Abstract
India's one billion plus strong population presents huge health care needs. Presently, approximately 250,000 general practitioners and 30,000 Government doctors are a part of the Indian healthcare workforce, but 80% of them are based in urban India. Problems which plague healthcare delivery and attributed to physician practice may be enumerated as - physicians (1) lack competencies, (2) lack updating, (3) prescribe irrationally (pressures from pharmaceutical companies and patients), (4) practice unethically, (5) refer excessively to specialists and other clinical professionals, and (6) investigate for diseases without justification. A multi-competent Family Physician who could provide a single-window, ethical, and holistic healthcare to patients and families is the need of the hour. Therefore, training, equipping, and empowering these 250,000 doctors to become such physicians will reduce health costs considerably. Distance medical education using all the andragogic methods can be used to train large number of individuals without displacing them from their work-places. Distance learning provides a useful interface for rapidly developing a specialized pool of doctors practicing and advocating family medicine as most-needed discipline. This motivated CMC Vellore, a premier institution for medical education in India, to start a the “refer less resolve more initiative” by offering “two year family medicine diploma course” by distance mode. This is an innovatively-written program consisting of problem-based self-learning modules, video-lectures, video-conferencing, and face-to-face contact programs. Ten secondary level hospitals, across the country, under the supervision of national and international family medicine faculty form the pillars of this program. This distance learning program offered by CMC Vellore has become the platform for change as there is special focus is on ethics, rational prescribing, consultation skills, application of family medicine principles; and practical demonstration of compassionate, cost-effective and high-quality care. The change in attitude has resulted in transformation in three major aspects of practice: professional, ethical, and patient care. So far, 942 private practitioners and 177 government doctors have been enrolled.
Keywords: Critical mass, distance education, family medicine, National Rural Health Mission, refer less
Bdackground
India's one billion plus strong population presents huge health care needs. At a glance, we seem to be doing well with more than 300[1] medical colleges churning out 30,000[2] odd medical graduates in a year, but sadly, there is no standardization of medical education across the country. The majority (two-thirds) of these graduating doctors do not get into a Post-Graduation course and they opt for General Practice (individually or in corporate setups) or join the Government Primary Health Centers. At present, there are 250,000 doctors in India who identify themselves to be in this category.[3,4] However, there is a grave mismatch in the distribution and population based representation of these doctors. The majority (73%) of India's rural population is catered by a minority (20%) of these doctors, while a vast majority (80%) of the doctors is concentrated in cities, where a little more than a fifth (27%) of the population lives. In the urban scenario, one observes a specialist culture where if a patient has a simple ailment like headache, he or she visits a neurologist and then gets referred to various specialists to sort out his/her headache and each specialist orders a battery of investigations escalating the health costs enormously, for the individuals and the healthcare system.[5,6] But in a rural scenario, there is no access to care for basic healthcare needs and the referrals to hospitals which are located at far away places, have resulted in increased morbidity and mortality. In both the scenarios, outcomes can be a lot better, if we have multi-competent specialists; who can provide a single-window, holistic healthcare to the communities they cater to.
In the public sector, presently there is an arrangement for a pentagram of five consultants to man the FRU (First Referral Units): Surgeon, Physician, ObGyn, Pediatrician, and Anesthetist.[7,4] Presently, 3215 FRUs[8] are functional (not fully manned), but the recommended need is for almost double the number of current FRUs (7415 FRUs). Approximately 700 specialists graduate and are available per year in each specialty. Among them, 10% (70) will join any FRU in a given year. That should take 100 years to fill up the gaps and the available positions. Even if the target is achieved, cases will fall between the cracks: Psychiatry, Orthopedics, Dermatology, etc. Having a specialist who does only a fraction of the work is expensive for the health system.[9] Well trained, multi-competent, attitude-altered family physicians again seem to be the solution for this serious mismatch between population needs and access to care![10]
Having said that a family physician is the need of the hour, we also have to realize that to design a training to equip doctors to become this multi-competent specialist, one has to address six major concerns: (1) lack of competencies, (2) lack of updating, (3) irrational Prescribing (pharmaceutical company or patient pushed), (4) unethical practices (kick-backs from imaging centers, laboratories etc.), (5) excessive referrals to specialists and (6) unnecessary investigations.
The Solution
In order to influence the culture of medical practice in India, there is a need to evolve educational program to train, equip, and empower physicians to to be able to handle patient problems ethically and confidently, thereby avoiding unnecessary referrals; which in turn will reduce health costs considerably. But how can the health system geared up to train 250,000 graduate doctors?
Distance education[11] using all the andragogic[12] methods seem to be the ideal answer for this challenge. A well organized distance medical education program can be a transformative tool towards creating a national impact. We have residency training in family medicine, but the numbers one can train is too small and many doctors do not find it attractive to spend 3 years pursuing a “glamour-less degree.” The medical fraternity itself is ignorant of or is opposed to the concept of family medicine. In this scenario, how to popularize this most-needed specialty and rapidly build a pool of specialist doctors practicing and advocating family medicine discipline! Those doctors who are already settled in practice may be attracted to skill enhancement programs by delivering training at their doorsteps.!!
This motivated CMC Vellore, a premier institution for medical education in India, to start a the “refer less resolve more initiative” by offering “two year family medicine diploma course” by distance mode.
Course Components
This course gives a unique opportunity for private and government doctors, who have no access to post graduate education, to earn credit for a course equivalent to other specialties. Also, it is an opportunity for them to update their knowledge and skills right at their door steps. This “refer less, resolve more” initiative is designed to help them gain confidence and competency to handle most patients by themselves. Course components include 75 problem-based modules written in self-learning format. The students also submit assignments, logbooks, project-work, and attend three 10-day contact programs (total 30 days). They also have optional of electives in skills training and have to pass two theory as well as practical exams to earn the diploma.
Structured training is imparted at selected secondary level hospitals (10 centers across the country), where family medicine principles are practiced on a daily basis and also where holistic and ethical care can be demonstrated [Figure 1]. The learning is facilitated by national and international family physicians, who visit to these centers. The training program is supplemented by video-lectures by the expert faculty as well as live video-conferencing sessions [Figure 2] to clarify any doubts. These contact programs have become platforms for change as they include (1) Ethical Group Discussions, (2) Rational Prescribing Exercises, (3) Consultation skill role-plays, (4) Family Medicine Principles application exercises, (5) Inputs on global Family Medicine scenario through international faculty, (6) Practical demonstration of compassionate, cost-effective, high-quality care, and (7) Motivational sessions focused on attitude change. All these training modules have resulted in desirable changes in the practice of the participant doctors and have helped them develop a vision.
Figure 1.

Contact program - consultation skills development session in progress
Figure 2.
Video-conferencing session in progress
The Impact
The course impacted the GPs in a way that it helped them study and update themselves with latest knowledge in the field of clinical medicine, use simple algorithms to reach proper diagnoses, write rational prescriptions, introduce ethical principles into their practice, confidently handle patients whom they were referring earlier and shift gear from the “commercial” focus to the “care” focus. So, there was transformation was visible in three broad spheres: professional, ethics and values, and culture of patient care.
The course was first offered in 2006 and since then it has been accommodating 200 private practitioners each year. Encouraged by the impact of the course, the Government of Tamil Nadu (TNHSP) offered sponsorship for doctor posted at primary health centers—45 doctors per year. Following this, the National Rural Health Mission (NRHM) has shown keen interest in PHC (primary health center) doctors in eight backward north Indian states to be trained in family medicine and sponsors 150 doctors per year. The MGIMS (Mahatma Gandhi Institute for Medical Sciences, Sewagram) has signed a MOU to run this program in three northern states. So far, 942 private practitioners [Table 1] and 177 government doctors [Table 2] have been enrolled and at present and the total yearly enrollment has gone upto 500 per year. The various collaborations and contact centers are portrayed in Figures 3 and 4.
Table 1.
Number of general practitioners enrolled
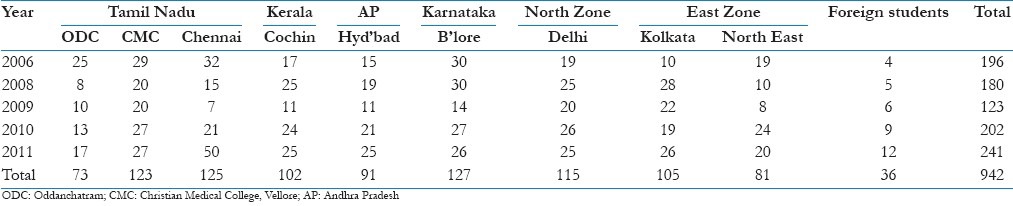
Table 2.
Number of government doctors enrolled
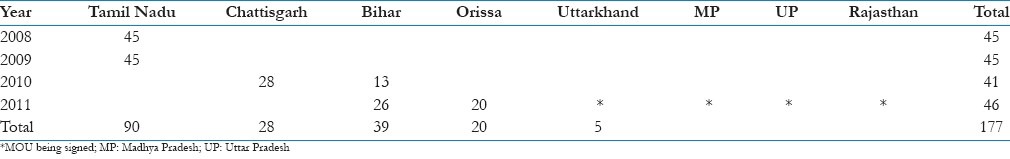
Figure 3.
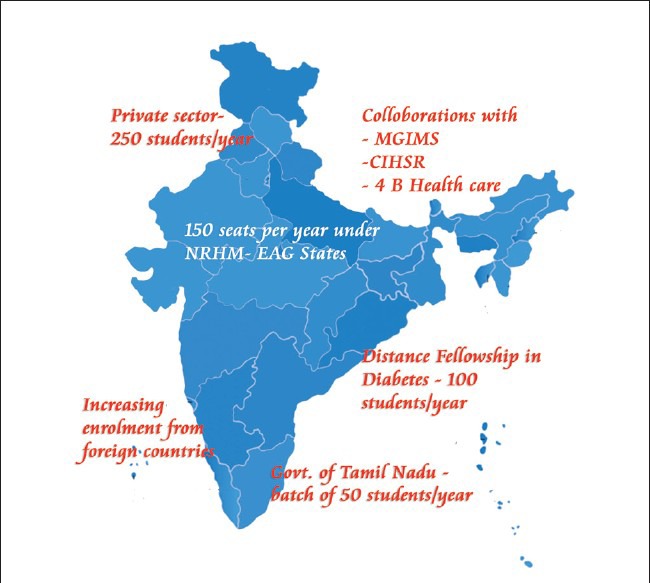
Present courses for doctors and collaborations
Figure 4.
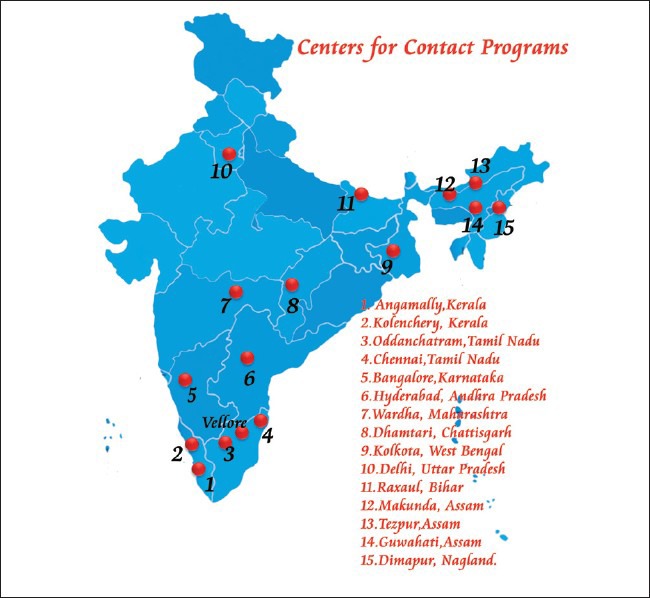
Centers for face-to-face sessions
Also, students from African countries and the middle east have started enrolling in the program. As the international students have visited India thrice during the contact programs, collaboration is being worked out with African countries to start a contact center in the respective countries. The program also has a resourceful and enthusiastic team of international faculty from the US, UK, and Australia who periodically visits and coordinates the contact programs at the various centers in the country. A masters level program in family medicine course which incorporates distance learning with 3 months of residential skills training is in the offing.
Other Areas of Focus
The other areas of focus are: E-learning, Primary care Research, Skills Lab, Student support, and CMEs.
Other initiatives to promote primary care
For young graduates
Integrated Post-Graduate Diploma in Family medicine (IPGDFM). – On the job training in more skill based family practice. Candidates are rigorously trained in family medicine principles and are expected to become strong advocates of the family medicine discipline. Number of enrollment is 70/year.
For family physicians
Distance Fellowship in Diabetes Management (DFID) – 100 students/year to facilitate holistic integrated cost-effective diabetes management at community level.
For medical students in clinical years
Supplementary education for medical students (SEMS) – 200 students/year, exposing students early-on to problem-based learning and family medicine principles.[13]
For health workers
Community Lay-leaders Health Training Certificate (CLHTC) Program – 200 students/year. Health worker training, trainees are be linked to family physicians to give community – based care.
Summary
Building a critical pool of trained family physicians in the country by raising standards of care, good primary care research and publications, uniting multiple individual efforts in the country under one umbrella; policy level changes like accreditation, incentives, and cadre positions, will all go a long way in elevating family medicine to the most-sought after specialty in the country. The path may be long and challenging….but we can make a difference…!
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Statistics MCI India. [Last accessed in Nov 2011]. Available from: http://www.mciindia.org/InformationDesk/MedicalCollegeHospitals/ListofCollegesTeachingMBBS.aspx .
- 2.World Health Organisation. 2007. [Last accessed on 2011 Nov 11]. p. 12. Available from: http://www.whoindia.org/LinkFiles/Human_Resources_Health_Workforce_in_India_-_Apr07.pdf .
- 3.Regulation of Medical Practitioners in India, Ashok Kumar, Central Bureau of Health Intelligence (CBHI) [Last accessed on 2011 Nov 11]. Available from: http://www.hum.au.dk/hsre/Docs/Presentations/4_Regulation-scope%20and%20limitations/1_Ashok_Kumar_Regulation.pdf .
- 4.RHS – Bulletin. 2010. [Last accessed on 2011 Nov 11]. http://www.mohfw.nic.in/BULLETIN%20 ON.htm .
- 5.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macinko J, Starfield B, Erinosho T. The impact of primary healthcare on population health in low- and middle-income countries. J Ambul Care Manage. 2009;32:150–71. doi: 10.1097/JAC.0b013e3181994221. [DOI] [PubMed] [Google Scholar]
- 7.Sandhya Srinivasan, Info Change News and Features, June. 2005. [Last accessed on Nov 2011]. Available from: http://www.infochangeindia.org/health/backgrounder/health-background-perspective.html .
- 8.Das A. Info Change News and Features. [Last accessed on June 2005]. Available from: http://www.infochangeindia.org/agenda/access-denied/nrhm-new-hope-for-the-rural-poor.html .
- 9.Shi L, Macinko J, Starfield B, Wulu J, Regan J, Politzer R. The relationship between primary care, income inequality, and mortality in US States, 1980-1995. J Am Board Fam Pract. 2003;16:412–22. doi: 10.3122/jabfm.16.5.412. [DOI] [PubMed] [Google Scholar]
- 10.Oxford: University Press; 1998. Starfield. Primary Care: Balancing Health Needs, Services, and Technology. [Google Scholar]
- 11.Keegan D. London: Routledge Falmer; 2001. Foundations of Distance Education. [Google Scholar]
- 12.Germany: Bamberg University; [Last accessed in 2003]. Reischmann, Jost: Why Andragogy? Available from: http://www.andragogy.net . [Google Scholar]
- 13.Zachariah P. Changing the Prescription, The Hindu. [Last accessed on Nov 2011]. Available from: http://www.thehindu.com/opinion/op-ed/article2609599.ece .


