Abstract
Patient: Male, 42
Final Diagnosis: Gluteal compartment syndrome • acute peripheral nauropathy
Symptoms: —
Medication: —
Clinical Procedure: —
Specialty: Critical Care Medicine
Objective:
Management of emergency care
Background:
Heroin addiction is common, with an estimated 3.7 million Americans reporting to have used it at some point in their lives. Complications of opiate overdose include infection, rhabdomyolysis, respiratory depression and central or peripheral nervous system neurological complications.
Conclusions:
We present a 42-year-old male admitted after heroin use with heroin-related peripheral nervous system complication preceded by an acute gluteal compartment syndrome and severe rhabdomyolysis.
Case Report:
Early diagnosis and surgical intervention of the compartment syndrome can lead to full recovery while any delay in management can be devastating and can lead to permanent disability. The presence of peripheral nervous system injuries may portend a poor prognosis and can also lead to long term disability. Careful neurological evaluation for signs and symptoms of peripheral nervous system injuries is of paramount importance, as these may be absent at presentation in patients with opioid overdose. There is a potential risk of delaying a necessary treatment like fasciotomy in these patients by falsely attributing clinical symptoms to a preexisting neuropathy. Early EMG and nerve conduction studies should be considered when the etiology of underlying neurological weakness is unclear.
MeSH Keywords: Addiction, Heroin, Rhabdomyolysis, Peripheral Nervous System, Disorder, Opioid-Related, electromyography
Background
Heroin use is a common finding in our population. Since the establishment of laws governing opioid prescription for non-cancer pain control in the 1990s, opioid use has increased substantially. Furthermore, standards of pain control set by Joint Commission on Accreditation of Healthcare Organizations (JCAHO) in 2000 paved way for further liberalization of their use. An estimated 3.7 million Americans have experimented with it at some point in their lives. Heroin, a morphine derived semisynthetic opioid, is metabolized after administration and binds rapidly to opioid receptors in the brain generating a surge of pleasurable sensation which leads to addiction. Americans, though less than 5% of total world population, consume up to 80% of world opioid supply [1]. In 2011, 620,000 (0.2%) of people aged 12 or older used heroin within the previous year. There were 178,000 first time users with a mean age of 22.2 years [2]. Abuse of these substances could lead to serious social and medical consequences with the younger generation particularly at higher risk. Complications of opiate overdose include infection, rhabdomyolysis, respiratory depression and various nervous system complications. We present a unique case of a heroin related peripheral nervous system complication preceded by an acute gluteal compartment syndrome.
Case Report
A 42-year-old male with a history of a prior gun-shot wound to the head, was brought by Emergency Medical Services after being found unresponsive at home by a family member with three empty syringes with needles next to the patient. As per family, last time they had spoken to patient was more than 24 hrs ago. He received dextrose and naloxone with no significant improvement in his neurological condition. Upon arrival to the emergency department his vital signs were stable, except for mild respiratory depression. He was drowsy with a Glasgow Coma Scale of 9/15, unable to provide any history. His pupils were constricted and he moved all extremities to noxious stimuli. No clinical signs of meningitis were appreciated. The remainder of his physical exam was unremarkable.
Initial laboratory tests demonstrated acute renal failure with a serum creatinine of 3.3 mg/dl and hyperkalemia. He was found to be in rhabdomyolysis with serum creatine kinase (CK) of 7721 unit/L, along with combined respiratory and anion gap metabolic acidosis (AGMA) with a pH of 7.19 (Table 1). Urine toxicology screen revealed opioids. Serum toxicology which only measures acetaminophen, alcohol and acetylsalicylic acids levels were undetectable. Abdominal ultrasound did not reveal any evidence of ureterolithiasis, nephrolithiasis or hydronephrosis.
Table 1.
Metabolic characteristics.
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Discharge | |
|---|---|---|---|---|---|---|
| Ph | 7.192 | 7.244 | 7.226 | 7.287 | 7.429 | – |
| Serum Creatinine | 3.3 | 6.4 | 7.4 | 7.1 | 0.3 | 1.2 |
| Serum HCO3 | 21.1 | 19.9 | 15.1 | 22.3 | 23.5 | 28 |
| Anion gap | 15 | 10 | 10 | 7 | 6 | 12 |
| Serum Potasium | 5.4 | 6.4 | 5.5 | 3.3 | 3.5 | 3.9 |
| Creatine kinase | 7721 | 114383 | 92566 | 45160 | 23546 | 139 |
| White blood count | 23 | 13.2 | 13.1 | 12.7 | 9.1 | 7.4 |
| AST/ALT | 588/1117 | – | – | 321/519 | 79/32 | – |
Over the next 24–36 hours his mental status improved and on further interview, he admitted to cannabinoid and intravenous heroin use but denied ingesting other toxic substances or prescription medications. Additionally, he complained of left thigh pain. Exam revealed a firm but non-tender left thigh region with intact peripheral pulses. He denied injecting in his thigh stating that he only injected in his forearm veins. Computed tomography (CT) scan of the left lower extremity revealed evidence of fascia edema of the lateral aspect of the vastus lateralis (Figure 1). The patient remained in acute renal failure with persistent hyperkalemia and AGMA. CK levels increased to 114,383 unit/L on day 2. Despite aggressive hydration, renal function deteriorated and patient gradually became anuric. Hemodialysis was initiated on day 3. Patient started reporting pain and swelling of the left thigh along with new bilateral lower extremity weakness. Physical exam demonstrated decreasing distal pulses on the left side along with tender and firm thigh with minimal voluntary movement of both lower extremities. Detailed neurological examination of the lower extremities revealed decreased bilateral motor strength (1/5) with allodynia. Patellar hyperreflexia was noted but the Achilles reflex was absent. No clonus was present and plantar responses were also absent. He had normal motor and sensory function of upper extremities except for mild biceps hyperreflexia. Cranial nerves were intact and there were no bowel or bladder symptoms. Given the clinical picture of a left gluteal compartment syndrome threatening the left lower extremity, he underwent emergent surgical fasciotomy and left gluteal compartment release. Intra-operatively, he was found to have necrotic and edematous gluteus maximus and medius muscles. Post operatively patient continued to complain of bilateral lower extremity weakness. A CT scan of the head was negative for acute stroke or bleed and CT scans of the cervical, thoracic and lumbar spine were also unremarkable. Connective tissue work up was inconclusive. Electromyography (EMG) and nerve conduction study performed which demonstrated severe axonal neuropathy of the bilateral lower extremity motor and sensory nerves, a finding most consistent with the axonal form of Guillain-Barré syndrome (Tables 2 and 3). Over the next week his renal function returned to normal and dialysis was discontinued. He was subsequently discharged to short term rehabilitation due to persistent lower extremity weakness.
Figure 1.
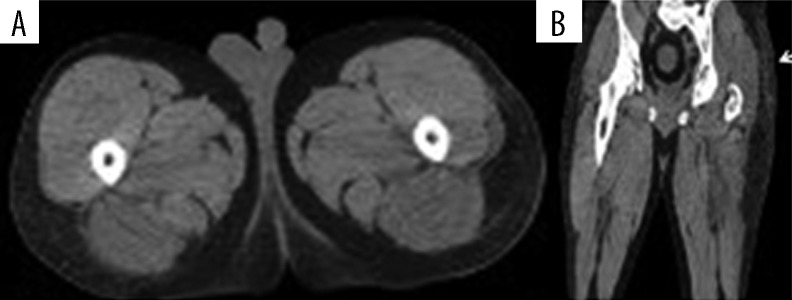
(A, B) CT of lower extremity without contrast showing flank soft tissue edema with prominence of the gluteal muscles on the left. There is apparent fascia edema of the lateral aspect of the vastus lateralis muscle along with edema on the lateral aspect of semitendinosus muscle bilaterally.
Table 2.
Electromyography.
| Side | Muscle | Nerve | Root | Ins act | Fibs | PSW | Amp | Dur | Poly | Recruitment | Int pat |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Right | Anterior tibialis | Peroneal | L4-5 | Normal | Normal | Normal | Normal | Normal | 0 | Reduced | 25% |
| Right | Medial gastrocnemius | Tibial | S1-2 | Normal | Normal | +1 | Normal | Normal | 0 | Reduced | 25% |
| Right | External hallucis longus | Peroneal | L5-S2 | Normal | Normal | Normal | Normal | Normal | 0 | Reduced | 25% |
| Right | Vastus medialis | Femoral | L2-4 | Normal | Normal | +1 | Normal | Normal | 0 | Reduced | 25% |
EMG reveals normal muscle membrane potential (as indicated by normal insertional activity {Ins Act}, fibrillations {Fibs} and positive sharp waves {Psw}) and intact action potential (as indicated by normal amplitude {Amp}, duration {Dur}, Polyphasic activity {Poly}). Study also reveals significantly reduced nervous system output (as indicate by recruitment {Recrt}, interference pattern {Int Pat}. Note: only 25% of the nervous system output was reaching the mentioned muscle.
Table 3.
Nerve conduction study reveals normal onset latency (which is a function of neuronal myelination) with significantly reduced amplitude in the lower extremity nerves suggesting axonal degeneration or death in these nerves, a finding suggestive of axonal form of Guillain Barre syndrome. Please note that these changes were not seen in the upper extremity nerves.
| Motor nerves | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NR | Onset (ms) | Norm onset (ms) | O-P amp (mV) | Norm amp (mV) | Neg dur (ms) | Segment name | Delta-O (ms) | Dist (cm) | Vel (m/s) | Norm vel (m/s) |
| Right peroneal (EDB) | ||||||||||
| Ankle | 4.92 | <5.5 | 0.08 | >2.5 | 5.70 | B fib-ankle | 6.25 | 29 | 46.40 | >40.0 |
| B Fib | 11.17 | 0.12 | 5.55 | Poplt-B fib | 1.09 | 6 | 55.05 | >40.0 | ||
| Poplt | 12.27 | 0.38 | 5.39 | |||||||
| Right tibial (AHB) | ||||||||||
| Ankle NR | <6.0 | >3.0 | Knee-ankle | −2.11 | >41.0 | |||||
| Knee | 14.30 | 0.05 | 3.91 | |||||||
| Left peroneal (EDB) | ||||||||||
| Ankle NR | <5.5 | >2.5 | ||||||||
| Left tibial (AHB) | ||||||||||
| Ankle | 5.70 | <6.0 | 0.83 | >3.0 | 3.13 | Knee-ankle | 9.06 | 42 | 46.36 | >41.0 |
| Knee | 14.77 | 0.45 | 4.92 | |||||||
| Left median (abd poll brev) | ||||||||||
| Wrist | 3.05 | <4.2 | 11.28 | >5.0 | 5.31 | Elbow-wrist | 3.52 | 19 | 53.98 | >50.0 |
| Elbow | 6.56 | 10.88 | 5.63 | |||||||
| Left ulnar (abd dig min) | ||||||||||
| Wrist | 2.89 | <4.2 | 11.90 | >3.0 | 6.09 | B elbow-wrist | 3.13 | 21 | 67.09 | >53.0 |
| B elbow | 6.02 | 12.79 | 6.25 | A elbow- B elbow | 1.17 | 8 | 68.38 | >53.0 | ||
| A elbow | 7.19 | 13.02 | 6.02 | Axilla- A elbow | 1.41 | 10 | 70.92 | |||
| Axilla | 8.59 | 13.22 | 6.09 | |||||||
Discussion
Immediate effects of opioid use may include mental depression, depressed cardiac and respiratory function, and skin flushing, dry mouth and nausea. Other more sub acute and less common adverse effects include peripheral nervous system injury, rhabdomyolysis which may lead to renal failure, and compartment syndrome [3] like the one seen in our patient. Rhabdomyolysis may be more severe when precipitated by drug overdoses compared to other etiologies. While pathogenesis in these patients is unclear, potential mechanisms for muscle injury include postural muscle compression when comatose, or an allergic or toxic reaction to heroin or its adulterants [4]. In our patient, the empty syringes were not brought up to the laboratory for analysis to look for other potential toxic substances not measured in urine or serum toxicology. Acute compartment syndrome is a surgical emergency which often results from the increased edema of the damaged tissues following crush or reperfusion injury. Compartment syndrome of the gluteal musculature is a rare condition which can be seen in patients with alcohol or illicit drug use as a consequence of prolonged immobilization in prone, lateral or sitting positions [5]. Early diagnosis can be problematic in this group as these patients are frequently unable to communicate their symptoms due to altered mental state related to substance abuse. Nonetheless early identification remains critical as a delay in diagnosis by only a few hours can be devastating for the patient and can lead to permanent disability. The diagnosis of compartment syndrome is mainly clinical and based on repeated physical exams. Measuring compartment pressures (CP) may be helpful, but a diagnostic pressure threshold is unknown. Normal intra-compartmental pressure is 0–8 mmHg in adults and symptoms like pain and paresthesias appear when the pressures elevate to a range of >20–30 mmHg [6]. In our patient, CP was not measured as he underwent emergent decompression, when measured, the CP threshold for fasciotomy varies from 30 to 50 mmHg [6–8]. There has been some evidence that irreversible tissue damage from ischemia is directly related to difference between diastolic blood pressure and CP rather than absolute CP [9,10]. There have been no studies in gluteal compartment syndrome and consequently there is no consensus in the literature about a specific CP pressure or differential pressure in this particular condition as an indication for surgery. Imaging studies like ultra-sonogram, Doppler ultrasound, CT and magnetic resonance imaging can aid in diagnosis. Newer diagnostic modalities include infrared spectroscopy, ultra-filtration catheterization and radiofrequency identification implants have been established but their use is limited.
Opioids can affect both the central and peripheral nervous systems. Central nervous system complications of heroin include seizures, hypoxic brain damage, stroke, heroin leukoencephalopathy and paraplegia. Heroin related peripheral nervous system injuries, which could be either traumatic or non-traumatic, have been reported rarely in literature. Traumatic complications occur as a result of pressure on dependent areas during periods of prolonged unresponsiveness after drug use and manifest as compressive neuropathies [11, 12]. Non traumatic peripheral nervous system manifestations are usually associated with rhabdomyolysis and include polyradiculopathy, plexitis, Guillain-Barre’ syndrome (GBS), and mononeuropathy [13]. Etiology of these complications is unclear, although few case reports of heroin-related peripheral neuropathies showed response to steroids, which suggested an immune mechanism [14]. A more recent case series proposed direct toxic injury as well as nerve or muscle compression as the cause of these injuries [15]. Opioid-induced GBS is extremely rare and is diagnosed by EMG demonstrating sensory-motor axonal neuropathy. There is no specific treatment for this condition and prognosis is poor in most cases. Most patients remain with significant disability on follow-up.
Conclusions
Our case highlights several rare yet potentially devastating complications of heroin overdose; a gluteal compartment syndrome with severe rhabdomyolysis along with sensory-motor axonal neuropathy. While early diagnosis and surgical intervention of a compartment syndrome can lead to full recovery, any delay in diagnosis can be devastating for the patient and can cause permanent disability. Peripheral nervous system injuries may portend a poor prognosis and can also lead to long term disability. These patients require careful and serial neurological evaluation for signs and symptoms of compartment syndrome and peripheral nervous system injuries as these may be absent at presentation in a patient with opioid overdose. Early EMG/ nerve conduction studies are recommended when the etiology of underlying neurological weakness is unclear. Failure to identify these patients carry the potential risk of delaying a necessary and limb saving treatment such us fasciotomy secondary to opioid overdose or falsely attributing clinical symptoms to a preexisting or developing neuropathy.
Abbreviations:
- BP
blood pressure
- CK
creatine kinase
- CP
compartment pressure
- CT
computed tomography
- EMG
electromyography
- GBS
Guillain-Barre’ syndrome
Footnotes
Author disclosure
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of the manuscript.
Informed consent was obtained from the patient prior to writing of this case report.
References:
- 1.Wang J, Christo PJ. The influence of prescription monitoring programs on chronic pain management. Pain Physician. 2009;12(3):507–15. [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration, Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 3.Radovanović MR, Milovanović DR, Ignjatović-Ristić D, Radovanović MS. Heroin addict with gangrene of the extremities, rhabdomyolysis and severe hyperkalemia. Vojnosanit Pregl. 2012;69(10):908–12. [PubMed] [Google Scholar]
- 4.Kumar R, West DM, Jingree M, Laurence AS. Unusual consequences of heroin overdose: rhabdomyolysis, acute renal failure, paraplegia and hyper-calcaemia. Br J Anaesth. 1999;83(3):496–98. doi: 10.1093/bja/83.3.496. [DOI] [PubMed] [Google Scholar]
- 5.Yoshioka H. Gluteal compartment syndrome. A report of 4 cases. Acta Orthop Scand. 1992;63(3):347–49. doi: 10.3109/17453679209154800. [DOI] [PubMed] [Google Scholar]
- 6.Mubarak SJ, Owen CA, Hargens AR, et al. Acute compartment syndromes: diagnosis and treatment with the aid of the wick catheter. J Bone Joint Surg Am. 1978;60(8):1091–95. [PubMed] [Google Scholar]
- 7.Allen MJ, Stirling AJ, Crawshaw CV, Barnes MR. Intracompartmental pressure monitoring of leg injuries. An aid to management. J Bone Joint Surg Br. 1985;67(1):53–57. doi: 10.1302/0301-620X.67B1.3968144. [DOI] [PubMed] [Google Scholar]
- 8.Taylor RM, Sullivan MP, Mehta S. Acute compartment syndrome: obtaining diagnosis, providing treatment, and minimizing medico legal risk. Curr Rev Musculoskelet Med. 2012;5(3):206–13. doi: 10.1007/s12178-012-9126-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heckman MM, Whitesides TE, Jr, Grewe SR, et al. Histologic determination of the ischemic threshold of muscle in the canine compartment syndrome model. J Orthop Trauma. 1993;7:199–210. doi: 10.1097/00005131-199306000-00001. [DOI] [PubMed] [Google Scholar]
- 10.McQueen MM, Court-Brown CM. Compartment monitoring in tibial fractures. The pressure threshold for decompression. J Bone Joint Surg Br. 1996;78(1):99–104. [PubMed] [Google Scholar]
- 11.Riggs JE, Schochet SS, Jr, Hogg JP. Focal rhabdomyolysis and brachial plexopathy: an association with heroin and chronic ethanol use. Mil Med. 1999;164(3):228–29. [PubMed] [Google Scholar]
- 12.Sheehan TP, Jabre JF. Dorsal ulnar sensory neuropathy in a heroin abuser. Muscle Nerve. 1995;18(5):559. [PubMed] [Google Scholar]
- 13.Smith WR, Wilson AF. Guillan-Barré syndrome in heroin addiction. JAMA. 1975;231(13):1367–68. [PubMed] [Google Scholar]
- 14.Warner-Smith M, Darke S, Day C. Morbidity associated with non-fatal heroin overdose. Addiction. 2002;97(8):963–67. doi: 10.1046/j.1360-0443.2002.00132.x. [DOI] [PubMed] [Google Scholar]
- 15.Kaku DA, So YT. Acute femoral neuropathy and iliopsoas infarction in intravenous drug abusers. Neurology. 1990;40(8):1317–18. doi: 10.1212/wnl.40.8.1317. [DOI] [PubMed] [Google Scholar]


