Abstract
Background and aims: Oral mucositis (OM) is still a common and severe acute side-effect of many oncologic treatments, especially in patients treated for head and neck cancer. It may affect quality of life, require supportive care and impact treatment planning and its efficacy. Low-level laser therapy (LLLT) seems to promote pain relief and reduces OM incidence and its severity. It has been recommended for these patients as a treatment option but without any consensus in the LLLT procedure. New recommendations and perspectives for clinical trials will be discussed.
Materials (Subjects) and Methods: Step by step, the efficacy of soft laser in the management of iatrogenic oral mucositis has been evaluated during the last two decades. Its effectiveness and level of recommendation got stronger with time. We will report and discuss some major results and the latest recommendations published on this topic.
Results: The major clinical results have been reported and analysed last year in a first meta-analysis 1). 11 randomized placebo-controlled trials were selected with a total of 415 patients treated with chemotherapy and/or radiotherapy for head and neck cancer. The relative risk for developing OM was significantly reduced after LLLT but only for a dose between 1 to 6 Joules per point. Pain, severity and duration of OM grade ≥ 2 were also reduced without difference with placebo for possible side-effects. Nine years after the positive results published for patients treated by radiotherapy alone 2), a new French randomized, multicentric, phase III trial for patients treated with new standard treatment, using LLLT in accordance to recent recommendations is ongoing. Seven centers are specifically established for this trial which should include a hundred patients.
Conclusions: The very encouraging results of LLLT in the prevention and treatment of OM in patients treated by chemotherapy or radiotherapy for advanced head and neck cancer could soon be proposed as a new standard of care, according to the multinational Association of Supportive care in Cancer (MASCC) criteria. Modern lasers are less time consuming and extraoral applicators for a possible use by trained paramedical staff could be helpful to complete clinician practice. A preventive dose of 2 J/cm2 and a curative dose of 4 J/cm2 if using a red wavelength lasers are now recommended.
Keywords: low-level laser therapy, oral mucositis, radiation therapy, chemotherapy
Introduction
Oral mucositis (OM) is a frequent acute side effect of antineoplastic treatment in patients treated by radiotherapy and/or chemotherapy especially for head and neck cancer (Fig.1). Its prevalence has increased over the last 5 years due to more aggressive treatment protocols and combined modality regimens, reaching 36% to 100% of patients 3). This painful side effect reduces quality of life and often requires narcotic analgesia, enteral or parenteral nutrition with additional costs 4).
Fig. 1:

Oral mucositis grade 3 :
Modifications of treatment planning may be necessary, leading to 19% of interruptions and possibly affect local control and finally survival 5). Treatment of OM is still essentially palliative and there is no consensus on any agent for prophylactic or therapeutic use, even for oral care with mouth rinse and cryotherapy. Several topical and systemic treatments have been tested to decrease frequency and severity of OM, but only few of them such as oral cryotherapy and palifermin 6), have shown a significant preventive effect. Some 12 different interventions have yielded partly positive results in controlled trials with varying degree of scientific support, but none of them has emerged as a gold standard 7).
Low-Level laser therapy (LLLT) is a non invasive simple and atraumatic therapeutic management corresponding to a local application of a high density monochromatic narrow-band light source (Fig. 2). The output power range from 5 to 200 mW with helium/neon (632.8 nm) or diode laser with various wavelengths (630-680, 700-830 and 900 nm). With adequate energy and fluence, three main effects have been clinically observed and reported: an analgesic effect 8), an anti-inflammatory effect and a wound healing property 9). Various biological effects explaining the last property has been described: an activation of energy production in mitochondria, an increased collagen production, a fibroblast cell proliferation, a detoxification of free radicals produced by the oncologic treatments, an inhibition of NK-Kappa B and also an angiogenesis 10). These mechanisms do not seem to be wavelength specific in the red and infrared spectrum but dose-dependent. No known toxicity has been reported by in vivo studies.
Fig. 2:

Intraoral treatment with LLLT
Laser therapy has been investigated in various areas of medicine and dentistry. Trials using soft laser to prevent and control OM are difficult to compare because many wavelengths and tools to assess mucositis were tested, and there was no protocol standardization. Nevertheless, the Multinational Association of Supportive Care in Cancer (MASCC) recommend the use of soft laser to prevent OM with a level IIB in patients undergoing high dose chemotherapy with hematopoietic stem cell transplant (HSCT). Until last year, scientific evidence of laser therapy in the management of OM in patients treated with other chemotherapy and / or radiotherapy was still limited to a level III 11).
Materials and Methods
Step by step, the efficacy of soft laser in the management of iatrogenic oral mucositis has been reported in the past literature, spanning over many years of research, a higher level of evidence and some recommendations. We will comment on the major results published during the last three decades. We will finally present the ongoing first French multicentric phase III prospective double-blind randomized trial in the prevention and treatment of oral mucositis in head and neck cancer patients treated with concurrent chemoradiation.
Results
The efficiency of Laser on reducing OM has been reported thirty years ago in France, in a retrospective study conducted by Ciais 12). Patients were treated with chemotherapy including Fluorouracil. Frequency and severity of OM were significantly reduced by laser therapy and incidence of oral complications decreased from 43% to 6%. With laser therapy, the compliance for cancer treatment was improved and all the patients received their chemotherapy as originally scheduled. In 1999, Bensadoun et al published the first randomized double blind trial for patients treated by radiotherapy for head and neck cancer. 30 patients were included, treated by radiotherapy alone and randomized between a 60 mW He-Ne 632.8 nm laser and a placebo light treatment. Again, there was a significant reduction of both grade 3 mucositis (7.6% versus 35.2%) and pain (1.9% versus 23.8%), with a reduction of pain relief in patients treated with active laser therapy 2). The efficacy of LLLT has been later evaluated in various randomized trials over the world, for patients treated by radiotherapy alone 14-16) or by concurrent chemoradiation 17-20).
During the last 2 decades, the benefit on incidence, time and duration of OM has been confirmed in most of randomized controlled studies published especially for patients submitted to a high dose chemotherapy prior to hematopoietic stem cell or bone marrow transplantation 21-23). In 2004, the expert panels of the Multinational Association of Supportive Care in Cancer (MASCC) and the International Society for Oral Oncology (ISOO) considered LLLT, after reviewing literature published from 1966 to May 2002, as a possible option in the management of OM for these patients, with a level II of evidence and a grade B of recommendation 5). Two years later, after selecting and reviewing results from 2 new clinical studies, soft laser was still a promising but not conclusive tool because of heterogeneity in laser parameters (wavelength, power, doses) and tools used to assess mucositis 6). In 2007, it became in updated data a “recommended” method for the prevention of OM during bone marrow transplantation or hematopoietic stem cell transplant 11). By contrast, there was no specific chapter for OM in the World Association for Laser Therapy (WALT) guidelines with a lack of consensus for the use of LLLT and its useful technical parameters. In 2010, a UK analysis using electronic searches from 1950 and selecting randomized controlled trials for patients receiving chemotherapy or radiotherapy or both, also showed a significant reduction in severe mucositis when compared with a sham procedure with a RR of 5.28. Nevertheless, the authors concluded with a non-enthusiastic, weak and unreliable evidence of low level laser efficacy on mucositis and suggested that further well designed, placebo-controlled trials were needed to improve this level of evidence 24).
A next step to achieve this goal has been made last year with the publication a systematic review of literature. It was the first meta-analysis on this topic 1). The objectives were to analyse the prophylactic and therapeutic effect of LLLT on OM, and to identify the effect of different technical parameters like power, dose, wavelength, time of treatment, and finally to point out some devices and a possible procedure. 11 randomized placebo-control trials published between 1997 and 2009 for a total of 415 patients were selected according to the exclusion / inclusion procedure chosen. Methodological quality was high with a mean score of 4.10 on a 5-point Jadad scale.
When LLLT started before OM ulcers occurred, there was a significant preventive effect of LLLT with a relative risk at 2.03 less (95% confidence interval: 1.11-3.69) for OM occurrence and p = 0.02. One trial using a very low dose of 0.18J/cm2 and short time of treatment was source of significant heterogeneity. But, after sub-grouping trials with doses above or over 1J/cm2, heterogeneity disappeared and Risk Ratio for preventing OM increased to 2.72 with a narrow confidence interval (95% CI: 19.8-3.74). LLLT reduced significantly in five studies the duration of OM grade 2 or worse with 4.38 days less than with placebo (p =0.0004, 95% CI: 3.35-5.40). Mucositis severity was analysed on a Standardized Mean Difference (SMD) because of heterogeneity in index scales used. The combined SMD effect size was 1.33 (95% CI: 0.68-1.98) which correspond to a very good effect (Fig. 3). What was the effect of Wavelengh? A subgroup analysis revealed no heterogeneity between trials for the red (630-670 nm) and the infrared (780-830 nm) subgroups respectively (p>0.21) and there were no significant wavelength differences in relative risks of OM between red at 2.72 and infrared at 3.48. But a further analysis of wavelength-specific doses revealed that a dose of 2J/cm2 or less with infrared light was ineffective in reducing mucositis severity (SMD = 0.38; 95% CI: 0.19-0.96), whereas, a dose of 6J/ cm2 for both red and infrared wavelengths was highly effective, increasing SMD effect at 2.17 (95% CI 1.48-2.86).
Fig. 3:
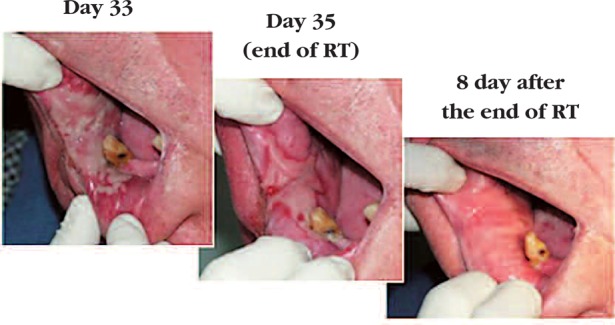
Healed oral mucositis after LLLT treatment
Analysis of pain intensity was performed in 4 trials using different scales. The combined analysis revealed a significant effect in favour of LLLT with an SMD at 1.22(95% CI 0.19-2.25) but also with heterogeneity caused by one trial.
All trials reported possible side effects but none of them found a difference between active laser treatment and placebo. Most of papers also reported that laser was very well tolerated by patients.
In conclusion, this first meta-analysis showed a moderate to strong evidence in favour of laser when applied with optimal dose (1-6 J per point), both in prevention, reduction of severity and duration of OM than on pain.
Discussion
Can we point out a gold standard for laser therapy in Oral mucositis? On the basis of randomized trials results and this meta-analysis, recommendations for LLLT parameters in prophylactic and therapeutic use have been recently proposed by Bensadoun and Nair 25), remaining that not less than 2J/cm2 for prophylactic and 4J/cm2 for therapeutic intents should be used with a red wavelength. In practice, treatment point per point with at least 1cm2 during 20 sec or 40 sec depending on the aim, should be applied. Also, laser therapy should be used daily during RT and other days until ulcer resolution with a minimum of three times a week (table 1).
Table 1: recommendations for low-level laser therapy (intraoral applicators only) in prophylaxis and curative treatment of oral mucositis : from Bensadoun RJ, Nair RG in Curr Opin Oncol, 24(4): 363-70.
Table 1: Recommendations for low-level laser therapy in oral mucositis prophylaxis and therapeutics (intraoral laser applicators only)a
| Parameters to be considered | Description | Recommendation |
| Wavelength | Historically: | Red wavelength 633-685 nm |
| He/Ne:632.8nm | Infrared wavelength 780-830nm | |
| Diodes: 630-950nm | ||
| Output | Depending upon the commercially available product | Diode laser outputs of 10-150mW |
| Dose | Depending upon the type of light source | Total dose per application (all over the treated surface): |
| Not less than 2J/cm2 red wavelengths and 3 J/cm2 for infrared for prophylactic use | ||
| Not less than 4J/cm2 red and infrared wavelengths for therapeutic effect. | ||
| Mode of application | How to apply | Application should be in a stationary manner, per a small area not more than 1 cm2. |
| Application should be made moving from point to point. | ||
| Duration of application | Minimum required irradiation time | An average of 6-20 points may be covered per application, depending on the surface area of the lesions in the oral cavity. |
| Time of treatment per point Is done by the formula: | ||
| t (s) = D (J/cm2) ˗ surface (cm2)/power (W) | ||
| For example, with a 100mW device, t will be 20s per point (1 cm2) for prophylactic effect (D=2J), and 40s per point for therapeutic effect (D=4J). | ||
| Targeting the lesion | Where to apply | Lesions must be identified first by trained clinicians before commencing therapy. |
| Duration of therapy | How often should therapy be followed | Therapy should be repeated daily during RT or every other day depending upon the clinical staging or grading and severity of oral lesions and/or OM (minimum of three times a week). |
| Until lesion(s) resolution. |
OM, oral mucositis; RT, radiotherapy.
aFor extraoral laser treatments, modalities are still under investigation.
These recommendations have been mostly applied in a Brazilian phase III double-blind placebocontrolled trial presented during the ASCO annual meeting in 2011 17). The purpose was to examine the effectiveness of laser therapy on Oral Mucositis and outcomes like pain, dysphagia, quality of life, in 94 head and neck cancer patients submitted to concurrent chemoradiation. The majority of patients were treated for an oropharyngeal tumor, with a conventional radiation and a concurrent cisplatin every 3 weeks. Main endpoints were OM incidence and severity, pain intensity and RT interruptions. A crossover was used for patients in placebo-arm presented a grade 3 mucositis and/or a giant ulcer. In this particular case, LLLT density energy was double from 4J/cm2 to 8J/cm2. Laser was used daily during the chemoradiation with a punctual form and 10 seconds per point, which is shorter than time of treatment recommended by Bensadoun. Nevertheless, the incidence of grade ¾ OM was 6.4 % in the LLLT arm versus 48% in the placebo arm which is highly significant (HR = 0.13 and p< 0.001). The incidence of ulcer was also lower with active laser with 17% versus 51% (p<0.001). Beside this benefits, pain was less severe in patients treated with active laser (p=0.012), with less used narcotic analgesic (HR = 0.33, p<0.001), feeding tube insertion or gastrostomy (HR = 0.037, p= 0.005). No patients in this study had RT or CT interruption due to OM but almost half patients of the placebo group used the cross over.
Finally, many points of quality of life, like physical and emotional functioning (p=0.037), pain (p=0.043), swallowing (p=0.001) and fatigue (p=0.011), were significantly improved by laser therapy. In conclusion, the authors suggested that LLLT should be a new standard of care in this setting.
Recently, the largest sample study on this topic has been submitted to publication 20). It was a triple blinded randomized trial for 221 patients treated with a conventional radiotherapy (66 Gy, 33 fractions, 5 fractions/week) and cisplatin every three weeks. Power density and dosage were both low (24 mW and 3 J/point with a 1 cm2 spot size). LLLT was used every day prior to radiation. The incidence of severe mucositis (grade > 2) was significantly reduced with laser (23.4% vs 70%). Pain and dysphagia were also significantly improved by LLLT with a significant reduction in opiod analgesic use.
According to last Bensadoun's recommendations, a national multicentric phase III trial, double-blind with placebo controlled, started in France in 2009. This study is coordinated by the west oncologic institute Paul Papin (ICO Paul papin) and funded by a national public grant (PHRC 2008). The objective is to evaluate the effectiveness of a 100 mW and 660 nm diode laser on OM in advanced head and neck patients treated with concurrent chemoradiotherapy, with or without surgery. RT is delivered with a conformational or IMRT technique. Chemotherapy is a 5FU-CDDP protocol, or CDDP alone or Cetuximab, according to the exclusive or post-operative statement and to the co-morbidities of the patient.
Main endpoint is grade 3-4 OM incidence and secondary endpoints are the impact on nutrition, quality of life, treatment interruptions, DFS, OS and laser toxicity.
Laser is used daily when mucositis becomes greater than grade 1 and is interrupted when OM becomes less severe than grade 2. This schedule has been chosen to be less time-consuming as possible to respect medical limited availability, and because severe and not moderate mucositis is in our opinion the main target.
Among almost 15 French centers using soft laser, 7 are now opened for this study and 44 patients have been enrolled over a hundred patients planned. This study could be a new key stone to evaluate the efficacy of laser therapy on oral induced mucositis but new studies are needed to evaluate new laser technologies than can treat with different wavelengths not even pharyngeal mucositis which is actually not treated but also cutaneous toxicities, especially in patients receiving targeted therapy like cetuximab.
Conclusions
In summary, low level laser therapy represents more than a promising agent to prevent or treat cancer—therapy induced OM. With diode and new technologies, laser is now less time-consuming and extraoral applicators with specific wavelength could be helpful to treat other sites of mucositis and skin toxicities. Also it may be used by trained paramedical staff like nurses who can complete clinician contribution. We can now use published recommendations for soft laser parameters. This is important for different clinician communities that are concerned with oral mucositis and for the homogeneity of laser procedure in future trials.
According to the MASCC criteria, and the results of the meta-analysis, LLLT could be soon proposed with a level I of evidence, as a possible new standard of care in respect to the last recommendations published if intraoral application is performed.
Acknowledgement
The authors would like to thank:
Brigitte Lemarquand, scientific information officer, ICO Paul Papin
Dr Virginie Berger PhD, team manager and clinical research ICO Paul Papin
There are no conflicts of interest.
References
- 1: Bjordal JM, Bensadoun RJ, Tunèr J, Frigo L, Gjerde K, Lopes-Martins RA. (2011): A systematic review with meta-analysis of the effect of low-level laser therapy (LLLT) in cancer therapy-induced oral mucositis. Support Care Cancer, 19(8):1069-77 [DOI] [PubMed] [Google Scholar]
- 2: Bensadoun RJ, Franquin JC, Ciais G, et al. (1999). Low-energy He/Ne laser in the prevention of radio-induced mucositis. A multicenter phase III randomized study in patients with head and neck cancer. Support Care Cancer, 7(4): 244-252 [DOI] [PubMed] [Google Scholar]
- 3: Caillot E, Denis F. (2012): Mucites radio-induites buccopharyngées: actualités sur la prise en charge. Cancer/radiotherapie, 16 : 358-363 [DOI] [PubMed] [Google Scholar]
- 4: Elting LS, Keefe DM, Sonis ST, Garden AS, Spijjkervet FK, Barasch A, et al. (2008): Patient-reported measurements of oral mucositis in head and neck cancer patients treated with radiotherapy with or without chemotherapy: demonstration of increased frequency, severity, resistance to palliation, and impact on quality of life. Cancer, 15; 113(10): 2704-13 [DOI] [PubMed] [Google Scholar]
- 5: Rubenstein EB, Peterson DE, Schubert M, Keefe D, McGuire D, Epstein J, et al. (2004): Mucositis Study section of the Multinational Association for Supportive Care in Cancer; International Society for Oral Oncology. Cancer, 1;100(9 suppl): 2026-46 [Google Scholar]
- 6: Worthington HV, Clarkson JE, Eden OB. (2007): Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev,17(4): CD000978. [DOI] [PubMed] [Google Scholar]
- 7: Treister N, Sonis S. (2007): Mucositis: biology and management. Curr opin Otolaryngol Head Neck Surg, 15(2):123-9 [DOI] [PubMed] [Google Scholar]
- 8: Jang H, Lee H. (2012). Meta-analysis of pain relief effects by laser irradiation on joint areas: Photomed Laser Surg, 30(8):405-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9: De Paula Eduardo C, de Freitas PM, Esteves-Oliveira M, Aranha AC, Ramalho KM, Simoes A, et al. (2010): Laser phototherapy in the treatment of periodontal disease. A review. Lasers med Sci, 25(6):781-92 [DOI] [PubMed] [Google Scholar]
- 10: Corazza AV, Jorge J, Kurachi C, Bagnato VS. (2007): Photobiomodulation on the angiogenesis of skin wounds in rats using different light sources. Photomed Laser Surg, 25(2):102-6 [DOI] [PubMed] [Google Scholar]
- 11: Keefe DM, Shubert MM, Elting LS, Sonis ST, Epstein JB, Raber-Durlacher JE, et al. (2007): Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer, 1;109(5):820-31 [DOI] [PubMed] [Google Scholar]
- 12: Ciais G, Namer M, Schneider M, Demard F, Pourreau-Schneider N, Martin PM, et al. (1992): Laser therapy in the prevention and treatment of mucositis caused by anticancer chemotherapy. Bull Cancer, 79(2): 183-91 [PubMed] [Google Scholar]
- 13: Migliorati CA, Oberle-Edwards L, Schubert M. (2006): The role of alternative and natural agents, cryotherapy, and/or laser for management of alimentary mucositis. Support care cancer, 14(6): 533-40 [DOI] [PubMed] [Google Scholar]
- 14: Maiya AG, Sagar MS, Fernandes DJ. (2006): Effect of low helium-neon(He-Ne) laser therapy in the prevention and treatment of radiation induced mucositis in head and neck cancer patients. Indian J Res, 124: 399-402 [PubMed] [Google Scholar]
- 15: Arora H, Pai KM, Maiya A, Vidyasagar MS, Rajeev A. (2008): Efficacy of He-Ne laser in the prevention and treatment of radiotherapy-induced oral mucositis in oral cancer patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 105(2):180-6 [DOI] [PubMed] [Google Scholar]
- 16: Kuhn A, Heinzmann G, da Silva CA, et al. (2008): Low-level infrared laser therapy to prevent radiotherapy-induced oral mucositis: a randomized placebo-controlled study. J Oral laser Appl, 8:219-24 [Google Scholar]
- 17: Antunes HS, Herchenhorm D, Araujo CM, Cabral R, Ferreira EM, Small A, et al. (2011): Phase III trial of low-level laser therapy to prevent induced oral mucitis in head and neck cancer patients submitted to concurrent chemoradiation. J Clin Oncol 29 suppl abstr LBA5524 [Google Scholar]
- 18: Lima AG, Villar RC, de Castro GJ, Antequera R, Gil E, Rosalmeida MC, et al. (2011): Oral mucositis prevention by low-level laser therapy in head and neck cancer patients undergoing concurrent chemoradiotherapy: a phase III randomized study. Int J Radiat Oncol Biol Phys, 82: 270-5 [DOI] [PubMed] [Google Scholar]
- 19: Kuhn A, Vacaro G, Almeida D, et al. (2007): Low-level infrared laser therapy for chemo-or radiotherapy-induced oral mucositis: a randomized, placebo-controlled study. J Oral Laser Appl, 7:175-81 [Google Scholar]
- 20: Gautam AP, Fernandes DJ, Vidyasager MS, Maiya AG, Vadhiraja BJ. (2012): Low level laser therapy for concurrent chemoradiotherapy induced oral mucositis in head and neck cancer patients. A triple blinded randomized controlled trial. Radiother Oncol August 9 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 21: Cowen D, Tardieu C, Schubert M, et al. (1997): Low energy helium-neon laser in the prevention of oral mucositis in patients undergoing bone marrow transplant : results of a double blind randomized trial. Int J Radiat Oncol Biol Phys, 38: 697-703 [DOI] [PubMed] [Google Scholar]
- 22: Antunes HS, de Azevedo AM, da Silva Bouzas LF, et al. (2007): Low-power laser in the prevention of induced oral mucositis in bone marrow transplantation patients: a randomized trial. Blood, 109: 2250-5 [DOI] [PubMed] [Google Scholar]
- 23: Schubert MM, Eduardo FP, Guthrie KA, et al. (2007): A phase III randomized double blind placebo-controlled clinical trial to determine the efficacy of low level laser therapy for the prevention of oral mucositis in patients undergoing hematopoietic cell transplantation. Support care Cancer, 15: 1145-54 [DOI] [PubMed] [Google Scholar]
- 24: Clarkson JE, Worthington HV, Furness S, McCabe M, Khalid T, Meyer S. (2010): Interventions for treating oral mucositis for patients with receiving treatment. Cochrane Database Syst rev, Aug 4(8): CD001973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25: Bensadoun RJ, Nair RG. (2012): Low-level laser therapy in the prevention and treatment of cancer therapy-induced mucositis: 2012 state of the art based on literature review and meta-analysis. Curr Opin Oncol, 24(4): 363-70 [DOI] [PubMed] [Google Scholar]


