Abstract
Hepatocellular carcinoma (HCC) is rare in children. Progressive familial intrahepatic cholestasis type II (PFIC2 and also called BSEP ((Bile Salt Export Pump)) deficiency) is an inherited disease that initiates end-stage liver cirrhosis which can predispose to HCC. HCC can occur in 15% of patients with PFIC2. In this case report, an 11-month-old boy with PFIC 2 was admitted for liver transplant work up. The finding of HCC was made incidentally by histopathology on the explanted liver after suspiciously gross examination. In this article, we found that the radiology (US) alone is not enough to exclude HCC. Finally, we conclude that any case of PFIC 2 (male or female) needs routine screening of serum AFP concentration, advanced radiological examination (CT, MRI) as well as careful macroscopic examination of their explanted liver (triple assessment) to exclude HCC.
Keywords: Progressive familial intrahepatic cholestasis type 2, hepatocellular carcinoma, liver, triple assessment, MRI & CT scan
Introduction
PFIC is a disorder resulting in chronic liver disease during childhood. (1) The exact prevalence remains unknown, but the estimated incidence varies between 1/50,000 to 1/100,000 births. (6) Three different subtypes with localized genetic defects were described, PFIC-1 (mutation in the FIC1 locus at chromosome 18q21-q22), PFIC-2 (genetic defect localized at 2q24) resulting in a defect of the BSEP, and PFIC-3 (defect in the MDR3 gene) (1). Children with PFIC present clinically with pruritus, jaundice, hepatosplenomegaly, and growth failure. (1) Although HCC is rare in children, (2) any child ( male or female ) with PFIC2 is at risk for hepatobiliary malignancy (15% may develop HCC or cholangiocarcinoma). (3–4) Liver ultrasound(US) is the best basic imaging modality for focal or diffuse disease of the liver. But if unsuccessful, advanced radiological investigation like computed tomography (CT) or magnetic resonance imaging (MRI) is indicated (5). By consideration of the percentage of PFIC2 and HCC association, we think that we should find a unique estimation that may open a new door for further research.
Case Report
An 11-month-old Saudi boy, known case of PFIC2(confirmed by immunohistochemistry ) was admitted for liver transplant work up. There is no history of consanguinity. Physical examination reveals abdominal distention and hepatosplenomegaly. His biochemical and hematology laboratory “workup” was reported as normal GGT and elevation of serum alpha fetoprotein (AFP) (was 22.2). Ultrasound abdomen showed heterogeneous parenchyma of the liver and there was no defined focal lesion.
Because of unspecific radiological (US) picture, an initial radiological suspicious of HCC was not made. However, further radiological investigations are not done.
Later, the patient underwent the total hepatectomy that weighing 900 g and measuring 18 × 14 × 6.5 cm. Serial sectioning of the liver about 1 cm interval shows green to tan-brown firm cut surface with focal nodule measuring 2 cm in maximum diameter and located in segment VIII. Histopathological examination revealed HCC (Figures 1&2) in background of suggestive features of PFIC2 (Figures 3&4). CD 34 stain showing canalicular (capillarization of sinusoids) positivity of the HCC (Figure 5). A final diagnosis of HCC complicating PFIC2 was eventually made.
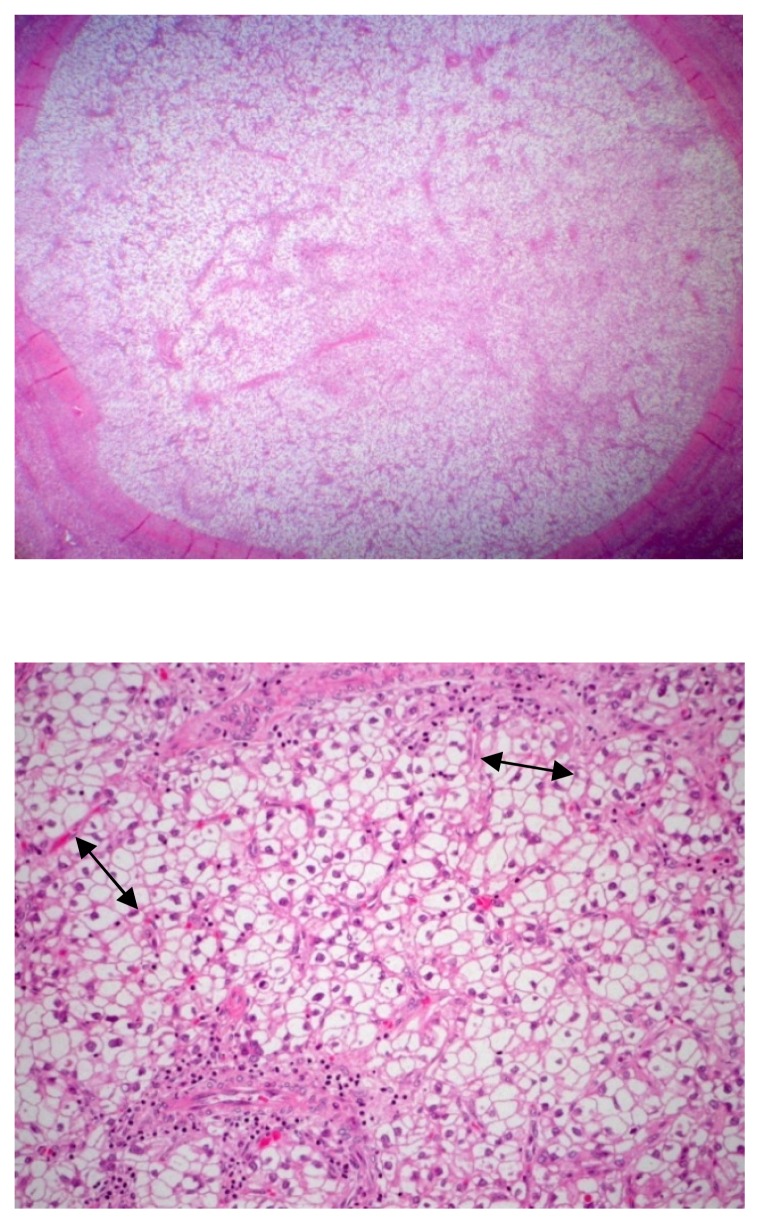
Fig. 1–2.
Hepatocellular carcinoma. Medium and low magnification showing a significant individual nodule(first picture) with predominate of clear cells with(2nd picture) greater than three cells thickness, distinct cells border and devoid of the portal tract.(H&E stain, 1: ×50 & 2: ×100)
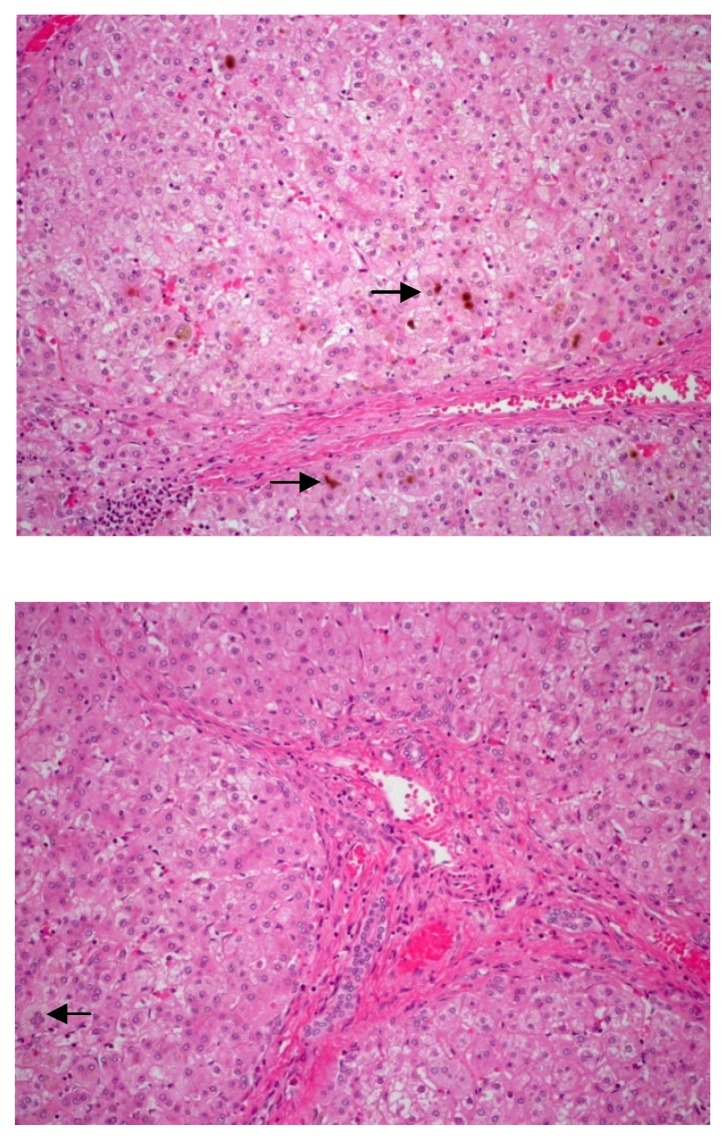
Fig. 3–4.
PFIC2. Medium and high magnification showing intralobular cholestasis with edema and multinucleation of hepatocytes.( H&E stain, 10x)
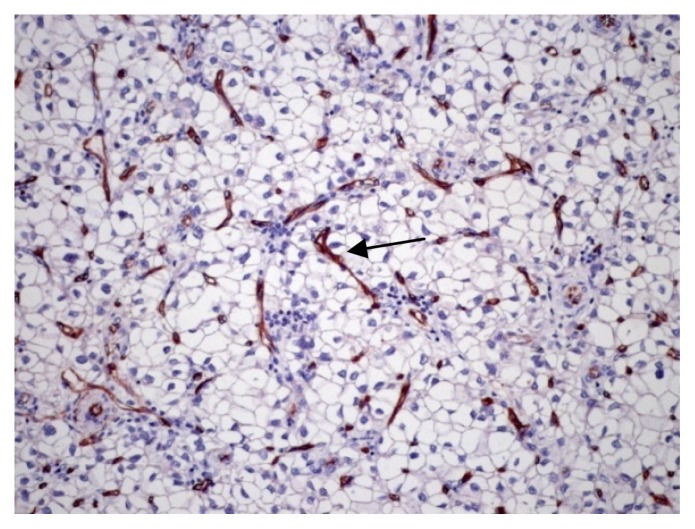
Fig. 5.
CD34 stain. Medium power magnification showing CD 34 canalicular positivity. (X100)
Discussion
We presented a rare case of HCC in a boy with PFIC2. It is not seen by US prior to transplantation. However, monitoring of HCC, especially in PFIC2 patients, should be offered from the first year of life. (6)
Our literature search showed that this difficult detection of hepatocellular carcinoma (as a focal lesion especially if it less than 3cm) by ultrasonography is quiet common in previous reported cases. (4&7–10)
Therefore, hepatocellular carcinoma in PFIC2 patient is frequently detected either incidentally or with metastasis. For example, in a previous study done by Knisely AS et al (4) showed that five cases (out of ten cases) diagnosed incidentally while other four cases (out of ten cases) diagnosed with metastasis. Subsequently, we need an exceptional approach for any PFIC 2 patient (male or female).
Our case represents a rare example of hepatocellular carcinoma complicating PFIC2 that need special evaluation (clinical suspicion, advanced radiological study and careful gross examination) as well as highly awareness of this commonly association.
Therefore, we can create what we called here as triple assessment. It is includes 1) clinical suspicion, 2) advanced radiological study and 3) careful gross examination to provide better management.
Conclusion
Because HCC is considered to be one of the rare malignant in children, its association with PFIC2 is frequently detected either incidentally or with metastasis. Therefore, we recommend triple assessment (clinical, advanced radiological and pathological assessment) of PFIC2 patients (male or female) and each of them should exclude HCC which was very useful in establishing the diagnosis in our case. Our case message here is to raise this approach that may open a new door for further research.
References
- 1.Ujhazy P, Ortiz P, Misra S, et al. Familial intrahepatic cholestasis 1: studies of localization and function. Hepatology. 2001;34:768–775. doi: 10.1053/jhep.2001.27663. [DOI] [PubMed] [Google Scholar]
- 2.Moore L, Bourne AJ, Moore DJ, Preston H, Byard RW. Hepatocellular carcinoma following neonatal hepatitis. Pediatr Pathol Lab Med. 1997;17:601–610. [PubMed] [Google Scholar]
- 3.Strautnieks SS, Byrne JA, Pawlikowska L, Cebecauerov D, Rayner A, Dutton L, Meier Y, Antoniou A, Stieger B, Arnell H, Ozçay F, Al-Hussaini HF, Bassas AF, Verkade HJ, Fischler B, Németh A, Kotalov R, Shneider BL, Cielecka-Kuszyk J, McClean P, Whitington PF, Sokal E, Jirsa M, Wali SH, Jankowska I, Pawłowska J, Mieli-Vergani G, Knisely AS, Bull LN, Thompson RJ. Severe bile salt export pump deficiency: 82 different ABCB11 mutations in 109 families. Gastroenterology. 2008;134:1203–1214. doi: 10.1053/j.gastro.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 4.Knisely AS, Strautnieks SS, Meier Y, Stieger B, Byrne JA, Portmann BC, Bull LN, Pawlikowska L, Bilezikçi B, Ozçay F, Lszl A, Tiszlavicz L, Moore L, Raftos J, Arnell H, Fischler B, Németh A, Papadogiannakis N, Cielecka-Kuszyk J, Jankowska I, Pawłowska J, Meln-Aldana H, Emerick KM, Whitington PF, Mieli-Vergani G, Thompson RJ. Hepatocellular carcinoma in ten children under five years of age with bile salt export pump deficiency. Hepatology. 2006;44:478–486. doi: 10.1002/hep.21287. [DOI] [PubMed] [Google Scholar]
- 5.Patel PR. Lecture Notes On Radiology. 2003. p. 129. [Google Scholar]
- 6.Anne DS, Emmanuel G, Christiane B, Emmanuel J. Progressive familial intrahepatic cholestasis: Review article. Orphanet Journal of Rare Diseases. 2009;4:11–12. doi: 10.1186/1750-1172-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quillin SP, Brink JA. Hepatoma complicating Byler disease. AJR Am J Roentgenol. 1992;159:432–433. doi: 10.2214/ajr.159.2.1321560. [DOI] [PubMed] [Google Scholar]
- 8.Esquivel CO, Gutierrez C, Cox KL, Garcia-Kennedy R, Berquist W, Concepcion W. Hepatocellular carcinoma and liver cell dysplasia in children with chronic liver disease. J Pediatr Surg. 1994;29:1465–1469. doi: 10.1016/0022-3468(94)90145-7. [DOI] [PubMed] [Google Scholar]
- 9.Yu SB, Kim HY, Eo H, Won JK, Jung SE, Park KW, et al. Clinical characteristics and prognosis of pediatric hepatocellular carcinoma. World J Surg. 2006;30:43–50. doi: 10.1007/s00268-005-7965-z. [DOI] [PubMed] [Google Scholar]
- 10.Ugarte N, Gonzalez-Crussi F. Hepatoma in siblings with progressive familial cholestatic cirrhosis of childhood. Am J Clin Pathol. 1981;76:172–177. doi: 10.1093/ajcp/76.2.172. [DOI] [PubMed] [Google Scholar]