Abstract
Presence of cholesteatoma in the middle ear of the patients with chronic mucosal otitis media has been reported in the literature. But presence of cholesteatoma only in the mastoid, in the absence of cholesteatoma in the middle ear of a patient with chronic mucosal otitis media, is not reported in the literature. In this article three cases of mastoid cholesteatoma, in patients with a clinical picture of chronic mucosal otitis media is reported along with the literature review.
Keywords: Mastoid, Cholesteatoma, Metaplasia
Introduction
Anatomical experiments has shown that artificially induced inflammation in the middle ear is associated with metaplasia to squamous epithelium, but the finding of epithelial cyst in chronic mucosal otitis media has not been recorded, unless there has been previous surgery when implantation may have occurred [1].
Presence of cholesteatoma only in the mastoid, in the absence of any cholesteatoma in the middle ear of a patient with chronic mucosal otitis media, is not reported in the literature. Three cases of mastoid cholesteatoma, in patients with chronic mucosal otitis media who never had any trauma or ear surgery in the past, are reported and its etiopathogenesis is discussed.
Case Reports
Case 1
A 24 years old female patient presented with the history of recurrent history of left ear discharge and decreased hearing of 6 years duration. During every episode, patient had ear pain with mucopurulent profuse ear discharge. Patient had relief from ear pain and ear discharge with antibiotic therapy.
The present episode of ear pain and ear discharge started 2 months back. It was mucopurulent foul-smelling discharge. After treatment with two courses of antibiotics, patient had relief from pain but not from ear discharge. Patient never had any dizziness or neck pain. Patient never had any surgical treatment for the ear disease. Patient was referred to otolaryngology clinic for further management.
On examination left pinna and post aural area were normal. There was no tenderness over the mastoid region. External auditory canal was normal. Otoscopic examination showed a central perforation in the pars tensa involving all the four quadrants. Middle ear mucosa was congested and scanty, mucopurulent discharge was present. Right ear examination was normal. Tuning fork tests suggested a conductive type of hearing loss in the left ear. Nose, paranasal sinuses and throat examination findings were normal. Ear swab culture showed Pseudomonas aeruginosa organism. Pure tone audiogram showed conductive deafness in the left ear. CT scan of the temporal bones showed features suggestive of mastoiditis on the left side.
As the examination findings suggestive of tubotympanic type of otitis media, patient was advised to undergo mastoidectomy with tympanoplasty. Under local anesthesia, left mastoid bone was exposed. Surprisingly, a 3mm × 4 mm opening was seen 15 mm behind the spine of Henle (Fig. 1). Cortical mastoidectomy was started carefully. Just beneath the opening, a whitish cystic mass measuring 9 mm × 6 mm was found and mastoid cells showed hypertrophic mucosa. Hypertrophic mucosa and mass were removed. Ossicular chain was intact and there was no cholesteatoma in the middle ear. Cortical mastoidectomy with type-1 tympanoplasty was done.
Fig. 1.

Intraoperative photograph showing oval shape erosion over the mastoid cortex
Postoperative period was uneventful. Histopathological examination of the mass removed from the mastoid cavity, showed the features of cholesteatoma (Fig. 2). After 6 months, pure tone audiogram showed closure of air bone gap. Patient did not have any problem during follow-up period of 1 year.
Fig. 2.
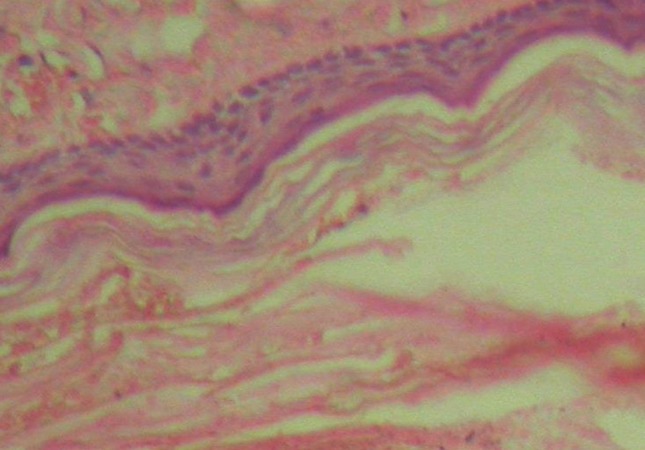
Photomicrograph of cholesteatoma showing stratified squamous epithelium and lamellar sheets of keratin (H&E: high power)
Case 2
A 36 year old male patient came with history of recurrent left ear discharge for the past 18 years. Patient had only partial relief from medical treatment. The present episode of ear discharge started 3 months back and it was scanty mucopurulent and occasionally foul smelling. It was not associated with fever or ear pain. As the patient did not get any relief from few courses antibiotics tablets and antibiotics ear drops, he was referred to major hospital for further management.
On examination patient had central perforation involving the antero inferior and antero superior quadrant of the pars tensa on the left side. Tympanosclerotic patch was present over the posterior inferior part of the eardrum (Fig. 3). Discharge was scanty, yellowish and foul smelling. There was no mastoid tenderness. Right ear, throat, nose and paranasal sinuses were normal. Tuning fork tests results were suggestive of conductive type of hearing loss on the left side. Ear swab culture showed P.aeruginosa organism.PTA showed conductive type of hearing loss on the left side. CT scans of the temporal bone showed soft tissue mass in the mastoid cavity surrounded by sclerotic bone on the left side (Fig. 4).
Fig. 3.
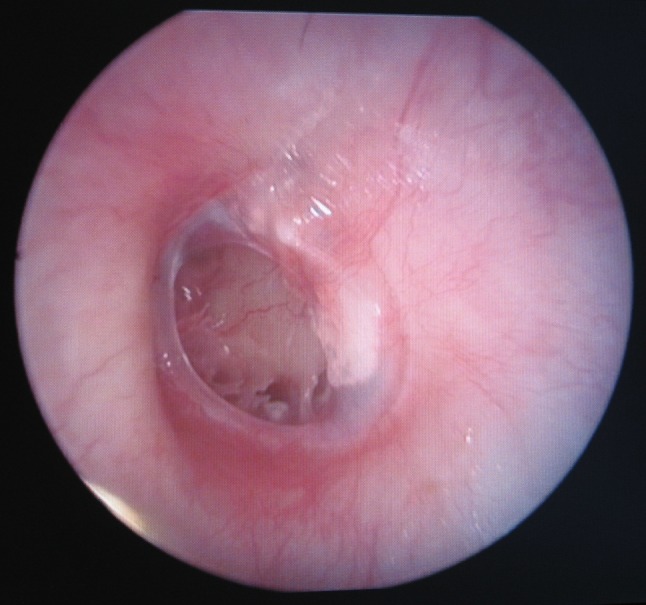
Endoscopic picture showing perforation in the antero inferior and antero superior quadrant of the pars tensa and tympanosclerotic patch on the left side
Fig. 4.

CT scan picture of the temporal bone showing soft tissue mass in the mastoid cavity and surrounding sclerotic bone on the left side
With a clinical diagnosis of chronic mucosal otitis media patient was advised mastoidectomy with tympanoplasty. Patient underwent mastoid exploration under local anesthesia. A small whitish cystic mass was found in the mastoid cavity and it was removed. Ossicles were intact and there was no cholesteatoma in the middle ear. Tympanosclerotic patch was removed from the tympanic membrane and type-1 tympanoplasty was done. Histopathological examination of the removed mass showed picture of cholesteatoma. Patient did not have any problem during the follow-up period of 1 year.
Case 3
An 18 year old female patient came with history of left ear discharge for the past 1 years. It was intermittent scanty and occasionally foul smelling. On examination she had a central perforation in the postero-superior part of the pars tensa with a thin posterior rim (Fig. 5). There was a scanty mucopurulent discharge. Tuning fork test showed conductive hearing loss on the left side and it was confirmed by PTA. Ear swab culture showed P. aeruginosa organisms. CT scan showed sclerosing mastoiditis changes and a small soft tissue mass near the tip on the left side (Fig. 6). With the diagnosis of chronic mucosal type of otitis media patient was advised mastoidectomy with tympanoplasty. With a clinical diagnosis of chronic mucosal otitis media patient was advised mastoidectomy with tympanoplasty. Patient underwent mastoid exploration under local anesthesia. On mastoid exploration a small whitish cystic mass was found in the lower part of the mastoid cavity nearer to the mastoid tip. It was completely removed and sent for histopathological examination. Middle ear and ossicles were normal and type-1 tympanoplasty was done. Histopathological examination of the removed mass showed keratinized squamous epithelium. Post operative period was uneventful. Patient did not have any problem during the follow up period of 1 year.
Fig. 5.
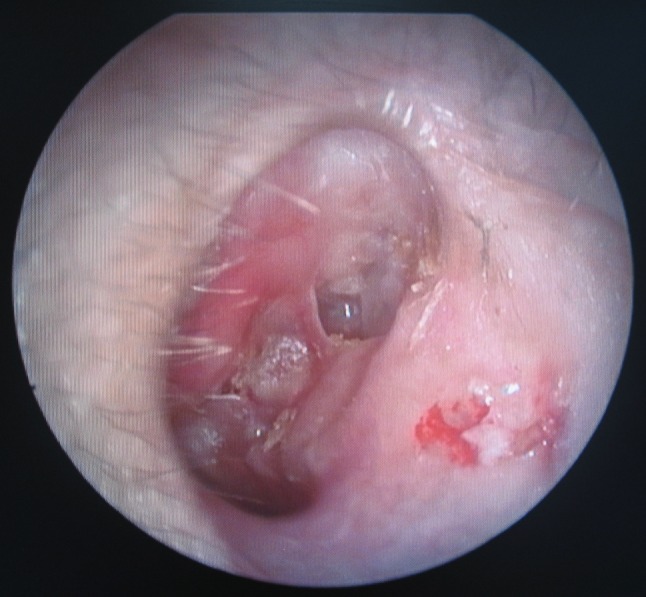
Endoscopic picture showing central perforation in the postero-superior part of the pars tensa on the left side
Fig. 6.

CT scan picture showing sclerosing mastoiditis changes and a small soft tissue mass near the tip of the mastoid on the left side
Discussion
Cholesteatoma is a cystic lesion formed from keratinizing stratified squamous epithelium, the matrix of which is composed of epithelium that rests on a stroma of varying thickness, the prematrix. It is mainly divided into congenital and acquired types [2]. Acquired cholesteatoma is classified into primary and secondary types. Primary acquired cholesteatoma refers to lesions with no previous history of otitis media, whereas secondary acquired cholesteatoma is said to follow active middle ear infection [3].
All three patients had ear discharge. Ear examination showed tubotympanic type of disease in the left ear and ossicular chain was intact in all the three cases. Cholesteatoma was found only in the mastoid during mastoidectomy in all the three patients. Hence, this was secondary acquired cholesteatoma. None of our patients had dizziness or neck pain which is suggestive of congenital cholesteatoma.
The pathophysiology of acquired cholesteatoma is controversial and its precise pathogenesis has been debated for more than two centuries. Four main theories have been used to explain he development of cholesteatoma:
Central perforations are rarely associated with cholesteatoma [3]. Experimental models by Massuda et al. [2, 4] has shown that epithelial migration of keratinizing epithelium at the edges of the tympanic membrane perforation as a possible cause of cholesteatoma development. In the present cases patients had central perforation and cholesteatoma was not present in the middle ear and attic, but it was found in the mastoid bone.
Metaplasia from the low cuboidal epithelium usually found in the in middle ear to a keratinized squamous epithelium has been postulated as the cause of cholesteatoma in the patient with chronic or recurrent otitis media [5]. Sade et al. [6], in a histopathological study, observed squamous metaplasia of middle ear epithelium in patients with cholesteatoma, particularly when granulation tissue was a prominent feature [3]. The rationale of the metaplasia theory is based on the well documented change of respiratory epithelium in other part of the body to squamous epithelium in the face of chronic irritation and inflammation [5].
Antral cholesteatoma are complication of chronic mastoiditis. This entity is difficult to diagnose radiologically from coalescent mastoiditis. It may break in through the mastoid tip and can result in a Bezold’s abscess [7]. In the present cases also CT scans of temporal bones showed features suggestive of mastoiditis and soft tissue mass on the affected side.
It is postulated that secondary to episodes of inflammation areas of metaplasia to squamous epithelium occurs in middle ear mucosa and then expand to create a cyst, as is known to occur with surgically implanted squamous epithelium [1]. This is observed frequently in revision middle ear surgery and described as “cholesteatoma pearl” formation that is the result of trapped viable keratinocytic formation that leads to a small localized cholesteatoma [2].
In the first case patient had cholesteatoma in the mastoid, which had eroded the lateral surface of the mastoid bone, 15 mm behind the spine of Henle and whitish mass was seen below the opening. Rest of the mastoid showed air cells with hypertrophic mucosa. In the second case mass was found in the antrum and in the third case mass was found near the tip. In all the cases there was no cholesteatoma in the middle ear. Patients never had any ear surgery in the past. The formation of cholesteatoma only in the mastoid may be due to metaplasia from the low cuboidal epithelium usually found in the in mastoid air cells, to a keratinized squamous epithelium secondary to chronic otitis media.
Chole et al. [8] have examined human and gerbil cholesteatomas for evidence of biofilms. Most cholesteatomas showed evidence of biofilm formation for both gram negative and gram positive bacteria [9]. Wang et al. [10] have shown that otopathogenic strains of P. aeruginosa are capable of producing biofilms and become highly resistant to antimicrobial therapy. These findings strongly suggest a role of bacterial biofilm in the pathogenesis of cholesteatoma [9]. In the present cases also Pseudomonas organisms were isolated from cultures of ear swabs.
Conclusion
In the present series all the patients had a clinical picture of chronic mucosal otitis media. During surgery cholesteatoma was found only in the mastoid, in the absence of any cholesteatoma in the middle ear. Presence of cholesteatoma only in the mastoid, in the absence of any cholesteatoma in the middle ear of patients with clinical picture of chronic mucosal otitis media, can be explained only on the basis of theory of metaplasia. In all these patient ear swab culture showed P. aeruginosa organism. Otopathogenic strains of P. aeruginosa may also play a role in the pathogenesis of mastoid cholesteatoma.
References
- 1.Browning GG (1997) Aetiopathology of inflammatory conditions of the external and middle ear, vol. 3. In: Kerr AG, Booth JB (eds). Scott Brown’s otolaryngology, 6th edn. Butterworth-Heinemann, Oxford, pp 3/3/1–3/3/37
- 2.Semaan TM, Megerian CA. The pathology of cholesteatoma. Otolaryngol Clin North Am. 2006;39:1143–1159. doi: 10.1016/j.otc.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Robin Y (1998) Chronic suppurative otitis media: cholesteatoma. In: Ludman H, Wright T. Diseases of the ear, 6th edn. Arnold Publications London. pp 386–397
- 4.Massuda ET, Oliveira JA. A new experimental model of acquired cholesteatoma. Laryngoscope. 2005;115(3):481–485. doi: 10.1097/01.mlg.0000157826.15756.67. [DOI] [PubMed] [Google Scholar]
- 5.Sculerati N, Bluestone CD. Pathogenesis of cholesteatoma. The Otolaryngol Clin North Am. 1989;22:859–868. [PubMed] [Google Scholar]
- 6.Sade J, Babiacki A, Pinkus G. The metaplastic and congenital origin of cholesteatoma. Acta Laryngologica (Stockholm) 1983;96:119–129. doi: 10.3109/00016488309132882. [DOI] [PubMed] [Google Scholar]
- 7.Liu DPC, Bergeron RT. Contemporary radiologic imaging in the evaluation of middle ear–attic–antral complex cholesteatomas. Otolaryngol Clin North Am. 1989;22:897–909. [PubMed] [Google Scholar]
- 8.Chole R, Faddis B. Evidence of microbial biofilms in cholesteatomas. Arch Otolaryngol Head Neck Surg. 2002;128:1129–1133. doi: 10.1001/archotol.128.10.1129. [DOI] [PubMed] [Google Scholar]
- 9.Macassey E, Dawes P. Biofilms and their role in otolaryngological disease. J Laryngol Otol. 2008;122:1273–1278. doi: 10.1017/S0022215108002193. [DOI] [PubMed] [Google Scholar]
- 10.Wang EW, Jung JY, Pashia ME, Nason R, et al. Otopathogenic Pseudomonas aeruginosa strains as competent biofilm formers. Arch Otolaryngol Head Neck Surg. 2005;131(11):983–989. doi: 10.1001/archotol.131.11.983. [DOI] [PubMed] [Google Scholar]


