3.77 (3.22–4.43) | <0.0001 |
| Diminished pleasure or interest | 2.85 (2.24–3.63) | 1.85 (1.64–2.09) | 4.65 (3.91–5.52) | <0.0001 |
| Significant weight change | 2.41 (1.89–3.07) | 1.88 (1.64–2.15) | 4.72 (3.86–5.77) | <0.0001 |
| Insomnia or hypersomnia | 2.55 (2.02–3.21) | 1.98 (1.75–2.23) | 4.94 (4.18–5.84) | <0.0001 |
| Psychomotor agitation or retardation | 2.78 (2.14–3.63) | 2.09 (1.80–2.42) | 5.47 (4.50–6.65) | <0.0001 |
| Fatigue or loss of energy | 2.61 (2.06–3.32) | 2.07 (1.82–2.35) | 5.34 (4.49–6.36) | <0.0001 |
| Feelings of worthlessness or guilt | 2.82 (2.18–3.64) | 1.98 (1.73–2.26) | 5.04 (4.26–5.98) | <0.0001 |
| Diminished ability to think or concentrate | 2.82 (2.24–3.56) | 1.97 (1.74–2.23) | 5.11 (4.29–6.08) | <0.0001 |
| Recurrent thoughts of death or suicidal ideation | 2.60 (1.92–3.52) | 2.03 (1.68–2.45) | 4.59 (3.75–5.60) | <0.0001 |
Note: MD symptoms are lifetime, while diagnosis is past-year. Models are adjusted for sex, age, education, and race/ethnicity.
Class 2 vs. Class 1.
Class 3 vs. Class 1.
Class 4 vs. Class 1.
As compared to the low dependence subtype (class 1), respondents in classes 2, 3, and 4 each had significantly higher (p < 0.0001) odds of past-year MD and each lifetime MD symptom. We found a marked and consistent pattern of association between subtypes of smokers in our sample and MD characteristics, with increasing odds ratios across classes that were significantly different, i.e. for all individual MD criteria the highest risk was found for class 4, followed by class 2, 3 and then class 1. The high dependence subtype (class 4) had the highest ratio of odds ranging from 3.77 to 5.47, followed by the behavioral-moderate subtype (class 2) with OR’s ranging from 2.17 to 2.85, and the physiological dependence subtype (class 3) with OR’s ranging from 1.71 to 2.09. The magnitude of difference in odds of past-year depression and lifetime criteria was similar between the high dependence and behavioral-moderate subtypes (classes 4 and 2), and the behavioral-moderate and physiological dependence subtypes (classes 2 and 3). For example, for the odds of past-year MD, respondents in the high dependence subtype (class 4) had over one and a half-fold higher odds than those in the behavioral-moderate subtype (class 2), and behavioral-moderate respondents also had over one and a half times higher odds of MD than those in the physiological dependence class (class 3). We directly tested the odds of MD for the behavioral-moderate and physiological classes to see if they differed via a post hoc contrast. The contrast for the odds of MD for behavioral-moderate respondents (OR = 3.66, 95% CI = 2.62–5.11) class as compared to the odds for respondents in the physiological class (OR = 2.15, 95% CI) was significant (F = 12.25, 1 df, p = 0.0008).
4. Discussion
Several key findings were generated from our analyses of 8, 842 daily smokers drawn from the NESARC sample. We found (1) evidence of empirically derived and meaningful subtypes of smokers in our latent class analyses; the results of our analyses identified four distinct classes; (2) these classes were characterized quantitatively, by increasing levels of severity, and qualitatively, with two unique dependence symptom configurations for respondents with mild or moderate ND; (3) there were significant differences between the classes in the prevalence of MD, ND, and smoking characteristics; and (4) as compared to the low dependence subtype (class 1 respondents) without current ND, the other classes had increasingly higher odds of past-year MD and odds of specific MD criteria that were consistent across symptoms, and (5) respondents with mild to moderate ND qualitatively differed in their ND symptom configurations and odds of MD.
We found evidence for quantitative and qualitative differences between the classes identified from the selected model. Fig. 1 suggests that the four classes form three groups quantitatively characterized by severity, with the lowest SEPs across the seven ND criteria among low dependence (class 1) respondents and the highest SEPs among high dependence (class 4) respondents. Behavioral-moderate and physiological dependence (classes 2 and 3) respondents hovered in the middle between classes 1 and 4 across ND criteria. This is consistent with previous latent class analysis research by Xian et al. (2007) of DSM-III-R ND criteria in a sample of middle-aged male veterans, which also identified 4 latent classes quantitatively characterized on a severity spectrum. Although there were changes in criteria between DSM-III-R and DSM-IV and our study drew from a different sample, we found a similar latent class structure as Xian et al. (2007). Both studies suggest that both the number and types of ND criteria must be taken into account when assessing severity of ND using DSM criteria. We also found only a small proportion (12.27%) of respondents of the high ND subtype (which had the highest SEPs across symptoms) were severely dependent (using endorsement of all seven ND criteria as an operational definition), although 100% of these individuals met criteria for past-year ND.
With respect to explanations for symptom level associations between ND and MD, the analyses suggest that severity is a strong component, but that among those with mild to moderate ND, behavioral criteria of ND may play a more prominent role in the likelihood of MD. As mentioned above, the behavioral-moderate and physiological subtypes (classes 2 and 3) were quite similar with respect to quantitative severity, but different SEP profiles exist for each. The behavioral-moderate subtype, with higher odds of depression than the physiological subtype, was characterized by moderate SEPs (greater than .40 for all but one symptom) across the seven ND criteria. Comparatively, SEPs for the physiological subtype, which was more affected by ND, were more concentrated. This class had a high SEP for the ‘withdrawal’ criteria, and two behavioral SEPs, ‘use despite health problems’ and ‘inability to cut down or quit’; this concentration could be viewed as indicative of greater physiological dependence. Behavioral-moderate respondents represent a unique subtype of mild to moderately dependent smoker that are at higher risk of depression, with a greater number of ND symptoms that are behavioral in nature. The AUDADIS-IV does not have a neuroticism subscale, but it may be that this subgroup of smokers would score higher on this trait, as research has shown linkages between smoking and neuroticism (Munafó and Black, 2007; Munafó et al., 2007).
The two main approaches used to define nicotine dependence are the Fagerström Test for Nicotine Dependence (FTND) (Heatherton et al., 1991) and the Diagnostic and Statistical Manual of Mental Disorders (DSM) (APA, 1994). As we described in Section 1, there are indications that these two approaches diagnose different smokers (Breslau and Johnson, 2000; Moolchan et al., 2002), have differential associations with major depression (Breslau and Johnson, 2000), and emphasize different aspects of nicotine dependence. Given that the FTND is intended to assess physical dependence and based on Breslau’s findings (2000) of no significant association between FTND and depression, it is reasonable to speculate that similar findings in our sample would be generated by any type of latent class analysis using the FTND. The intention of this paper is not to settle the validity of these contending definitions of nicotine dependence, but rather to identify subtypes of smokers with greater likelihoods of major depression comorbidity. Our results, when considered along with other research, indicate that DSM assessment of nicotine dependence may more useful for identifying those most likely to be depressed.
We explored whether the latent classes were meaningful and added information about these respondents beyond grouping by ND severity. When severity of ND, operationalized as number of DSM ND criteria, was included in the multivariable logistic regression model, respondents assigned to the behavioral-moderate class still had higher odds of MD than the low dependence referent group. The odds ratios for the behavioral-moderate and the physiological dependence classes were not significantly different, but this may be a power issue rather than being indicative of true similarity. So while respondents in these mild to moderate ND groups had almost identical mean number of ND criteria, even after controlling for the number of ND criteria we still found a higher likelihood of MD for the behavioral-moderate subtype than for the physiological dependence subtype. This qualitative difference between these two classes cannot be completely accounted for by severity of ND measured simply by the number of criteria endorsed. This suggests that the symptom profile for the behavioral-moderate class represents a unique and important configuration of dependence symptoms that is associated with MD.
The following data limitations should be kept in mind when interpreting the results generated from the present study. First, the NESARC data are cross-sectional and comprised of self-reported retrospective information from respondents, thus precluding a precise examination of temporal effects. We did, however, utilize past-year ND symptoms and focused on past-year MD diagnoses rather than lifetime diagnoses. These are likely to be more accurate for study as the period of recall for respondents is briefer and less prone to recall error. Second, our adjusted analyses of individual major depression criteria were based on lifetime symptoms rather than symptoms experienced in the past 12 months, as we did not have data linking symptoms to specific episodes of depression for respondents with multiple episodes. Given our limited understanding of the nature of the factors connecting ND and MD in the general population, the identification of subtypes of smokers and their respective risks of MD are important and clinically relevant epidemiological findings. These temporal difficulties will be reduced in the future, as the NESARC has been designed as a longitudinal study and analysis of the second wave of data will allow for examination of temporal effects and exploration of causal models.
The NESARC is a rich data set with which to examine specific aspects of the ND and MD comorbidity, for several reasons. First, unlike many studies of these disorders that have used unstandardized assessments of ‘smoking’, did not assess dependence, or used criteria from previous DSM editions, the items included in the survey allowed for the mirroring of DSM-IV criteria and construction of disorders. Likewise, most community studies of this important comorbidity have utilized symptom scales for depression that preclude the assessment of DSM-IV defined MD. Second, the large sample size is quite important to this study because the prevalence of current (past 12-month) comorbidity (as opposed to lifetime comorbidity, i.e., having each disorder at some time during the lifespan) is relatively low in the general population. We were also able to extend previous LCA research of ND symptoms by using data that is nationally representative, which allows for broad generalizability of the results reported in this study.
Employing LCA allowed us to view the classification of respondents from both quantitative and qualitative perspectives. Through these analyses, we were able to empirically identify homogeneous groups of smokers, mainly characterized by ND severity, rather than subjectively classifying respondents with predetermined cut-points. Our analyses have identified subtypes of smokers that experience higher prevalence rates of depression than that found in the general population. We found a meaningful proportion of respondents (14.93% of study population) who were characterized by ND severity also had the highest prevalence of depression. This is consistent with previous co-occurring disorders research demonstrating increased risk of additional psychopathology with increased severity of the primary disorder. We also detected qualitative differences in symptom configuration between respondents with mild or moderate dependence that were associated with differences in the likelihood of MD, identifying a behavioral-moderate subgroup of smokers with less severe nicotine dependence who also had a significantly elevated risk of MD (OR = 3.66; CI, 2.62–5.11). While the respondents in this class were quite similar to quantitative ND severity of other classes, they endorsed wider range of ND criteria, many of which emphasize the psychological or behavioral aspects of ND.
The results of these analyses suggest that some behavioral ND criteria, such as time spent smoking and unintended increased use, and the tolerance criterion, may be more centrally related to MD. The moderate SEPs associated with a wide range of symptoms in this moderate-behavioral class indicates that there is a great deal of heterogeneity in symptom profiles among these smokers, while respondents in the physiological class (with a lower odds of MD) are likely to have more homogeneous profiles emphasizing physiological dependence. Future research is needed on the importance of specific ND criteria in predicting MD. The present study is an intermediate step in illuminating the threads that connect these two disorders. Investigating the linkages between them is of the utmost public health importance, given their high prevalence and co-occurrence in the population and the impact smoking and depression have on disability, morbidity, and mortality.
Acknowledgments
Role of funding source
Funding for this study was provided to Melinda Manley by National Institute of Mental Health Training Grant (T32-MH14235). The NIMH had no further role in the study, writing of the report, or in the decision to submit the manuscript for publication. The National Epidemiologic Survey of Alcohol and Related Conditions (NESARC), from which the data used for the present study were drawn, was designed and conducted by the NIAAA, a part of the NIH.
Footnotes
Contributors
All authors participated in the design of the study and analyses. Melinda Manley and Dr. de Jonge undertook the analyses. Melinda Manley wrote the first draft of the manuscript and all authors participated in revisions. All authors contributed to the manuscript and have approved this final version.
Conflicts of interest
All authors declare that they have no conflicts of interest.
References
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Breslau N, Johnson EO. Predicting smoking cessation and major depression in nicotine-dependent smokers. American Journal of Public Health. 2000;90:1122–1127. doi: 10.2105/ajph.90.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003a;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003b. [Google Scholar]
- Hagenaars JA, McCutcheon AL, editors. Applied Latent Class Analysis. Cambridge University Press; New York: 2002. [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jorm AF. Association between smoking and mental disorders: results from an Australian national prevalence survey. Australian and New Zealand Journal of Public Health. 1999;23:245–248. doi: 10.1111/j.1467-842x.1999.tb01250.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Wai Tat C, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden PAF, Bucholz KK, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Martin NG, Heath AC. Nicotine withdrawal in women. Addiction. 1997;92:889–902. [PubMed] [Google Scholar]
- McCutcheon AL. Latent Class Analysis. Sage; Newbury Park, CA: 1987. [Google Scholar]
- Moolchan ET, Radzius A, Epstein DH, Uhl G, Gorelick DA, Cadet JL, Henning-field JE. The Fagerström Test for Nicotine Dependence and the Diagnostic Interview Schedule: do they diagnose the same smokers? Addictive Behaviors. 2002;27:101–113. doi: 10.1016/s0306-4603(00)00171-4. [DOI] [PubMed] [Google Scholar]
- Munafó MR, Black S. Personality and smoking status: a longitudinal analysis. Nicotine & Tobacco Research. 2007;9:397–404. doi: 10.1080/14622200701188869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafó MR, Zetteler JI, Clark TG. Personality and smoking status: a meta-analysis. Nicotine & Tobacco Research. 2007;9:405–413. doi: 10.1080/14622200701188851. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Muthén & Muthén; Los Angeles, CA: 1998–2004. [Google Scholar]
- RTI. SUDAAN Language Manual, Release 9.0. Research Triangle Institute; Research Triangle Park, NC: 2004. [Google Scholar]
- Storr CL, Hongling Z, Kung-Yee L, Anthony JC. Empirically derived latent classes of tobacco dependence syndromes observed in recent-onset tobacco smokers: epidemiological evidence from a national probability sample survey. Nicotine & Tobacco Research. 2004a;6:533–545. doi: 10.1080/14622200410001696493. [DOI] [PubMed] [Google Scholar]
- Storr CL, Reboussin BA, Anthony JC. Early childhood misbehavior and the estimated risk of becoming tobacco-dependent. American Journal of Epidemiology. 2004b;160:126–130. doi: 10.1093/aje/kwh184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xian H, Scherrer JF, Eisen SA, Lyons MJ, Tsuang M, True WR, Bucholz KK. Nicotine dependence subtypes: association with smoking history, diagnostic criteria and psychiatric disorders in 5440 regular smokers from the Vietnam Era Twin Registry. Addictive Behaviors. 2007;32:137–147. doi: 10.1016/j.addbeh.2006.03.031. [DOI] [PubMed] [Google Scholar]
- Xian H, Scherrer JF, Madden PAF, Lyons MJ, Tsuang M, True WR, Eisen SA. Latent class typology of nicotine withdrawal: genetic contributions and association with failed smoking cessation and psychiatric disorders. Psychological Medicine. 2005;35:409–419. doi: 10.1017/s0033291704003289. [DOI] [PubMed] [Google Scholar]


