Figure 1.
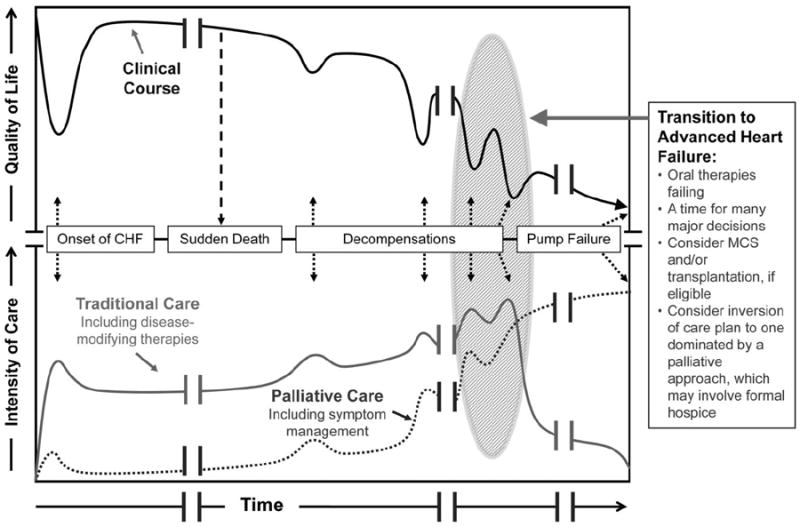
A depiction of the clinical course of heart failure with associated types and intensities of available therapies. Black line: Patients tend to follow a progressive, albeit nonlinear, decline in health-related quality of life as the disease progresses; this course can be interrupted by sudden cardiac death caused by arrhythmia or can end in a more gradual death caused by progressive pump failure. Gray line: At disease onset, multiple oral therapies are prescribed for cardiac dysfunction and/or treatment of comorbidities. As disease severity increases, the intensity of care may increase in parallel, with intensification of diuretics, addition of an implantable cardioverter-defibrillator/cardiac resynchronization therapy for those eligible, and increasing interaction with the medical system through ambulatory visits and hospitalizations, until the time when standard therapies begin to fail (transition to advanced heart failure). Dotted line: Palliative therapies to control symptoms, address quality of life, and enhance communication are relevant throughout the course of heart failure, not just in advanced disease; palliative therapies work hand in hand with traditional therapies designed to prolong survival. The critical transition into advanced heart failure from the medical perspective is often followed by a transition in goals of care from the patient and family perspective, wherein palliative therapies may become the dominant treatment paradigm (for the majority of patients in whom transplantation and mechanical circulatory support are not an option). Clinicians must recognize the transition to advanced heart failure so that therapeutic options can be considered in a timely fashion and patients are able to proactively match medical decisions to clinical realities. CHF indicates chronic heart failure; MCS, mechanical circulatory support. Modified from Lanken et al;21 reprinted with permission of the American Thoracic Society. Copyright © 2012, American Thoracic Society.
