Dear Editor,
We present here a case report of a benign seminal vesicle cystadenoma treated with laparoscopic ablation in a 31-year-old man. The clinical presentation, gross appearance, microscopic characteristics, immunohistochemical and ultrastructural findings of this uncommon tumour are discussed.
Primary seminal vesicle tumours are rare and may be benign or malignant. Benign primary seminal vesicle tumours include cystadenomas, hydatid cysts, papillary adenomas and amyloid depositions. Malignant primary seminal vesicle tumours include cystosarcoma phyllodes, adenocarcinoma, sarcoma, carcinoid and primary seminoma.1 In some cases, cystadenoma of the seminal vesicle was an incidental finding of an asymptomatic mass.2,3 The majority of patients present with symptoms of urinary outflow obstruction, haematuria or haematospermia.4,5,6 The wide variety of presenting features might result from variations in the size and location of the retrovesical mass. In our case, the presenting symptom was haematospermia, and the retrovesical mass was detected with abdominal pelvic CT.
All tumours of the seminal vesicle are resected using open surgery or laparoscopic ablation.2,3 Open surgery includes transperineal, transvesical, paravesical, retrovesical and transcoccygeal approaches. In one case, radical cystoprostatectomy, low anterior resection of the rectum and orthotopic neobladder reconstruction were performed.1,3 The surgical removal of seminal vesicle tumours via open surgery has become much more difficult. A transvesical approach is believed to be the best surgical approach because it enables full exposure and complete excision of the tumour with minimal risk of damage to the rectum and the bladder nerves.7 The laparoscopic approach to the management of seminal vesicle cysts has been described. Laparoscopic excision of seminal vesicle disease is an effective surgical procedure associated with minimal postoperative morbidity, short hospitalisation times and rapid recovery for the patient.8
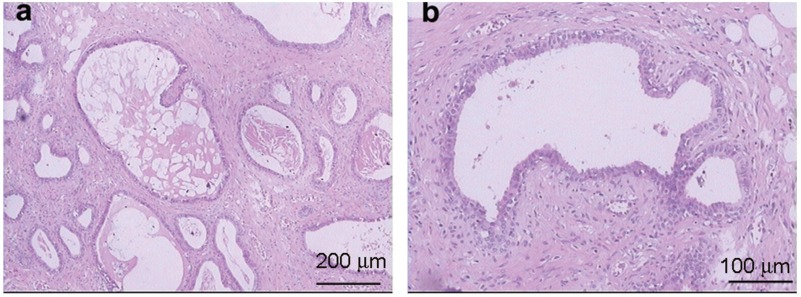
Macroscopically, the cystadenoma of the seminal vesicle consists of a multilobulated mass containing bloody fluid.1 A prominent feature of cystadenomas of the seminal vesicle in microscopic examination is that the cystic area is lined with a single layer of columnar or cuboidal epithelium surrounded by a fibrous stroma.9 Histologically, multiple glands and cysts of varying sizes and shapes are filled with homogeneous eosinophilic material, with no malignant features. The stromal component is abundant. All findings are consistent with cystic epithelial stromal tumour.1 Immunohistochemical staining is helpful for diagnosing cystadenoma of the seminal vesicle. The epithelium is positive for cytokeratin and negative for calretinin and prostate-specific antigen. The stromal cells show no reactivity for the S-100 protein, but irregular weak positive reactions for smooth muscle actin.3
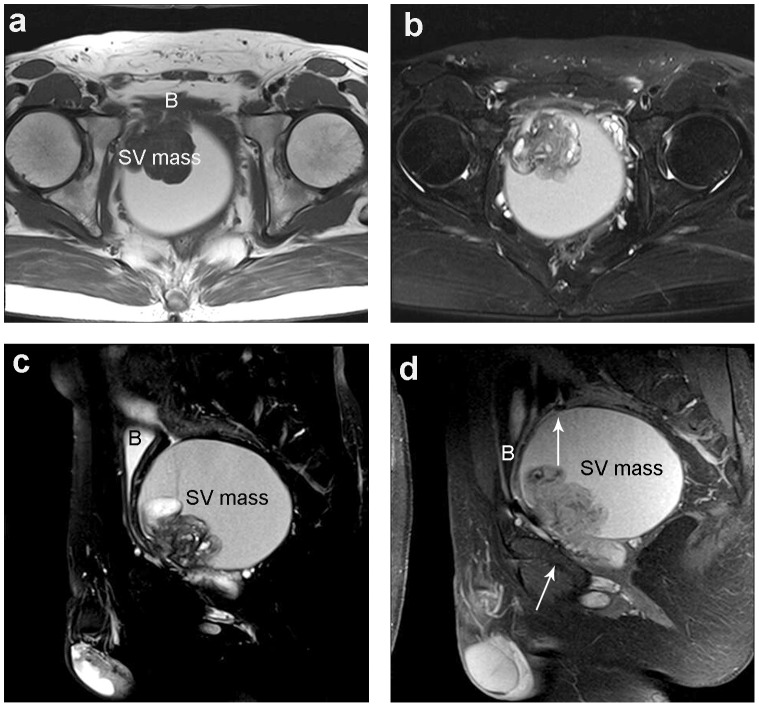
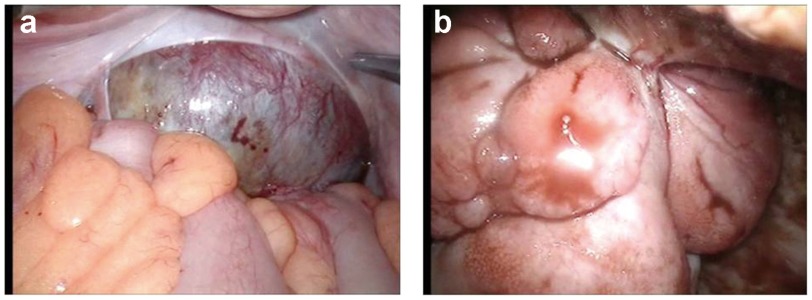
We report a 31-year-old man who presented with recurrent haematospermia. An MRI of the pelvis revealed a mass that consisted of both cystic (maximal diameter of 8.8 cm) and solid elements (4.4 cm) (Figure 1). The solid and cystic mass in the left seminal vesicle was resected using laparoscopic excision. The patient was counselled for the laparoscopic excision of a solid and cystic mass of the left seminal vesicle. He was placed in the Trendlenberg position, and a camera port was inserted through a small periumblical incision using the Hassan technique. One 10-mm port and three 5-mm ports were inserted under direct vision. The relevant landmarks, including the external iliac vessels, the internal ring of inguinal canal and the vas deferens, were inspected. Initial inspection revealed a cystic mass projecting from behind the bladder into the abdominal cavity (Figure 2a).
Figure 1.
MRI of the pelvis. (a) An axial pre-contrast spin echo T1-weighted image (T1WI) shows a solid and cystic occupying lesion behind the bladder. The solid portion presents an isointensity lobulated mass (arrow) relative to the muscles, and the cystic portion presents a homogeneous hyperintensity. (b) A T2-weighted image (T2WI) axial view pre-contrast with fat suppression shows the solid portion presenting an inhomogeneous hyperintensity (arrow) relative to the muscles and the cystic part demonstrating a homogeneous hyperintensity. (c) A sagittal plane T2WI with fat suppression shows the solid portion of the tumour presenting a 5 cm×6 cm lobulated mass arising from the seminal vesicle (arrow). (d) A sagittal plane T1WI post-contrast view with fat suppression shows the solid portion of the tumour presenting with a mild-to-medium delayed inhomogeneous enhancement. The solid portion is connected to the seminal vesicle via a pedunculation (arrow). B, bladder; SV, seminal vesicle; T1WI, T1-weighted image; T2WI, T2-weighted image.
Figure 2.
Laparoscopic view a cystic mass. (a) A laparoscopic view of a cystic mass projecting from behind the bladder into the abdominal cavity. (b) A laparoscopic view of a 5 cm×2 cm tumour detected in the front internal wall of the mass and connecting to the left seminal vesicle.
The peritoneum overlying the mass was incised sharply. Further dissection around the mass was difficult and was abandoned because of serious adhesion. The mass was then incised, and a total of 600 ml of chocolate brown fluid was aspirated. A 5 cm×2 cm tumour was detected in the front internal wall of the mass connected to the left seminal vesicle (Figure 2b). The left seminal vesicle was dissected and divided, and the cystic wall was removed to the greatest possible extent. The excised specimens were placed in an entrapment sac and extracted through the right incision, along with the 10-mm trocar. A final inspection was performed to assure excellent haemostasis. The operative time was 125 min, and the blood loss was 120 ml. The patient's recovery was uncomplicated. Postoperative examinations 10 months after surgery showed that the haematospermia has disappeared.
The histological features were consistent with seminal vesicle cystadenoma (Figure 3). Cystic tumours of the seminal vesicle should be removed as soon as possible because they may be malignant.1 The laparoscopic excision of prostate and bladder tumours is steadily becoming the standard procedure. Laparoscopic excision of seminal tumours is advisable because of its obvious benefits of less invasiveness and easy recovery.
Figure 3.
Histological view of this cystadenoma of the seminal vesicle (HE staining). (a) Multiple glands and cysts of varying sizes and shapes are filled with homogeneous eosinophilic material, with no malignant features. Scale bar=200 µm. (b) The prominent intervening stroma contain abundant smooth muscle and fibres. Scale bar=100 µm.
Author contributions
JGZ participated in drafting the manuscript; WHC, SXX and RPW helped to collect the clinical data and participated in the paper's discussion. ZLS supervised the study design and coordination. All of the authors have read and approved the final manuscript.
The authors declare no competing financial interests.
References
- Lorber G, Pizov G, Gofrit ON, Pode D. Seminal vesicle cystadenoma: a rare clinical perspective. Eur Urol. 2011;60:388–91. doi: 10.1016/j.eururo.2009.07.022. [DOI] [PubMed] [Google Scholar]
- Gil AO, Yamakami LY, Genzini T. Cystadenoma of the seminal vesicle. Int Braz J Urol. 2003;29:434–6. doi: 10.1590/s1677-55382003000500009. [DOI] [PubMed] [Google Scholar]
- Lee CB, Choi HJ, Cho DH, Ha US. Cystadenoma of the seminal vesicle. Int J Urol. 2006;13:1138–40. doi: 10.1111/j.1442-2042.2006.01511.x. [DOI] [PubMed] [Google Scholar]
- Lagalla R, Zappasodi F, Lo Casto A, Zenico T. Cystadenoma of he seminal vesicle: US and CT findings. Abdom Imaging. 1993;18:298–300. doi: 10.1007/BF00198130. [DOI] [PubMed] [Google Scholar]
- Dalgaard JB, Giertsen JC. Primary carcinoma of the seminal vesicle: case and survey. Acta Pathol Microbiol Scand. 1956;39:255–67. doi: 10.1111/j.1699-0463.1956.tb03400.x. [DOI] [PubMed] [Google Scholar]
- Mazur MT, Myers JL, Maddox WA. Cystic epithelial-stromal tumor of the seminal vesicle. Am J Surg Pathol. 1987;11:210–7. doi: 10.1097/00000478-198703000-00006. [DOI] [PubMed] [Google Scholar]
- Wein AJ, Kavoussi LR, Novic AC, Partin AW, Peters CA, et al. Campbell-Walsh Urology. 9th ed. Philadelphia, PA; Saunders Elsevier; 2007.; pp. 1116–25. [Google Scholar]
- McDougall EM, Afane JS, Dunn MD, Shalhav AL, Clayman RV. Laparoscopic management of retrovesical cystic disease: Washington University experience and review of the literature. J Endourol. 2001;15:815–9. doi: 10.1089/089277901753205816. [DOI] [PubMed] [Google Scholar]
- Mazzucchelli L, Studer UE, Zimmermann A. Cystadenoma of the seminal vesicle: case report and literature review. J Urol. 1992;147:1621–4. doi: 10.1016/s0022-5347(17)37649-8. [DOI] [PubMed] [Google Scholar]