Figure 3.
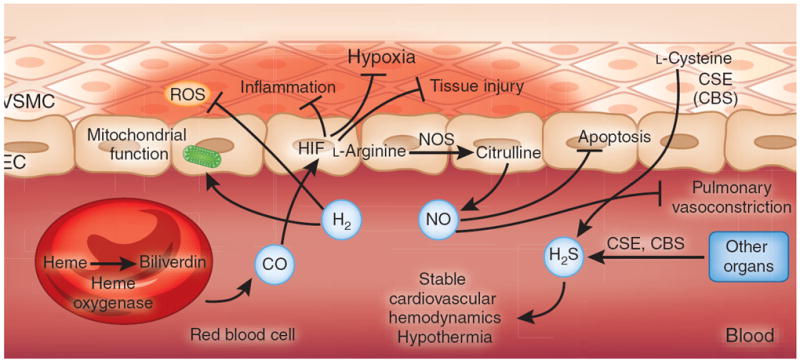
Therapeutic gases for the treatment of ischemia and reperfusion. CO, NO and H2S are considered to be endogenous gas transmitters. The predominant pathway for endogenous CO production involves the conversion of the erythrocyte-derived porphyrin molecule heme to biliverdin by the action of heme oxygenase, liberating CO as a byproduct141. CO has been implicated in attenuating inflammation and tissue injury through the stabilization of HIF. NO is produced predominantly from the endogenous metabolism of l-arginine to citrulline by NO synthase, which is expressed in multiple cell types, including vascular endothelia and neurons (not shown)105. Inhaled NO has been therapeutically used to attenuate hypoxic pulmonary vasoconstriction or to dampen apoptosis during ischemia and reperfusion142. H2S is produced endogenously through the metabolism of l-cysteine by the action of either cystathionine β-synthase (CBS) (expressed predominantly in the brain, nervous system, liver and kidney) or cystathionine γ-lyase (CSE) (expressed predominantly in liver and in vascular and nonvascular smooth muscle)143. Therapeutic use of inhaled H2S has been shown to induce a suspended-animation–like state characterized by hypothermia and stable cardiovascular hemodynamics, and to have protective effects during ischemia and reperfusion. In contrast to endogenous gas transmitters, no biological pathway for the generation of H2 has been described in mammalian cell systems. Therapeutic use of inhaled H2 has been shown to attenuate ischemia and reperfusion–associated accumulation of ROS and to preserve mitochondrial function. EC, endothelial cell; VSMC, vascular smooth muscle cell.
