Abstract
Introduction:
Children have non specific symptoms after mild head injury (MHI). It is difficult to define indication of CT scan among them. We aimed at identification of predictors of CT scan findings after MHI.
Materials and Methods:
Children aged ≤12 years with GCS 13-15 after head injury were retrospectively evaluated for their clinical and CT scan findings during January to March 2010. The variables used for detection of abnormal (positive) CT scan were age, gender, cause of injury (road traffic accident, fall, and assault), loss of consciousness, vomiting, ear or nose bleed, seizure, and GCS score.
Results:
A total of 133 children were included in study. Sixty nine (51.9%) children had abnormal CT findings. There was no statistical difference in patients with normal vs abnormal CT scan for presence of any of the variables evaluated.
Conclusion:
An abnormal CT scan cannot be reliably ruled out in a child with MHI based on symptoms; hence a policy of liberal CT scan based on clinical acumen is advisable.
Keywords: Clinical prediction rule, mild head injury, traumatic intracranial hematoma
Introduction
Mild head injury (MHI) is common in children. The exact epidemiology of pediatric MHI is difficult to estimate, as these children are managed by different specialists in different setups. In our head injury registry comprising 7,164 patients, children accounted for 20% of all head injury cases presenting to casualty.[1] Many children after MHI do not receive medical attention. When a child following MHI presents to the casualty/emergency room, it poses a potential problem for the treating neurosurgeon. Most of them may not have any significant injury, but few can have traumatic mass lesions requiring surgery or admission. Because of nonspecific symptoms of MHI in children, it is difficult to decide on the need for a computed tomography (CT) scan. To obviate this decision dilemma, a few clinical prediction rules (CPR) have been developed for MHI in children.[2] An ideal CPR should detect the entire patients at the risk of abnormal CT scan, with a minimum number of scans required to detect one positive case.[3] We aimed at identifying the predictability of positive CT scan from common symptoms after MHI in children.
Materials and Methods
This study was conducted at a tertiary-level referral center for the treatment of neurological, neurosurgical, and psychiatric patients. The center has a separate facility for trauma cases that serves patients from neighboring districts. Patients with head injury are evaluated by neurosurgery residents and data are entered in a structured “head injury proforma”, which consists of comprehensive clinical and head CT scan findings. The data are verified by a qualified neurosurgeon on duty. Data of all patients with MHI, defined as Glasgow Coma Scale (GCS) score ≥13, over a period from January 1, 2010, to March 15, 2010, were retrospectively reviewed, and children ≤ 12 years were identified. We chose the cut-off age limit as 12 years because of the policy of government hospitals in India for registration in pediatric department. CT scan findings were confirmed independently from images archived in the picture archival communication system (PACS) of the institute by senior author (DS). We used 15-point Child's GCS for all children.[4] To identify the predictors of our dependent variable “CT scan findings”, it was categorized as normal and abnormal. The abnormal CT scan was defined as any skull fracture, cerebral edema, epidural hematoma, subdural hematoma, cerebral contusion, intracerebral hematoma, and subarachnoid hemorrhage. The variables used for the analysis were age, gender, cause of injury (road traffic accident, fall, and assault), loss of consciousness, vomiting, ear or nose bleeding, seizure, and GCS (13, 14, and 15).
Statistical methods
The analysis was performed in SPSS 15 version (SPSS, Inc., Chicago, IL, USA; Network license, serial number 5047404). Data were expressed using descriptive statistics such as mean, standard deviation for continuous variables, frequency, and percentage for categorical variables. Statistical analysis was done using Chi-square test for categorical variables, and Mann–Whitney U test for continuous variables with 5% significance level. The discriminative ability of mentioned variables in predicting CT abnormality was evaluated using area under receiver operating characteristics (ROC) curve (AUC).
Results
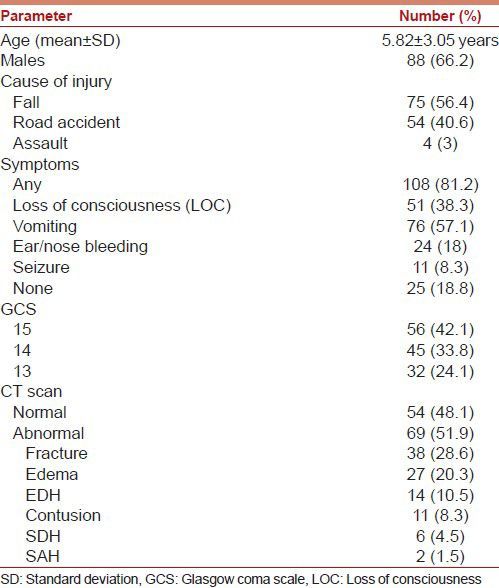
A total of 1,628 patients with MHI were evaluated during the study period; of these, 133 children ≤12 years (mean, 5.82 ± 3.05) were identified. Table 1 presents the general demographic profile of these children. Most of the children were male. The most common cause of injury was fall, and most patients presented in GCS 15. The common symptoms were loss of consciousness (LOC), vomiting, ear or nose bleeding, and seizure. Other symptoms such as headache, giddiness, vision impairment, speech change, weakness of face or limbs, walking difficulty, and cerebrospinal fluid (CSF) rhinorrhea were absent. The abnormal (positive) CT scan was seen in 51.9% of cases. The most common CT scan finding was skull fracture followed by cerebral edema. Three patients required surgery for the evacuation of epidural hematoma; all of them had at least one symptom.
Table 1.
Demographic profile of patients
The analysis of symptoms is given in Table 2. The presence of any symptom had an odds ratio of 1.80 (95% CI, 0.74-4.37) for a positive CT scan, but it was not significant. Among all symptoms, ear or nose bleeding had the highest odds ratio of 2.11 (95% CI, 0.83-5.34) for a positive CT scan, but it was not significant. The most common combination of symptoms was loss of consciousness and vomiting. Even the combination of symptoms was not significantly different in children with normal or abnormal CT scan. The estimates of symptoms and the AUC for the prediction of an abnormal CT scan are given in Tables 3 and 4. The sensitivity of presence of any symptom is good, but specificity is poor for abnormal CT scan. The AUC for any symptom was 0.545 (95% CI, 0.446-0.643), which is poor [Figure 1a]. The AUC for individual symptoms was also poor [Figure 1b].
Table 2.
Analysis of symptoms
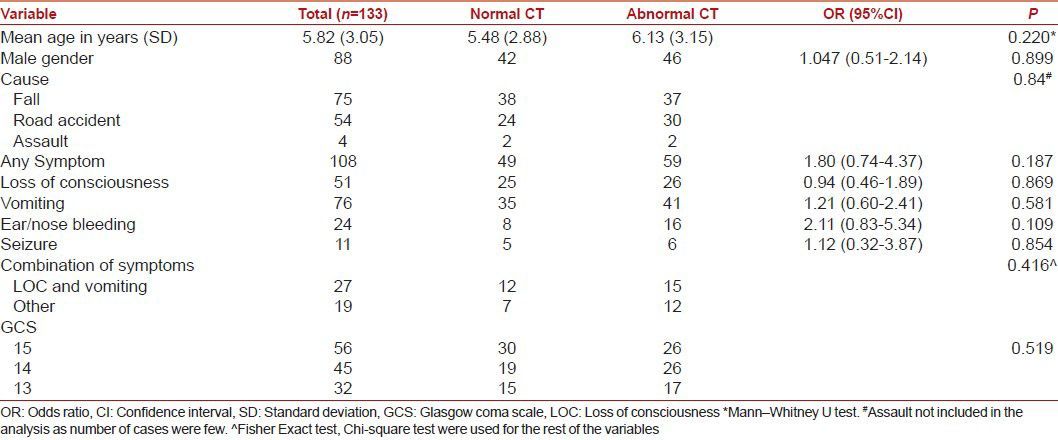
Table 3.
Sensitivity and specificity for presence of any symptom
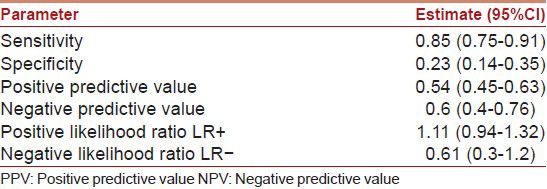
Table 4.
Area under receiver operating characteristics curve
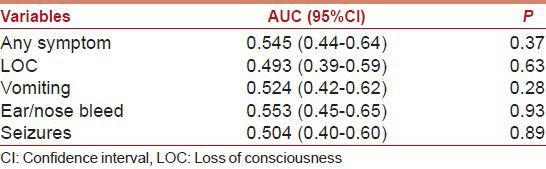
Figure 1.
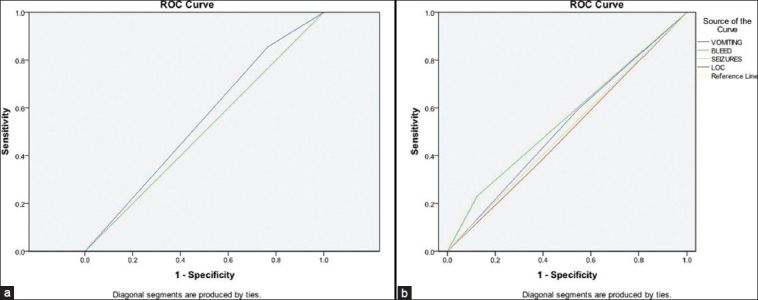
(a) Area under receiver operating characteristics (ROC) curve (AUC) for the presence of any symptom (b) ROC AUC for all symptoms
Discussion
Head injuries are common in children, but the majority of them are mild. Most head-injured children are conscious on arrival to casualty and do not have neurological deficit. However, such a patient constitutes a potential problem for neurosurgeons because a child with an apparent MHI can rarely develop an intracranial hematoma, deteriorate, and die. There is controversy regarding the policy for hospital admission and evaluation with CT scan for these children. A CT scan is desirable for children with MHI as it is useful for detection of a clinically significant intracranial lesion, prognostication, and decision for discharge. Children with MHI and brain lesions on CT scan have greater impairment on cognitive testing.[5] On the other hand, children with normal CT scan after MHI can be discharged, and hospitalization is generally unnecessary.[6] However, CT scan is not advisable for all children because of a remote risk of cancer.[7] In a recent study on cancer due to CT scan, the authors found that the use of CT scans in children to deliver cumulative doses of about 50 mGy (i.e. 2-3 CT scans) almost tripled the risk of leukemia, and doses of about 60 mGy tripled the risk of malignant brain tumor. This finding translates into one excess case of leukemia and one excess case of brain tumor per 10,000 CT scans. The authors mentioned that clinical benefits of CT scan should outweigh the small absolute risks, and justification of any CT scan is important.[7]
To obviate unnecessary CT scans, many guidelines are available for indication of CT scan for MHI in adults.[3] Among these, Canadian CT Head Rule (CCHR) is the most widely validated rule, with a sensitivity of 99-100% and a specificity of 48-77%.[8,9,10] A few CPR are available for the need for CT scan in children with MHI.[10,11,12,13,14] These rules differ considerably in population, predictors, outcomes, methodologic quality, and performance. Many of them are not validated in a separate population, and their impact on practice has not been assessed. No single CPR is applicable to all patients. The range of sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) of these rules are 95-100%, 26-87%, 99-100%, and 5-12%, respectively.[2,10,11] The highest quality CPR for children with MHI are the Canadian assessment of tomography for childhood head injury (CATCH), Children's head injury algorithm for the prediction of important clinical events (CHALICE), and Pediatric Emergency Care Applied Research Network (PECARN).[15,16,17,18] The symptoms and signs included in these CPR, with a decreasing order of probability of intracranial injury, include depressed or basal skull fracture, focal neurological deficit, coagulopathy, post-traumatic seizures, previous neurosurgery, visual symptoms, bicycle and pedestrian motor vehicle accident, loss of consciousness, vomiting, severe or persistent headache, amnesia, GCS < 14, intoxication, and scalp hematoma/laceration.[10] The dependant variable abnormal (positive) CT scan in these rules included the following CT scan findings: Skull fracture, epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intraventricular hemorrhage, cerebral contusion, and cerebral edema. Few rules also defined significant injury as any CT scan finding that may require neurosurgical intervention, intracranial pressure monitoring, or admission to intensive care unit.[10] In our patient population, only four symptoms were present: Vomiting, loss of consciousness, ear or nose bleeding, and seizures. We did not include scalp injury as a variable because it has little diagnostic value.[10] We do not perform coagulation profile for patients with MHI at our institute; hence, we did not include this variable. Post-traumatic amnesia (PTA) is also an important predictor of abnormal CT scan. The emergence from PTA is difficult to assess in children; hence, we did not include this variable. We included all CT scan findings listed above as inclusion criteria for abnormal (positive) CT scan. We did not define separately significant intracranial injury. We did not include the need for surgery as a dependant variable since we had only three cases requiring surgery. The analysis of symptoms revealed slightly different estimates for the positivity of CT scan as compared to literature. The sensitivity and negative predictive value were less in our study. This means that one cannot reliably rule out the possibility of an abnormal CT scan in children with MHI without any symptoms.
Our study had certain limitations. The patient profile in our study included only the patients who underwent CT scan. We do not have the estimate of other children with MHI who did not undergo CT scan. We did not have as many patients in GCS 15 as in other studies; this itself shows a referral bias. We also had a higher rate of abnormal CT scan than other studies. The probable reason for higher positivity was inclusion of skull fracture, which was not included in other studies.[13,15,16,17] However, in spite of these limitations, our study answers one important question for neurosurgeons. A child with MHI presenting to a neurosurgeon should undergo CT scan if he/she has any of the following symptoms: Vomiting, loss of consciousness, ear/nose bleeding, and seizures. A child with MHI without any symptoms may require a CT scan depending on the clinical acumen of the evaluating neurosurgeon. A good clinical judgment based on experience is a better strategy than CT scan for the all versus discharge-all approach.
Based on our study, one cannot reliably rule out an abnormal CT scan in a child with MHI; hence, a policy of liberal CT scan is advisable. The immediate benefits of CT outweigh the remote risk of cancer in many circumstances. The diagnostic accuracy and speed of scanning cannot be replaced with any other modality, and it will be in practice worldwide.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gururaj G, Kolluri SVR, Chandramouli BA, Subbakrishna DK, Kraus JF. Traumatic Brain Injury. National Institute of Mental Health and Neuro Sciences. 2005 Publication no. 61. [Google Scholar]
- 2.Maguire JL, Boutis K, Uleryk EM, Laupacis A, Parkin PC. Should a head-injured child receive a head CT scan? A systematic review of clinical prediction rules. Pediatrics. 2009;124:e145–54. doi: 10.1542/peds.2009-0075. [DOI] [PubMed] [Google Scholar]
- 3.Shukla D, Devi BI. Mild traumatic brain injuries in adults. J Neurosci Rural Pract. 2010;1:82–8. doi: 10.4103/0976-3147.71723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirkham FJ, Newton CR, Whitehouse W. Paediatric coma scales. Dev Med Child Neurol. 2008;50:267–74. doi: 10.1111/j.1469-8749.2008.02042.x. [DOI] [PubMed] [Google Scholar]
- 5.Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, et al. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. J Neurosurg Pediatr. 2008;1:461–70. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- 6.Holmes JF, Borgialli DA, Nadel FM, Quayle KS, Schambam N, Cooper A, et al. Do children with blunt head trauma and normal cranial computed tomography scan results require hospitalization for neurologic observation? Ann Emerg Med. 2011;58:315–22. doi: 10.1016/j.annemergmed.2011.03.060. [DOI] [PubMed] [Google Scholar]
- 7.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391–6. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 9.Stiell IG, Clement CM, Rowe BH, Schull MJ, Brison R, Cass D, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294:1511–8. doi: 10.1001/jama.294.12.1511. [DOI] [PubMed] [Google Scholar]
- 10.Pandor A, Goodacre S, Harnan S, Holmes M, Pickering A, Fitzgerald P, et al. Diagnostic management strategies for adults and children with minor head injury: A systematic review and an economic evaluation. Health Technol Assess. 2011;15:1–202. doi: 10.3310/hta15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palchak MJ, Holmes JF, Vance CW, Gelber RE, Schauer BA, Harrison MJ, et al. A decision rule for identifying children at low risk for brain injuries after blunt head trauma. Ann Emerg Med. 2003;42:492–506. doi: 10.1067/s0196-0644(03)00425-6. [DOI] [PubMed] [Google Scholar]
- 12.Haydel MJ, Shembekar AD. Prediction of intracranial injury in children aged five years and older with loss of consciousness after minor head injury due to nontrivial mechanisms. Ann Emerg Med. 2003;42:507–14. doi: 10.1067/s0196-0644(03)00512-2. [DOI] [PubMed] [Google Scholar]
- 13.Atabaki SM, Stiell IG, Bazarian JJ, Sadow KE, Vu TT, Camarca MA, et al. A clinical decision rule for cranial computed tomography in minor pediatric head trauma. Arch Pediatr Adolesc Med. 2008;162:439–45. doi: 10.1001/archpedi.162.5.439. [DOI] [PubMed] [Google Scholar]
- 14.Pickering A, Harnan S, Fitzgerald P, Pandor A, Goodacre S. Clinical decision rules for children with minor head injury: A systematic review. Arch Dis Child. 2011;96:414–21. doi: 10.1136/adc.2010.202820. [DOI] [PubMed] [Google Scholar]
- 15.Osmond MH, Klassen TP, Wells GA, Correll R, Jarvis A, Joubert G, et al. Pediatric Emergency Research Canada (PERC) Head Injury Study Group. CATCH: A clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ. 2010;182:341–8. doi: 10.1503/cmaj.091421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunning J, Daly JP, Lomas JP, Lecky F, Batchelor J, Mackway-Jones K, et al. Children’shead injury algorithm for the prediction of important clinical events study group. Derivation of the children's head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Child. 2006;91:885–91. doi: 10.1136/adc.2005.083980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Jr, Atabaki SM, Holubkov R, et al. Pediatric Emergency Care Applied Research Network (PECARN). Identification of children at very low risk of clinically-important brain injuries after head trauma: A prospective cohort study. Lancet. 2009;374:1160–70. doi: 10.1016/S0140-6736(09)61558-0. [DOI] [PubMed] [Google Scholar]
- 18.Lyttle MD, Crowe L, Oakley E, Dunning J, Babl FE. Comparing CATCH, CHALICE and PECARN clinical decision rules for paediatric head injuries. Emerg Med J. 2012;29:785–94. doi: 10.1136/emermed-2011-200225. [DOI] [PubMed] [Google Scholar]


