Abstract
Peptide hormones are released from the gastrointestinal tract in response to nutrients and communicate information regarding the current state of energy balance to the brain. These hormones regulate appetite, energy expenditure and glucose homeostasis. They can act either via the circulation at target peripheral tissues, by activation of the vagus nerve or by acting on key brain regions implicated in energy homeostasis such as the hypothalamus and brainstem. This review gives an overview of the main gut hormones implicated in the regulation of food intake and how some of these are being targeted to develop anti obesity treatments.
Keywords: peptide YY (PYY), glucagon-like peptide-1 (GLP-1), glucagon, ghrelin, bariatric surgery, obesity
Introduction
Obesity is one of the greatest health care challenges of our time. Currently there are estimated to be 2 billion adults who are overweight worldwide (body mass index 25–30 kg/m2) and a further 500 million are obese (BMI greater than 30 kg/m2). Being overweight or obese carries an increased risk type 2 diabetes, ischaemic heart disease, stroke and cancer, and carries an increased risk of both all cause, and cause-specific mortality (1,2). This has prompted a concerted effort to identify effective novel treatments for obesity. The role of peripheral hormones and the gut/brain axis in the regulation of appetite has become a hot topic in recent years, owing to the growing global obesity crisis. Of particular interest has been the potential of these peripheral signals to provide novel targets for developing anti-obesity therapies. The focus of this review is to provide a synopsis of the gut-brain cross talk involved in the regulation of food intake.
Neuroendocrine control of appetite
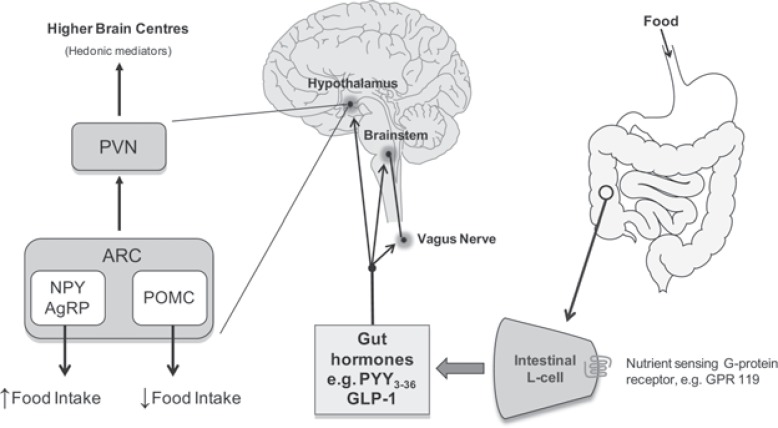
The hypothalamus and the brainstem are the main central nervous system regions responsible for the regulation of energy homeostasis. Although it is important to remember these regions are not solely responsible. Both the hypothalamus and the brainstem receive peripheral neural and hormonal signals that relay information regarding energy availability, both acutely i.e. nutritional state and long term availability i.e. adiposity (3). Neural afferents and hormonal signals from the periphery are integrated with higher brain centre signals (e.g. relaying reward drive and mood) to regulate appetite and control energy expenditure (4) (Figure 1).
Figure 1.
Gut-brain axis: regulation of food intake.
Nutrients created by the digestion of food are proposed to activate G-protein coupled receptors on the luminal side of enetroendocrine cells e.g. the L-cell. This stimulates the release of gut hormones which may influence food intake at three sites: the vagus nerve, brainstem and hypothalamus. Within the arcuate nucleus of the hypothalamus two neuronal populations are thought to be critical conduits through which peripheral signals are integrated to alter the drive to eat, the orexigenic NPY/AgRP neurons and the anorexigenic POMC neurons. Further connections between hypothalamic nuclei and higher brain centres may exist which control the hedonic aspects of food ingestion.
ARC - arcuate nucleus; AgRP - agouti related peptide; GLP-1 - glucagon like peptide-1; NPY - neuropeptide Y; POMC – propiomelanocortin; PVN - paraventricular nucleus; PYY - peptide YY.
The arcuate nucleus (ARC) of the hypothalamus is believed to play a crucial role in the regulation of food intake and energy homeostasis. The ARC contains two populations of neurons with opposing effects on food intake (5). Orexigenic neurons (i.e. those stimulating appetite) express neuropeptide Y (NPY) and Agouti-related protein (AgRP) (6–8). Whilst anorexigenic neurons (i.e. those inhibiting appetite) in the ARC express alpha-melanocyte-stimulating hormone (alpha-MSH) derived from pro-opiomelanocortin (POMC), and cocaine-and amphetamine-regulated transcript (CART) (9).
The ARC is adjacent to the median eminence, a ‘circumventricular organ’ with fenestrated capillaries and hence an incomplete blood-brain barrier (10). Circulating hormones are able to pass across the median eminence and influence the activity of the ARC neurons directly. Gut hormones are released from the gastrointestinal tract on a meal to meal basis and signal short term nutrient availability to the ARC. Other circulating factors such as insulin and leptin (a circulating peptide released from adipose tissue) relay information about long-term energy stores and adiposity (11). Thus the ARC has been described as a conduit through which the body can balance its energy requirements to maintain weight.
Additionally short term availability of nutrients is signalled by gastrointestinal vagal afferents. Following a meal the vagus is activated by both mechanoreceptors and chemoreceptors. The resultant neural signals converge in the nucleus of the tractus solitarius (NTS) within the brainstem. These signal are then fed forward Neuronal from the NTS to the hypothalamus. Circulating factors such as gut hormones are also thought to act at the NTS, which like the ARC is adjacent to a circumventricular organ, the ‘area postrema’ (AP). For example, ablation of both the AP and another circumventricular organ, the subfornical organ (SFO), has been shown to delay the anorectic action of the gut hormone peptide tyrosine tyrosine (PYY) (12). Gut hormones also alter the activity of the ascending vagal pathways from the gut to the brainstem (13).
Hence, the hypothalamic ARC orexigenic and anorexigenic neurons are influenced by numerous neural and hormonal inputs. These ARC neurons in turn project to a number of extra-hypothalamic and intra-hypothalamic regions, including in particular the hypothalamic paraventricular nucleus (PVN), where some of the important efferent pathways regulating energy expenditure arise.
Enteroendocrine cells of the gastrointestinal tract
There are at least 15 different types of enteroendocrine cells diffusely distributed throughout the gastrointestinal epithelium (14). These cells produce and release a variety of hormones and signalling molecules, which together constitute the largest endocrine organ in the body (14,15). Chemosensing of gut luminal contents by the enteroendocrine GI cells plays a critical role in the control of functions such as digestion, pancreatic secretion, food intake, and metabolic regulation. Evidence that endocrine cells can directly sense luminal contents has been demonstrated in PYY and glucagon like peptide −1 (GLP-1) expressing L cells. Both human and rodent L cells express receptors previously identified in the oral epithelium for detecting sweet (T1R2 and T1R3) and bitter sensation (T2R), as well as amino acids (T1R1 and T1R3) (16,17). Additionally, the gustducin G protein which is associated with these taste receptors has been identified in L cells (16,17). Activation of these receptors is thought to lead to increased intracellular calcium and release of gastrointestinal peptides from enteroendocrine cells (17). The presence of the sweet taste receptor subunit T1R3 and gustducin may also underlie a luminal glucose sensing mechanism, since activation of these receptors mediates the postprandial release of GLP-1 from intestinal L cells (16).
Fatty acids derived from digestion of dietary fats appear to be sensed via separate mechanisms. The short-chain fatty acid receptors GPR43 and GPR41 are expressed in PYY-containing enteroendocrine L cells (18,19). Short chain fatty acids have been shown to increase both PYY and GLP-1 secretion in rats when delivered directly into the colon (20,21). GPR119 is another G protein coupled receptor found in intestinal endocrine cells as well as pancreatic beta cells (22). Administration of oleoylethanolamide (OEA), an endogenous long chain fatty acid derivative, and other GPR119 agonists increases GLP-1 secretion, both in vitro and in vivo in rodents (22,23).
The enteroendocrine L cells therefore have the capacity to integrate complex nutrient sensing in the gut and to respond appropriately by releasing gut hormones. In addition to chemical stimulation, the endocrine cells of the gut also respond to neural and physical stimulation of the cell by releasing peptide containing granules at the basolateral side of the cell. These peptides can have an endocrine role, a local paracrine role, and/or activate receptors present on nerves innervating the GI mucosa (24).
Gut hormones regulating food intake
The gastrointestinal tract releases more than 20 different regulatory peptide hormones that influence a number of physiological processes (25). The release of gut hormones such as PYY, GLP-1, and oxyntomodulin (OXM) is stimulated by distension of the stomach, production of nutrients from the digestion of food, and by neuronal signals (26,27).
Gut hormones are believed to contribute to the short-term feelings of satiety and hunger (28). These peptides are thought to reduce food intake by decreasing hypothalamic orexigenic signalling and increasing anorectic signalling (13,29). These peptides also mediate inhibitory feedback mechanisms on intestinal transit, contributing to prolonged gastric distension, and increased satiety between meals (30,31). These combined CNS effects and ‘intestinal brake’ mechanisms facilitate the control of food intake and postprandial transit through the gastrointestinal tract and thereby the immediate availability of energy. Below the focus of the review will concentrate on 5 of the most studied gut hormones which have been shown to control food intake and body weight and which are being actively pursued as anti-obesity targets.
Peptide tyrosine tyrosine (PYY)
PYY belongs to the ‘PP-fold’ family of proteins like NPY and pancreatic polypeptide (PP). These peptides are 36 amino acids in length and share a common tertiary structural motif known as the PP-fold. C-terminal amidation of these proteins is a necessary requirement for biological activity. PYY exists endogenously in two forms: PYY1-36 and PYY3-36(32). The enzymatic cleavage of secreted PYY1-36 at the amino terminal by the cell surface enzyme dipeptidyl peptidase IV (DPP-IV) gives rise to PYY3-36(33), which is the predominant form of circulating PYY immunoreactivity. PYY1-36 and PYY3-36 exert their effects through the neuropeptide Y family of receptors (34). PYY1-36 binds with similar affinity to all of the Y receptors, however PYY3-36 is a selective high affinity agonist at the Y2 receptor subtype (Y2R) (35). The Y2R is thought to be the receptor responsible for mediating the reduction of food intake by PYY. It is an auto-inhibitory pre-synaptic receptor found on NPY neurons within the ARC (36), and deficiency of the Y2R abolishes the anorectic effects of PYY (29). Furthermore, the anorectic effects of PYY3-36 are attenuated by Y2R antagonists (37). PYY3-36 is therefore thought to reduce food intake through activation of the Y2R.
Low levels of PYY are detected in enteroendocrine cells in the stomach, and levels increase distally along the small and large intestine, reaching their highest levels in cells in the colon and rectum (26). Endogenous circulating concentrations of PYY are lowest in the fasting state, and rise post-prandially in proportion to caloric intake (26). Plasma levels of PYY rise within 30 minutes of a meal, and in humans, circulating levels plateau at 1–2 hours post-prandially, remaining elevated for up to 6 hours (38). Protein rich meals cause the greatest increase in PYY levels compared to other macronutrients (39,40). Peripheral administration of PYY3-36 reduces food intake and weight gain in rodents (29,41–43). Intravenous administration of PYY inhibits food intake in humans and unlike leptin is equally effective in normal and obese subjects (44).
The anorectic effects of PYY3-36 appear to be mediated centrally via the ARC, as peripheral administration of PYY3-36 increases c-fos expression in this hypothalamic nucleus (29). Peripheral administration has been reported to decrease expression and release of NPY whilst activating POMC neurons (29). However, others have reported PYY3-36 inhibits POMC neurons via postsynaptic Y2R (45). Moreover, POMC knockout mice maintain their acute anorectic response to peripherally administered PYY3-36, suggesting that POMC is not critical to the inhibitory effects of PYY3-36 on feeding (46).
A vagal brainstem mediated pathway may also be involved since PYY is expressed by the neurones of the myenteric plexus and the Y2R receptor is expressed by the vagus nerve (47). Furthermore the anorectic effect of PYY3-36 on both food intake (47,48), and ARC activation of feeding neurons, are abolished following bilateral sub-diaphragmatic total truncal vagotomy or following transection of the brainstem–hypothalamic pathway in rodents (48).
Interestingly, it has recently been shown that acute effects of gastrointestinal bypass surgery on body weight are lost in PyyKO mice (49), and that wild-type mice losing weight after gastrointestinal bypass surgery exhibit increased colonic Pyy expression and circulating fasting PYY levels (49). Suggesting PYY plays a key role in mediating the early weight loss that occurs following gastrointestinal bypass surgery.
The effects of PYY3-36 on satiety and central control of appetite are clear. Most are mediated via anorectic neuronal populations in the ARC, but vagal/brainstem-mediated pathways and peripheral effects of PYY on gastric emptying and intestinal motility may also play a part. High plasma concentrations of PYY result in nausea, but the importance of PYY3-36 at physiological levels in the regulation of energy intake make it a prime focus for new obesity therapies, targeted either at PYY itself, or against the Y2 receptor.
Glucagon-like peptide-1 (GLP-1)
GLP-1 is a 30 amino acid peptide produced from the cleavage of preproglucagon (50). The two bio-active forms of GLP-1, GLP-17-37 and GLP-17-36 amide, are released into the circulation from L cells of the gastrointestinal tract in response to an oral glucose load (51). Physiologically, GLP-1 is an important in-cretin, augmenting glucose-dependent insulin release (52). In addition, GLP-1 inhibits the secretion of glucagon, thereby inhibiting endogenous glucose production (53). The net effect is to reduce blood glucose following a meal. GLP-1 also delays gastric emptying (54), and increases satiety (55,56).
Like PYY, GLP-1 has been shown to act centrally at hypothalamic nuclei known to be implicated in the control of appetite including the ARC, PVN and supraoptic nucleus (57). Both acute peripheral and central administration of GLP-1 reduce food intake in rats (58,59) and chronic administration of GLP-1 reduces weight gain (55). The intravenous administration of GLP-1 to normal and obese humans decreases food intake in a dose dependent manner (60) as well as reducing gastric emptying (61,62). These effects are thought to be mediated through vagal and brainstem pathways since peripheral administration of GLP-1 activates neurons within the brainstem in rats (63). Furthermore, this increase in neuronal activity, and the anorectic effects of GLP-1, are abolished following vagotomy in rodents (48,63). More recently, functional magnetic resonance imaging (fMRI) has confirmed the activation of the VMH and PVN following peripheral administration of GLP-1 (64).
GLP-1 is rapidly degraded in the circulation by DPP-IV, making native GLP-1 unsuitable for therapeutic use. Longer acting GLP-1 mimetics have been developed (65). Exendin-4 is a naturally occurring GLP-1 mimetic isolated from the venom of Heloderma suspectum, a lizard native to several southwestern American states (66). A truncated form of this peptide, exendin 9–39, acts as a competitive antagonist at the GLP-1 receptor. Acute intracerebroventricular administration of exendin 9–39 increases food intake and chronic administration increases body weight in rats (55,59). Suggesting endogenous peripheral GLP-1 may physiologically reduce appetite and food intake. However, GLP-1 receptor knockout mice do not have altered food intake or body weight (67). This may be because developmental changes compensate for the lack of GLP-1 signalling, or may reflect that GLP-1 has a more important physiological role in controlling blood glucose than in regulating food intake.
The discovery of exendin-4 has led to the development of a synthetic version, exenatide. Exenatide has a much longer in vivo half-life than native GLP-1, stimulates insulin release, suppresses glucagon and lowers blood glucose. It is the first incretin mimetic approved for the treatment of type 2 diabetes (68). Exenatide has also been shown to reduce body weight in treated diabetics in phase III clinical trials (69–71). The weight loss associated with exenatide is considered a significant advantage as many anti-diabetic treatments are commonly associated with weight gain. Nausea is a relatively common side effect of Exenatide treatment. However, it does not seem to be intrinsically linked to the effects on appetite (3). Whilst GLP-1 has been developed as a treatment for diabetes due to its incretin properties, the observed effects of GLP-1 on satiety and weight loss are a valuable secondary effect. Indeed recent data suggests liraglutide may be useful for the treatment of obesity, causing sustained weight loss over 2 years but with a 50% rate of nausea and vomiting in the 3.0 mg/day group in the first year (72). The newest long acting analogues of GLP-1, exenatide-LAR (Amylin Pharmaceuticals, FDA approved January 2012), taspoglutide (Ipsen and Roche) and Albiglutide (GlaxoSmithKline), have been shown to effectively control glucose and to reduce weight. These agents allow for less-frequent dosing schedules, improved glycemic control throughout the day, and improved treatment satisfaction compared to some available agents (73). It remains to be seen whether these drugs perform well enough in specific weight loss paradigms such that they could be used as anti-obesity agents.
Oxyntomodulin (OXM)
OXM, like GLP-1, is also a product of the preproglucagon precursor molecule. It is a 37 amino acid peptide released post-prandially from L cells in proportion to caloric intake (27). OXM delays gastric emptying and reduces gastric acid secretion (74), and has been shown acutely to decrease food intake and in the longer term to decrease weight gain in rodents (75,76). In addition, chronic administration of OXM produces greater weight loss compared to pair-fed controls, suggesting an increase in energy expenditure may also help to reduce body weight (77). OXM has been shown to reduce food intake in normal weight human volunteers when administered intravenously or subcutaneously (78). Given preprandially to obese subjects it reduces both food intake and body weight (79). As in rats, there is evidence that OXM may also increase energy expenditure in humans (80).
Although OXM has some agonist activity at the glucagon receptor, there is evidence that its anorectic effect is predominantly mediated via the GLP-1 receptor (75,81). The anorectic effects of OXM are abolished in GLP-1 receptor knockout mice (81) and in the presence of the GLP-1 receptor antagonist exendin 9–39 (76). OXM has a 50-fold lower affinity for the GLP-1 receptor than GLP-1 itself, but despite this, it reduces food intake with similar potency (75). Furthermore, although the administration of exendin 9–39 directly into the ARC blocks the anorectic effects of OXM, it does not block those of GLP-1 (76). Therefore, it is possible that OXM may act via an as yet unidentified receptor. Studies using manganese-enhanced magnetic resonance imaging MRI (MEMRI) has shown that intraperitoneal administration of OXM produces a distinct pattern of neuronal activation compared to GLP-1 (82), implying that these two hormones act via different hypothalamic pathways.
Glucagon
Glucagon is a 29 amino acid peptide secreted from the α-cells of the pancreatic islets of Langerhans. It is a further product of preproglucagon cleavage alongside OXM and GLP-1. Glucagon is released into the portal vein in fasted states and also in response to exercise, and acts on the liver to promote hepatic glycogenolysis and gluconeogenesis and maintain glycaemic balance (83–86).
Glucagon mediates its effects via the glucagon receptor, a 7-transmembrane G-protein coupled receptor which has a wide tissue distribution. It is expressed in the gut, adrenal glands, brain, heart, pancreas, spleen and in adipocytes, but is predominantly found in the liver and kidney (87).
As a potential treatment for obesity, glucagon has been shown to increase energy expenditure in rats, and also in humans during insulin deficiency (88). It also significantly reduces food intake, with a subjective reduction of appetite in man (89). Infusion of glucagon into the portal vein but not the inferior vena cava causes a reduction in meal size in rats (90).
Glucagon presents an interesting prospect in the treatment of obesity due to its effect on increasing energy expenditure, and increasing satiety. It has been demonstrated that the potentially unfavourable effect on glucose tolerance due to glucagon’s actions on hepatic glycogenolysis and gluconeogenesis is effectively counteracted by dual agonism at the glucagon and GLP-1 receptors (91,92). The data from these studies demonstrated highly effective weight loss in diet-induced obese mice whilst avoiding the hyperglycaemia that might be expected from agonism at the glucagon receptor.
Ghrelin
Ghrelin is a 28-amino acid acylated peptide secreted from the stomach. It was originally identified as an endogenous ligand for the ‘growth hormone secretagogue’ receptor (GHS-R) and is a growth-hormone-releasing peptide (93).
Ghrelin is the only orexigenic gut hormone (94), causing an increase in food intake and weight gain in rodents following both peripheral and central administration (95–97). Intravenous administration of ghrelin has also been shown to stimulate gastric acid secretion and motility in rats (98). In normal subjects, ghrelin levels are highest in the fasted state (99), and levels are chronically higher in people with weight loss due to anorexia nervosa or dietary reduction (100–102). In contrast to other gut hormones, plasma ghrelin levels decrease after meals (100,103) and are low in obese subjects (102). Ghrelin concentrations are also reduced after gastric bypass surgery, and this may contribute to weight loss in such patients (101).
Ghrelin receptors are found in the ARC of the hypothalamus suggesting a central mode of action. Consistent with this c-fos expression is increased in the ARC after peripheral administration of ghrelin (104) and ablation of the ARC blocks ghrelin induced food intake (105). When given centrally, ghrelin also stimulates c-fos expression in other nuclei known to be involved in appetite control including the PVN, dorsomedial nucleus, and lateral hypothalamus as well as in the AP and NTS in the brainstem (95). Ghrelin and its receptor are both expressed in vagal afferents in mice (106), and blockade of the gastric vagal afferent has been shown to abolish ghrelin-induced feeding, growth hormone secretion, and activation of NPY-producing and growth hormone-releasing hormone producing neurons in rats suggesting an additional mode of action (107).
Diet induced obesity is associated with a blunting of ghrelin’s orexigenic effect. There has therefore been recent interest in the interaction between the ghrelin system and macronutrients. High fat feeding has been shown to render NPY/AgRP neurones relatively ghrelin resistant (108), and diets high in fat have been shown to directly inhibit the hyperphagic effect of ghrelin (109,110). These data have significant implications for developing anti-obesity treatments targeting the ghrelin system and suggest success of these approaches could depend on the fat content of the diet the patient consumes. More recently, ghrelin has been shown to engage neurons in the ventral tegmental area of the brain and may provide a link between the gut and neuronal control of stress-induced eating of ‘comfort foods’ (111).
Other gut peptides
A number of other gut-derived peptides have been shown to reduce food intake. However, the physiological role of these peptides in the regulation of food intake and energy homeostasis remains unclear.
CCK is released post-prandially from the small intestine (3), and has also been shown to co-localise with PYY in L cells (112) Two types of CCK receptor have been identified in the CNS and peripheral tissues CCK1 and 2 (113). CCK is released post-prandially in response to saturated fat, long-chain fatty acids, amino acids and small peptides that would normally result from protein digestion (114,115). CCK release and signalling via the CCK-1 receptors in response to these long chain fatty acids mediates stimulation of PYY release and inhibition of ghrelin (an orexigenic gut hormone) in human subjects (116).
The effects of CCK on appetite are well documented. Peripheral administration of CCK in rodents results in a dose dependant reduction in food intake, decreasing both meal size and duration (117). CCK administration is also associated with an increase in postprandial satiety behaviours such as increased grooming and decreased locomotor activity (117). In humans, intravenous administration of physiological doses of CCK reduces food intake and increases the perception of fullness (118). Unfortunately, the therapeutic potential of CCK as a treatment for obesity is limited by nausea and tachyphylaxis of the anorectic effects associated with chronic administration (119).
PP is an amidated 36-amino acid peptide and belongs to the ‘PP fold’ family of peptides. It is released post-prandially under vagal control by pancreatic islet PP cells (120–122). PP binds to all the members of the Y receptor family, but has the highest affinity for the Y4 receptor subtype (123). The effects of PP are likely to be mediated by both the hypothalamus and brainstem (124). PP is comparable to other anorectic intestinal peptides such as PYY, being secreted in proportion to caloric intake. Circulating levels rise after meals and remain elevated for up to 6 hours post-prandially (120). Intraperitoneal injection of PP acutely reduces food intake in fasted mice (124), an effect that remains apparent for 24 hours after injection. Furthermore, chronic administration of PP over 6 days in ob/ob mice significantly reduces body weight gain and improves glucose profile (124). Intravenous infusion of PP at doses that achieve normal post-prandial plasma concentrations reduces appetite in lean humans and inhibition of food intake persists for 24 hours after infusion (125). PP has also been shown to reduce food intake at lower infusion rates (126). Furthermore, pancreatic polypeptide has been shown to reduce food intake in patients with obesity secondary to Prader-Willi syndrome (127). Additionally, PP has also been implicated in energy homeostasis, with exogenous administration of PP causing an increase in oxygen consumption (124), thus implying that part of the effect of PP on body weight may be due to increased energy expenditure. It has also been shown to increase spontaneous locomotor activity in mice (128). These data have lead to a concerted effort to develop long acting PP analogues, which have completed Phase I trials (129).
NT was first isolated from hypothalamic tissue, but is widely distributed throughout the central nervous system. However, the majority of NT is found within enteroendocrine cells of the GI tract (130). NT regulates a number of digestive processes, including gastrointestinal motility, and pancreatic and biliary secretion (131). It also has trophic effects on the pancreas and small intestine (132,133). Plasma levels of NT increase after a meal, with intraluminal fat being the most potent stimulus (134). Peripheral administration of neurotensin decreases food intake and grooming behaviour in rats only at large doses (135). Therefore at physiological levels, neurotensin is unlikely to play a major role in appetite regulation. Although neurotensin acutely reduces food intake when administered centrally in rats or peripherally in mice, chronic administration to mice has no significant effect on food intake or body weight (136). The lack of chronic effects on body weight suggests that NT is unlikely to be useful as a treatment for obesity.
Intracerebroventricular injection of glucagon-like peptide-2 (GLP-2) into rats inhibits food intake. In contrast, GLP-2 administered peripherally does not inhibit food intake in rodents or humans (137,138). GLP-2 appears to play a more important physiological role as an intestinal growth factor (138).
Amylin is a peptide co-secreted with insulin by pancreatic beta cells. Injection of amylin or amylin agonist has been shown to reduce food intake in a number of species, including humans (139–143). The amylin receptor agonist pramlintide has been shown to cause weight loss in diabetic humans (141,143).
Vasoactive intestinal polypeptide (VIP) has been shown to reduce appetite, in addition to its well-characterized effects on the cardiovascular system and gastrointestinal motility and secretion. Intracerebroventricular administration of VIP has been shown to cause a potent short-lived decrease in food intake and an increase in activity and energy expenditure in rats. Treatment of hypothalamic explants with VIP stimulated the release of the anorexigenic peptide α-MSH (144). These studies suggest a possible endogenous role for VIP in the hypothalamic control of energy homeostasis.
Gut hormones and the treatment of obesity
Lifestyle and dietary modification alone are inadequate for the successful treatment of the majority of obese individuals. However, despite an increasingly high demand for intervention, the field of obesity therapeutics has limited options to offer these patients. The history of obesity pharmacotherapy is littered with examples of drugs withdrawn from the market due to adverse effects outweighing the beneficial effects of weight loss. Recent examples include Sibutramine, a norepinephrine and serotonin reuptake inhibitor, and Rimonabant, which is a cannabinoid-1 receptor blocker. Sibutramine was withdrawn after it was found to increase heart rate and blood pressure in some subjects, and was associated with an increased risk of stroke and non-fatal myocardial infarction in patients with pre-existing cardiovascular conditions (145), whilst Rimonabant was withdrawn amidst concerns regarding adverse psychiatric events (146). The only currently licensed product in the UK is Orlistat, a pancreatic lipase inhibitor which prevents fat absorption and confers a modest weight loss of 2.9 kg more than placebo over the course of a year (147).
The only obesity treatment that has been shown to confer long-term, sustained weight loss and a decrease in overall mortality is bariatric surgical intervention (148,149). Several surgical procedures are available to achieve weight loss. Gastric banding restricts the amount of food that can be comfortably ingested and increases the satiating effect of food (150). A more efficient reduction in appetite and weight loss is seen with surgical procedures that involve gastrointestinal bypass, such as Roux-en-Y Gastric bypass (RYGB) (148,149,151). Weight loss is normally associated with reduced plasma levels of the adipocyte-derived anorectic hormone leptin, causing increased hunger (152). However, following RYGB, despite significant reductions in body weight and leptin levels, appetite is markedly reduced (151). It has now been demonstrated that RYGB is more effective than either standard or intensive medical therapy in achieving glycaemic control and remission in patients with Type 2 diabetes (T2DM) (153,154). These seminal studies raise the question as to whether bariatric surgery could become a more important treatment for T2DM than medical therapy. Indeed, in a recent positional paper the International Diabetes Federation supported the selective use of various bariatric procedures for obese individuals with medically resistant T2DM (155). However, significant questions remain, not least is how long do these effects last? But also include when is the best time for surgical intervention? Does bariatric surgery work for everyone? What are the surgical/risk benefits in moderately obese patients? This list is by no means exhaustive. Given RYGB requires major surgery, which has inherent risk and is expensive, there is considerable effort aimed at determining how RYGB and other surgeries induce sustained weight loss and resolution of T2DM.
Of particular interest has been the suggestion that RYGB ameliorates coexistent type 2 diabetes mellitus before substantial weight loss has occurred and more rapidly than gastric banding. The differences between gastric banding and RYGB may be due to alterations in the anorectic and incretin gut hormone profile that is seen following RYGB, but not following gastric banding (156,157). Experimental evidence suggests that these anorectic gut hormones may mediate the effects of RYGB on appetite and body weight (157,158). Post-prandial PYY and GLP-1 levels begin to rise as early as 2 days following gastric bypass in humans (158), and secretory products of enteroendocrine L-cells, including PYY and GLP-1 remain elevated two years after bypass surgery (159). Inhibiting gut hormone release with somatostatin analogue octreotide increases the food intake after gastric bypass surgery but not following gastric banding (158), further suggesting that these hormones play a critical role. In rodent models of bariatric surgery increases in circulating GLP-1 (160) and PYY and a reduction in ghrelin (49), have been implicated in mediating the beneficial effects of these surgeries. Determining the mechanisms behind the sustained reduction in appetite may identify pathways that can be targeted by anti-obesity agents. To this end there has been recent concerted effort to mimic the rise in gut hormones following gut bypass by either the development of peptide based analogues or by the design of small molecule drugs which target nutrient sensing receptors on the enteroendocrine L-cell.
Long acting versions of PYY and OXM are being actively pursued by the pharmaceutical industry, such as Pfizer’s OAP-189, we await the dissemination of data from ongoing trials. In addition Given that gut hormones are co-released one logical approach would be the development of combination therapies. Indeed data suggests that co-administration of gut hormones can have additive effects on food intake inhibition, for example PYY + GLP-1 (161) or PYY + OXM (162). Such combination approaches may prove more effective than individual administration. Very recently the development of chimeric agonists has emerged as a novel form of combination therapy (91,92). GLP-1/glucagon co-agonists combine the appetite suppressive effects of GLP-1 and glucagon with the energy expenditure promoting effects of glucagon. Whilst at the same time GLP-1’s insulinotropic effects inhibit the detrimental hyperglycaemic effects of glucagon. Marcadia Ltd., now a subsidiary of Roche, first reported the beneficial effects of this approach and their compound is now undergoing clinical trials. In addition, Zealand Pharma is also developing a similar compound, ZP-2929, in partnership with Boehringer Mannheim. Time will tell if the promising pre-clinical data translates in to clinical benefit (163).
Considerable energy has also been directed toward the development of gut hormone secretagogues. The most well characterised class being agonists of GPR119. These compounds have been shown to release both GLP-1 and PYY (22). Their anti-diabetic effects are well defined; stimulation of GLP-1 and a direct insulinotropic action (22,164). It is less clear if these compounds will be effective as anti-obesity agents, but some agonists have been shown to significantly reduce food intake, for example PSN632408 (165). GPR119 is currently the only target for which synthetic modulators stimulate both incretin and insulin release. This highly beneficial profile has generated great industry interest with at least 9 companies actively working in this area. Initial clinical trials have been successful with respect to the anti-diabetic indication (166,167).
Conclusion
Obesity has emerged as a major global healthcare challenge. The significant mortality and morbidity associated with obesity has inspired a vast amount of research directed towards developing safe and efficacious weight-loss agents. The beneficial effects of centrally acting weight-loss agents have been negated by their potentially hazardous effects on mood, reward, dependence and autonomic tone. Gut hormones, as outlined in this article, play an important role in the homeostatic control of food intake and offer an alternative to centrally acting drugs. We believe that in time these approaches will develop clinically useful compounds which will offer a real answer to the ever growing burden of obesity.
Acknowledgments
Investigative Medicine is funded by the MRC, BBSRC, NIHR, an Integrative Mammalian Biology (IMB) Capacity Building Award, an FP7- HEALTH-2009-241592 EuroCHIP grant and by the NIHR Imperial Biomedical Research Centre Funding Scheme. GAB is funded by an NIHR Career Development Fellowship.
Footnotes
Potential conflict of interest
None declared.
References
- 1.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy KG, Dhillo WS, Bloom SR. Gut peptides in the regulation of food intake and energy homeostasis. Endocr Rev. 2006;27:719–27. doi: 10.1210/er.2006-0028. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz MW, Woods SC, Porte D, Jr, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404:661–71. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhri OB, Field BC, Bloom SR. Gastrointestinal satiety signals. J Obes (Lond) 2008;32(Suppl 7):S28–31. doi: 10.1038/ijo.2008.235. [DOI] [PubMed] [Google Scholar]
- 6.Bewick GA, Gardiner JV, Dhillo WS, Kent AS, White NE, Webster Z, et al. Postembryonic ablation of AgRP neurons in mice leads to a lean, hypophagic phenotype. FASEB J. 2005;19:1680–2. doi: 10.1096/fj.04-3434fje. [DOI] [PubMed] [Google Scholar]
- 7.Broberger C, Johansen J, Johansson C, Schalling M, Hökfelt T. The neuropeptide Y/agouti gene-related protein (AGRP) brain circuitry in normal, anorectic, and mono-sodium glutamate-treated mice. Proc Natl Acad Sci USA. 1998;95:15043–8. doi: 10.1073/pnas.95.25.15043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hahn TM, Breininger JF, Baskin DG, Schwartz MW. Coexpression of Agrp and NPY in fasting-activated hypothalamic neurons. Nat Neurosci. 1998;1:271–2. doi: 10.1038/1082. [DOI] [PubMed] [Google Scholar]
- 9.Elias CF, Lee C, Kelly J, Aschkenasi C, Ahima RS, Couceyro PR, et al. Leptin activates hypothalamic CART neurons projecting to the spinal cord. Neuron. 1998;21:1375–85. doi: 10.1016/s0896-6273(00)80656-x. [DOI] [PubMed] [Google Scholar]
- 10.Peruzzo B, Pastor FE, Blázquez JL, Schöbitz K, Peláez B, Amat P, et al. A second look at the barriers of the medial basal hypothalamus. Exp Brain Res. 2000;132:10–26. doi: 10.1007/s002219900289. [DOI] [PubMed] [Google Scholar]
- 11.Porte D, Jr, Baskin DG, Schwartz MW. Leptin and insulin action in the central nervous system. Nutr Rev. 2002;60:S20–9. doi: 10.1301/002966402320634797. discussion S68–84, 85–7. [DOI] [PubMed] [Google Scholar]
- 12.Baraboi ED, Michel C, Smith P, Thibaudeau K, Ferguson AV, Richard D. Effects of albumin-conjugated PYY on food intake: the respective roles of the circumventricular organs and vagus nerve. Eur J Neurosci. 2010;32:826–39. doi: 10.1111/j.1460-9568.2010.07318.x. [DOI] [PubMed] [Google Scholar]
- 13.Jobst EE, Enriori PJ, Cowley MA. The electrophysiology of feeding circuits. Trends Endocrinol Metab. 2004;15:488–99. doi: 10.1016/j.tem.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Sjolund K, Sanden G, Hakanson R, Sundler F. Endocrine cells in human intestine: an immunocytochemical study. Gastroenterology. 1983;85:1120–30. [PubMed] [Google Scholar]
- 15.Cheng H, Leblond CP. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. V. Unitarian Theory of the origin of the four epithelial cell types. Am J Anat. 1974;141:537–61. doi: 10.1002/aja.1001410407. [DOI] [PubMed] [Google Scholar]
- 16.Jang HJ, Kokrashvili Z, Theodorakis MJ, Carlson OD, Kim BJ, Zhou J, et al. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc Natl Acad Sci USA. 2007;104:15069–74. doi: 10.1073/pnas.0706890104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rozengurt N, Wu SV, Chen MC, Huang C, Sternini C, Rozengurt E. Colocalization of the alpha-subunit of gustducin with PYY and GLP-1 in L cells of human colon. Am J Physiol Gastrointest Liver Physiol. 2006;291:G792–802. doi: 10.1152/ajpgi.00074.2006. [DOI] [PubMed] [Google Scholar]
- 18.Karaki S, Mitsui R, Hayashi H, Kato I, Sugiya H, Iwanaga T, Furness JB, Kuwahara A. Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res. 2006;324:353–60. doi: 10.1007/s00441-005-0140-x. [DOI] [PubMed] [Google Scholar]
- 19.Tazoe H, Otomo Y, Karaki S, Kato I, Fukami Y, Terasaki M, et al. Expression of short-chain fatty acid receptor GPR41 in the human colon 2. Biomed Res. 2009;30:149–56. doi: 10.2220/biomedres.30.149. [DOI] [PubMed] [Google Scholar]
- 20.Cherbut C, Ferrier L, Rozé C, Anini Y, Blottière H, Lecannu G, Galmiche JP. Short-chain fatty acids modify colonic motility through nerves and polypeptide YY release in the rat. Am J Physiol. 1998;275:G1415–22. doi: 10.1152/ajpgi.1998.275.6.G1415. [DOI] [PubMed] [Google Scholar]
- 21.Fu-Cheng X, Anini Y, Chariot J, Voisin T, Galmiche JP, Rozé C. Peptide YY release after intraduodenal, intraileal, and intracolonic administration of nutrients in rats. Pflugers Arch. 1995;431:66–75. doi: 10.1007/BF00374378. [DOI] [PubMed] [Google Scholar]
- 22.Chu ZL, Carroll C, Alfonso J, Gutierrez V, He H, Lucman A, et al. A role for intestinal endocrine cell-expressed g protein-coupled receptor 119 in glycemic control by enhancing glucagon-like Peptide-1 and glucose-dependent insulinotropic Peptide release. Endocrinology. 2008;149:2038–47. doi: 10.1210/en.2007-0966. [DOI] [PubMed] [Google Scholar]
- 23.Lauffer LM, Iakoubov R, Brubaker PL. GPR119 is essential for oleoylethanolamide-induced glucagon-like peptide-1 secretion from the intestinal enteroendocrine L-cell. Diabetes. 2009;58:1058–66. doi: 10.2337/db08-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cummings DE, Overduin J. Gastrointestinal regulation of food intake. J Clin Invest. 2007;117:13–23. doi: 10.1172/JCI30227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy KG, Bloom SR. Gut hormones and the regulation of energy homeostasis. Nature. 2006;444:854–9. doi: 10.1038/nature05484. [DOI] [PubMed] [Google Scholar]
- 26.Adrian TE, Ferri GL, Bacarese-Hamilton AJ, Fuessl HS, Polak JM, Bloom SR. Human distribution and release of a putative new gut hormone, peptide YY. Gastroenterology. 1985;89:1070–77. doi: 10.1016/0016-5085(85)90211-2. [DOI] [PubMed] [Google Scholar]
- 27.Le Quellec A, Kervran A, Blache P, Ciurana AJ, Bataille D. Oxyntomodulin-like immunoreactivity: diurnal profile of a new potential enterogastrone. J Clin Endocrinol Metab. 1992;74:1405–9. doi: 10.1210/jcem.74.6.1592887. [DOI] [PubMed] [Google Scholar]
- 28.Badman MK, Flier JS. The gut and energy balance: visceral allies in the obesity wars. Science. 2005;307:1909–14. doi: 10.1126/science.1109951. [DOI] [PubMed] [Google Scholar]
- 29.Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, et al. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature. 2002;418:650–4. doi: 10.1038/nature00887. [DOI] [PubMed] [Google Scholar]
- 30.Lin HC, Zhao XT, Wang L, Wong H. Fat-induced ileal brake in the dog depends on peptide YY. Gastroenterology. 1996;110:1491–5. doi: 10.1053/gast.1996.v110.pm8613054. [DOI] [PubMed] [Google Scholar]
- 31.Wen J, Phillips SF, Sarr MG, Kost LJ, Holst JJ. PYY and GLP-1 contribute to feedback inhibition from the canine ileum and colon. Am J Physiol. 1995;269:G945–52. doi: 10.1152/ajpgi.1995.269.6.G945. [DOI] [PubMed] [Google Scholar]
- 32.Grandt D, Schimiczek M, Beglinger C, Layer P, Goebell H, Eysselein VE, et al. Two molecular forms of peptide YY (PYY) are abundant in human blood: characterization of a radioimmunoassay recognizing PYY 1-36 and PYY 3-36. Regul Pept. 1994;51:151–9. doi: 10.1016/0167-0115(94)90204-6. [DOI] [PubMed] [Google Scholar]
- 33.Medeiros MD, Turner AJ. Processing and metabolism of peptide-YY: pivotal roles of dipeptidylpeptidase-IV, aminopeptidase-P, and endopeptidase-24.11. Endocrinology. 1994;134:2088–94. doi: 10.1210/endo.134.5.7908871. [DOI] [PubMed] [Google Scholar]
- 34.Larhammar D. Structural diversity of receptors for neuropeptide Y, peptide YY and pancreatic polypeptide. Regul Pept. 1996;65:165–74. doi: 10.1016/0167-0115(96)00110-3. [DOI] [PubMed] [Google Scholar]
- 35.Grandt D, Teyssen S, Schimiczek M, Reeve JR, Jr, Feth F, Rascher W, et al. Novel generation of hormone receptor specificity by amino terminal processing of peptide YY. Biochem Biophys Res Commun. 1992;186:1299–306. doi: 10.1016/s0006-291x(05)81547-5. [DOI] [PubMed] [Google Scholar]
- 36.Broberger C, Landry M, Wong H, Walsh JN, Hökfelt T. Subtypes Y1 and Y2 of the neuropeptide Y receptor are respectively expressed in pro-opiomelanocortin- and neuropeptide-Y-containing neurons of the rat hypothalamic arcuate nucleus. Neuroendocrinology. 1997;66:393–408. doi: 10.1159/000127265. [DOI] [PubMed] [Google Scholar]
- 37.Abbott CR, Small CJ, Kennedy AR, Neary NM, Sajedi A, Ghatei MA, et al. Blockade of the neuropeptide Y Y2 receptor with the specific antagonist BIIE0246 attenuates the effect of endogenous and exogenous peptide YY(3-36) on food intake. Brain Res. 2005;1043:139–44. doi: 10.1016/j.brainres.2005.02.065. [DOI] [PubMed] [Google Scholar]
- 38.Batterham RL, Bloom SR. The gut hormone peptide YY regulates appetite. Ann N Y Acad Sci. 2003;994:162–8. doi: 10.1111/j.1749-6632.2003.tb03176.x. [DOI] [PubMed] [Google Scholar]
- 39.Batterham RL, Heffron H, Kapoor S, Chivers JE, Chandarana K, Herzog H, et al. Critical role for peptide YY in protein-mediated satiation and body-weight regulation. Cell Metab. 2006;4:223–33. doi: 10.1016/j.cmet.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 40.Pedersen-Bjergaard U, Host U, Kelbaek H, Schifter S, Rehfeld JF, Faber J, et al. Influence of meal composition on postprandial peripheral plasma concentrations of vasoactive peptides in man. Scand J Clin Lab Invest. 1996;56:497–503. doi: 10.3109/00365519609088805. [DOI] [PubMed] [Google Scholar]
- 41.Challis BG, Pinnock SB, Coll AP, Carter RN, Dickson SL, O’Rahilly S. Acute effects of PYY3-36 on food intake and hypothalamic neuropeptide expression in the mouse. Biochem Biophys Res Commun. 2003;311:915–9. doi: 10.1016/j.bbrc.2003.10.089. [DOI] [PubMed] [Google Scholar]
- 42.Chelikani PK, Haver AC, Reidelberger RD. Intravenous infusion of peptide YY(3-36) potently inhibits food intake in rats. Endocrinology. 2005;146:879–88. doi: 10.1210/en.2004-1138. [DOI] [PubMed] [Google Scholar]
- 43.Vrang N, Madsen AN, Tang-Christensen M, Hansen G, Larsen PJ. PYY(3-36) reduces food intake and body weight and improves insulin sensitivity in rodent models of diet-induced obesity. Am J Physiol Regul Integr Comp Physiol. 2006;291:R367–75. doi: 10.1152/ajpregu.00726.2005. [DOI] [PubMed] [Google Scholar]
- 44.Batterham RL, Cohen MA, Ellis SM, Le Roux CW, Withers DJ, Frost GS, et al. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med. 2003;349:941–8. doi: 10.1056/NEJMoa030204. [DOI] [PubMed] [Google Scholar]
- 45.Ghamari-Langroudi M, Colmers WF, Cone RD. PYY3-36 inhibits the action potential firing activity of POMC neurons of arcuate nucleus through postsynaptic Y2 receptors. Cell Metab. 2005;2:191–9. doi: 10.1016/j.cmet.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 46.Challis BG, Coll AP, Yeo GS, Pinnock SB, Dickson SL, Thresher RR, et al. Mice lacking pro-opiomelanocortin are sensitive to high-fat feeding but respond normally to the acute anorectic effects of peptide-YY3-36. Proc Natl Acad Sci USA. 2004;101:4695–700. doi: 10.1073/pnas.0306931101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koda S, Date Y, Murakami N, Shimbara T, Hanada T, Toshinai K, et al. The role of the vagal nerve in peripheral PYY3-36-induced feeding reduction in rats. Endocrinology. 2005;146:2369–75. doi: 10.1210/en.2004-1266. [DOI] [PubMed] [Google Scholar]
- 48.Abbott CR, Monteiro M, Small CJ, Sajedi A, Smith KL, Parkinson JR, et al. The inhibitory effects of peripheral administration of peptide YY(3-36) and glucagon-like peptide-1 on food intake are attenuated by ablation of the vagal-brainstem-hypothalamic pathway. Brain Res. 2005;1044:127–31. doi: 10.1016/j.brainres.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 49.Chandarana K, Gelegen C, Karra E, Choudhury AI, Drew ME, Fauveau V, et al. Diet and gastrointestinal bypass-induced weight loss: the roles of ghrelin and peptide YY. Diabetes. 2011;60:810–8. doi: 10.2337/db10-0566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dhanvantari S, Seidah NG, Brubaker PL. Role of prohormone convertases in the tissue-specific processing of proglucagon. Mol Endocrinol. 1996;10:342–55. doi: 10.1210/mend.10.4.8721980. [DOI] [PubMed] [Google Scholar]
- 51.Herrmann C, Göke R, Richter G, Fehmann HC, Arnold R, Göke B. Glucagon-like peptide-1 and glucose-dependent insulin-releasing polypeptide plasma levels in response to nutrients. Digestion. 1995;56:117–26. doi: 10.1159/000201231. [DOI] [PubMed] [Google Scholar]
- 52.MacDonald PE, El-Kholy W, Riedel MJ, Salapatek AM, Light PE, Wheeler MB. The multiple actions of GLP-1 on the process of glucose-stimulated insulin secretion. Diabetes. 2002;51(Suppl 3):S434–42. doi: 10.2337/diabetes.51.2007.s434. [DOI] [PubMed] [Google Scholar]
- 53.Willms B, Werner J, Holst JJ, Orskov C, Creutzfeldt W, Nauck MA. Gastric emptying, glucose responses, and insulin secretion after a liquid test meal: effects of exogenous glucagon-like peptide-1 (GLP-1)-(7-36) amide in type 2 (noninsulin-dependent) diabetic patients. J Clin Endocrinol Metab. 1996;81:327–32. doi: 10.1210/jcem.81.1.8550773. [DOI] [PubMed] [Google Scholar]
- 54.Schirra J, Nicolaus M, Roggel R, Katschinski M, Storr M, Woerle HJ, et al. Endogenous glucagon-like peptide 1 controls endocrine pancreatic secretion and antro-pyloro-duodenal motility in humans. Gut. 2006;55:243–51. doi: 10.1136/gut.2004.059741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meeran K, O’Shea D, Edwards CM, Turton MD, Heath MM, Gunn I, et al. Repeated intracerebroventricular administration of glucagon-like peptide-1-(7-36) amide or exendin-(9-39) alters body weight in the rat. Endocrinology. 1999;140:244–50. doi: 10.1210/endo.140.1.6421. [DOI] [PubMed] [Google Scholar]
- 56.Punjabi M, Arnold M, Geary N, Langhans W, Pacheco-López G. Peripheral glucagon-like peptide-1 (GLP-1) and satiation. Physiol Behav. 2011;105:71–6. doi: 10.1016/j.physbeh.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 57.Shughrue PJ, Lane MV, Merchenthaler I. Glucagon-like peptide-1 receptor (GLP1-R) mRNA in the rat hypothalamus. Endocrinology. 1996;137:5159–62. doi: 10.1210/endo.137.11.8895391. [DOI] [PubMed] [Google Scholar]
- 58.Tang-Christensen M, Vrang N, Larsen PJ. Glucagon-like peptide containing pathways in the regulation of feeding behaviour. Int J Obes Relat Metab Disord. 2001;25(Suppl 5):S42–7. doi: 10.1038/sj.ijo.0801912. [DOI] [PubMed] [Google Scholar]
- 59.Turton MD, O’Shea D, Gunn I, Beak SA, Edwards CM, Meeran K, et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature. 1996;379:69–72. doi: 10.1038/379069a0. [DOI] [PubMed] [Google Scholar]
- 60.Verdich C, Flint A, Gutzwiller JP, Näslund E, Beglinger C, Hellström PM, et al. A meta-analysis of the effect of glucagon-like peptide-1 (7-36) amide on ad libitum energy intake in humans. J Clin Endocrinol Metab. 2001;86:4382–9. doi: 10.1210/jcem.86.9.7877. [DOI] [PubMed] [Google Scholar]
- 61.Näslund E, Bogefors J, Skogar S, Grybäck P, Jacobsson H, Holst JJ, et al. GLP-1 slows solid gastric emptying and inhibits insulin, glucagon, and PYY release in humans. Am J Physiol. 1999;277:R910–6. doi: 10.1152/ajpregu.1999.277.3.R910. [DOI] [PubMed] [Google Scholar]
- 62.Nauck MA, Niedereichholz U, Ettler R, Holst JJ, Orskov C, Ritzel R, et al. Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol. 1997;273:E981–8. doi: 10.1152/ajpendo.1997.273.5.E981. [DOI] [PubMed] [Google Scholar]
- 63.Imeryüz N, Yeğen BC, Bozkurt A, Coşkun T, Villanueva-Peñacarrillo ML, Ulusoy NB. Glucagon-like peptide-1 inhibits gastric emptying via vagal afferent-mediated central mechanisms. Am J Physiol. 1997;273:G920–7. doi: 10.1152/ajpgi.1997.273.4.G920. [DOI] [PubMed] [Google Scholar]
- 64.Parkinson JR, Chaudhri OB, Kuo YT, Field BC, Herlihy AH, Dhillo WS, et al. Differential patterns of neuronal activation in the brainstem and hypothalamus following peripheral injection of GLP-1, oxyntomodulin and lithium chloride in mice detected by manganese-enhanced magnetic resonance imaging (MEMRI) Neuroimage. 2009;44:1022–31. doi: 10.1016/j.neuroimage.2008.09.047. [DOI] [PubMed] [Google Scholar]
- 65.Joy SV, Rodgers PT, Scates AC. Incretin mimetics as emerging treatments for type 2 diabetes. Ann Pharmacother. 2005;39:110–8. doi: 10.1345/aph.1E245. [DOI] [PubMed] [Google Scholar]
- 66.Eng J, Kleinman WA, Singh L, Singh G, Raufman JP. Isolation and characterization of exendin-4, an exendin-3 analogue, from Heloderma suspectum venom. Further evidence for an exendin receptor on dispersed acini from guinea pig pancreas. J Biol Chem. 1992;267:7402–5. [PubMed] [Google Scholar]
- 67.Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3:153–65. doi: 10.1016/j.cmet.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 68.Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–705. doi: 10.1016/S0140-6736(06)69705-5. [DOI] [PubMed] [Google Scholar]
- 69.Buse JB, Henry RR, Han J, Kim DD, Fineman MS, Baron AD, et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care. 2004;27:2628–35. doi: 10.2337/diacare.27.11.2628. [DOI] [PubMed] [Google Scholar]
- 70.DeFronzo RA, Ratner RE, Han J, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care. 2005;28:1092–100. doi: 10.2337/diacare.28.5.1092. [DOI] [PubMed] [Google Scholar]
- 71.Kendall DM, Riddle MC, Rosenstock J, Zhuang D, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care. 2005;28:1083–91. doi: 10.2337/diacare.28.5.1083. [DOI] [PubMed] [Google Scholar]
- 72.Astrup A, Carraro R, Finer N, Harper A, Kunesova M, Lean ME, et al. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond) 2012;36:843–54. doi: 10.1038/ijo.2011.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tzefos M, Harris K, Brackett A. Clinical efficacy and safety of once-weekly glucagon-like peptide-1 agonists in development for treatment of type 2 diabetes mellitus in adults. Ann Pharmacother. 2012;46:68–78. doi: 10.1345/aph.1Q379. [DOI] [PubMed] [Google Scholar]
- 74.Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ. Oxyntomodulin from distal gut. Role in regulation of gastric and pancreatic functions. Dig Dis Sci. 1989;34:1411–9. doi: 10.1007/BF01538078. [DOI] [PubMed] [Google Scholar]
- 75.Dakin CL, Gunn I, Small CJ, Edwards CM, Hay DL, Smith DM, et al. Oxyntomodulin inhibits food intake in the rat. Endocrinology. 2001;142:4244–50. doi: 10.1210/endo.142.10.8430. [DOI] [PubMed] [Google Scholar]
- 76.Dakin CL, Small CJ, Batterham RL, Neary NM, Cohen MA, Patterson M, et al. Peripheral oxyntomodulin reduces food intake and body weight gain in rats. Endocrinology. 2004;145:2687–95. doi: 10.1210/en.2003-1338. [DOI] [PubMed] [Google Scholar]
- 77.Dakin CL, Small CJ, Park AJ, Seth A, Ghatei MA, Bloom SR. Repeated ICV administration of oxyntomodulin causes a greater reduction in body weight gain than in pair-fed rats. Am J Physiol Endocrinol Metab. 2002;283:E1173–7. doi: 10.1152/ajpendo.00233.2002. [DOI] [PubMed] [Google Scholar]
- 78.Cohen MA, Ellis SM, Le Roux CW, Batterham RL, Park A, Patterson M, et al. Oxyntomodulin suppresses appetite and reduces food intake in humans. J Clin Endocrinol Metab. 2003;88:4696–701. doi: 10.1210/jc.2003-030421. [DOI] [PubMed] [Google Scholar]
- 79.Wynne K, Park AJ, Small CJ, Patterson M, Ellis SM, Murphy KG, et al. Subcutaneous oxyntomodulin reduces body weight in overweight and obese subjects: a double-blind, randomized, controlled trial. Diabetes. 2005;54:2390–5. doi: 10.2337/diabetes.54.8.2390. [DOI] [PubMed] [Google Scholar]
- 80.Wynne K, Park AJ, Small CJ, Meeran K, Ghatei MA, Frost GS, Bloom SR. Oxyntomodulin increases energy expenditure in addition to decreasing energy intake in overweight and obese humans: a randomised controlled trial. Int J Obes (Lond) 2006;30:1729–36. doi: 10.1038/sj.ijo.0803344. [DOI] [PubMed] [Google Scholar]
- 81.Baggio LL, Huang Q, Brown TJ, Drucker DJ. Oxyntomodulin and glucagon-like peptide-1 differentially regulate murine food intake and energy expenditure. Gastroenterology. 2004;127:546–58. doi: 10.1053/j.gastro.2004.04.063. [DOI] [PubMed] [Google Scholar]
- 82.Chaudhri OB, Parkinson JR, Kuo YT, Druce MR, Herlihy AH, Bell JD, et al. Differential hypothalamic neuronal activation following peripheral injection of GLP-1 and oxyntomodulin in mice detected by manganese-enhanced magnetic resonance imaging. Biochem Biophys Res Commun. 2006;350:298–306. doi: 10.1016/j.bbrc.2006.09.033. [DOI] [PubMed] [Google Scholar]
- 83.Striffler J, Cardell EL, Cardell RR., Jr Effects of glucagon on hepatic glycogen and smooth endoplasmic reticulum. Am J Anat. 1981;160:363–79. doi: 10.1002/aja.1001600402. [DOI] [PubMed] [Google Scholar]
- 84.Studer RK, Snowdowne KW, Borle AB. Regulation of hepatic glycogenolysis by glucagon in male and female rats. Role of cAMP and Ca2+ and interactions between epinephrine and glucagon. J Biol Chem. 1984;259:3596–604. [PubMed] [Google Scholar]
- 85.Stevenson RW, Steiner KE, Davis MA, Hendrick GK, Williams PE, Lacy WW, et al. Similar dose responsiveness of hepatic glycogenolysis and gluconeogenesis to glucagon in vivo. Diabetes. 1987;36:382–9. doi: 10.2337/diab.36.3.382. [DOI] [PubMed] [Google Scholar]
- 86.Wasserman DH, Spalding JA, Bracy D, Lacy DB, Cherrington AD. Exercise-induced rise in glucagon and keto-genesis during prolonged muscular work. Diabetes. 1989;38:799–807. doi: 10.2337/diab.38.6.799. [DOI] [PubMed] [Google Scholar]
- 87.Svoboda M, Tastenoy M, Vertongen P, Robberecht P. Relative quantitative analysis of glucagon receptor mRNA in rat tissues. Mol Cell Endocrinol. 1994;105:131–7. doi: 10.1016/0303-7207(94)90162-7. [DOI] [PubMed] [Google Scholar]
- 88.Nair KS. Hyperglucagonemia increases resting metabolic rate in man during insulin deficiency. J Clin Endocrinol Metab. 1987;64:896–901. doi: 10.1210/jcem-64-5-896. [DOI] [PubMed] [Google Scholar]
- 89.Schulman JL, Carleton JL, Whitney G, Whitehorn JC. Effect of glucagon on food intake and body weight in man. J Appl Physiol. 1957;11:419–21. doi: 10.1152/jappl.1957.11.3.419. [DOI] [PubMed] [Google Scholar]
- 90.Geary N, Le Sauter J, Noh U. Glucagon acts in the liver to control spontaneous meal size in rats. Am J Physiol. 1993;264:R116–22. doi: 10.1152/ajpregu.1993.264.1.R116. [DOI] [PubMed] [Google Scholar]
- 91.Pocai A, Carrington PE, Adams JR, Wright M, Eiermann G, Zhu L, et al. Glucagon-like peptide 1/glucagon receptor dual agonism reverses obesity in mice. Diabetes. 2009;58:2258–66. doi: 10.2337/db09-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Day JW, Ottaway N, Patterson JT, Gelfanov V, Smiley D, Gidda J, et al. A new glucagon and GLP-1 co-agonist eliminates obesity in rodents. Nat Chem Biol. 2009;5:749–57. doi: 10.1038/nchembio.209. [DOI] [PubMed] [Google Scholar]
- 93.Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–60. doi: 10.1038/45230. [DOI] [PubMed] [Google Scholar]
- 94.Bewick GA, Kent A, Campbell D, Patterson M, Ghatei MA, Bloom SR, Gardiner JV. Mice with hyperghrelinemia are hyperphagic and glucose intolerant and have reduced leptin sensitivity. Diabetes. 2009;58:840–6. doi: 10.2337/db08-1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lawrence CB, Snape AC, Baudoin FM, Luckman SM. Acute central ghrelin and GH secretagogues induce feeding and activate brain appetite centers. Endocrinology. 2002;143:155–62. doi: 10.1210/endo.143.1.8561. [DOI] [PubMed] [Google Scholar]
- 96.Tschöp M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000;407:908–13. doi: 10.1038/35038090. [DOI] [PubMed] [Google Scholar]
- 97.Wren AM, Small CJ, Ward HL, Murphy KG, Dakin CL, Taheri S, et al. The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology. 2000;141:4325–8. doi: 10.1210/endo.141.11.7873. [DOI] [PubMed] [Google Scholar]
- 98.Masuda Y, Tanaka T, Inomata N, Ohnuma N, Tanaka S, Itoh Z, et al. Ghrelin stimulates gastric acid secretion and motility in rats. Biochem Biophys Res Commun. 2000;276:905–8. doi: 10.1006/bbrc.2000.3568. [DOI] [PubMed] [Google Scholar]
- 99.Toshinai K, Mondal MS, Nakazato M, Date Y, Murakami N, Kojima M, et al. Upregulation of Ghrelin expression in the stomach upon fasting, insulin-induced hypoglycemia, and leptin administration. Biochem Biophys Res Commun. 2001;281:1220–5. doi: 10.1006/bbrc.2001.4518. [DOI] [PubMed] [Google Scholar]
- 100.Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, et al. Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab. 2001;86:4753–8. doi: 10.1210/jcem.86.10.7885. [DOI] [PubMed] [Google Scholar]
- 101.Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623–30. doi: 10.1056/NEJMoa012908. [DOI] [PubMed] [Google Scholar]
- 102.Shiiya T, Nakazato M, Mizuta M, Date Y, Mondal MS, Tanaka M, et al. Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J Clin Endocrinol Metab. 2002;87:240–4. doi: 10.1210/jcem.87.1.8129. [DOI] [PubMed] [Google Scholar]
- 103.Tschöp M, Wawarta R, Riepl RL, Friedrich S, Bidlingmaier M, Landgraf R, Folwaczny C. Post-prandial decrease of circulating human ghrelin levels. J Endocrinol Invest. 2001;24:RC19–21. doi: 10.1007/BF03351037. [DOI] [PubMed] [Google Scholar]
- 104.Hewson AK, Dickson SL. Systemic administration of ghrelin induces Fos and Egr-1 proteins in the hypothalamic arcuate nucleus of fasted and fed rats. J Neuroendocrinol. 2000;12:1047–9. doi: 10.1046/j.1365-2826.2000.00584.x. [DOI] [PubMed] [Google Scholar]
- 105.Tamura H, Kamegai J, Shimizu T, Ishii S, Sugihara H, Oikawa S. Ghrelin stimulates GH but not food intake in arcuate nucleus ablated rats. Endocrinology. 2002;143:3268–75. doi: 10.1210/en.2002-220268. [DOI] [PubMed] [Google Scholar]
- 106.Page AJ, Slattery JA, Milte C, Laker R, O’Donnell T, Dorian C, et al. Ghrelin selectively reduces mechanosensitivity of upper gastrointestinal vagal afferents. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1376–84. doi: 10.1152/ajpgi.00536.2006. [DOI] [PubMed] [Google Scholar]
- 107.Date Y, Murakami N, Toshinai K, Matsukura S, Niijima A, Matsuo H, et al. The role of the gastric afferent vagal nerve in ghrelin-induced feeding and growth hormone secretion in rats. Gastroenterology. 2002;123:1120–8. doi: 10.1053/gast.2002.35954. [DOI] [PubMed] [Google Scholar]
- 108.Briggs DI, Enriori PJ, Lemus MB, Cowley MA, Andrews ZB. Diet-induced obesity causes ghrelin resistance in arcuate NPY/AgRP neurons. Endocrinology. 2010;151:4745–55. doi: 10.1210/en.2010-0556. [DOI] [PubMed] [Google Scholar]
- 109.Gardiner JV, Campbell D, Patterson M, Kent A, Ghatei MA, Bloom SR, Bewick GA. The hyperphagic effect of ghrelin is inhibited in mice by a diet high in fat. Gastroenterology. 2010;138:2468–76. doi: 10.1053/j.gastro.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 110.Perez-Tilve D, Heppner K, Kirchner H, Lockie SH, Woods SC, Smiley DL, et al. Ghrelin-induced adiposity is independent of orexigenic effects. FASEB J. 2011;25:2814–22. doi: 10.1096/fj.11-183632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chuang JC, Perello M, Sakata I, Osborne-Lawrence S, Savitt JM, Lutter M, Zigman JM. Ghrelin mediates stress-induced food-reward behavior in mice. J Clin Invest. 2011;121:2684–92. doi: 10.1172/JCI57660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Roth KA, Kim S, Gordon JI. Immunocytochemical studies suggest two pathways for enteroendocrine cell differentiation in the colon. Am J Physiol. 1992;263:G174–80. doi: 10.1152/ajpgi.1992.263.2.G174. [DOI] [PubMed] [Google Scholar]
- 113.Moran TH, Robinson PH, Goldrich MS, McHugh PR. Two brain cholecystokinin receptors: implications for behavioral actions. Brain Res. 1986;362:175–9. doi: 10.1016/0006-8993(86)91413-7. [DOI] [PubMed] [Google Scholar]
- 114.Liddle RA, Goldfine ID, Rosen MS, Taplitz RA, Williams JA. Cholecystokinin bioactivity in human plasma. Molecular forms, responses to feeding, and relationship to gallbladder contraction. J Clin Invest. 1985;75:1144–52. doi: 10.1172/JCI111809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rehfeld JF, Bungaard JR, Friis-Hansen L, Goetze JP. On the tissue-specific processing of procholecystokinin in the brain and gut--a short review. J Physiol Pharmacol. 2003;54(Suppl 4):73–9. [PubMed] [Google Scholar]
- 116.Degen L, Drewe J, Piccoli F, Gräni K, Oesch S, Bunea R, et al. Effect of CCK-1 receptor blockade on ghrelin and PYY secretion in men. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1391–9. doi: 10.1152/ajpregu.00734.2006. [DOI] [PubMed] [Google Scholar]
- 117.Antin J, Gibbs J, Holt J, Young RC, Smith GP. Cholecystokinin elicits the complete behavioral sequence of satiety in rats. J Comp Physiol Psychol. 1975;89:784–90. doi: 10.1037/h0077040. [DOI] [PubMed] [Google Scholar]
- 118.Lieverse RJ, Jansen JB, Masclee AA, Lamers CB. Satiety effects of a physiological dose of cholecystokinin in humans. Gut. 1995;36:176–9. doi: 10.1136/gut.36.2.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Covasa M, Marcuson JK, Ritter RC. Diminished satiation in rats exposed to elevated levels of endogenous or exogenous cholecystokinin. Am J Physiol Regul Integr Comp Physiol. 2001;280:R331–7. doi: 10.1152/ajpregu.2001.280.2.R331. [DOI] [PubMed] [Google Scholar]
- 120.Adrian TE, Bloom SR, Bryant MG, Polak JM, Heitz PH, Barnes AJ. Distribution and release of human pancreatic polypeptide. Gut. 1976;17:940–44. doi: 10.1136/gut.17.12.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Larsson LI, Sundler F, Håkanson R. Immunohistochemical localization of human pancreatic polypeptide (HPP) to a population of islet cells. Cell Tissue Res. 1975;156:167–71. doi: 10.1007/BF00221800. [DOI] [PubMed] [Google Scholar]
- 122.Schwartz TW, Holst JJ, Fahrenkrug J, Jensen SL, Nielsen OV, Rehfeld JF, et al. Vagal, cholinergic regulation of pancreatic polypeptide secretion. J Clin Invest. 1978;61:781–9. doi: 10.1172/JCI108992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Michel MC, Beck-Sickinger A, Cox H, Doods HN, Herzog H, Larhammar D, et al. XVI. International Union of Pharmacology recommendations for the nomenclature of neuropeptide Y, peptide YY, and pancreatic polypeptide receptors. Pharmacol Rev. 1998;50:143–50. [PubMed] [Google Scholar]
- 124.Asakawa A, Inui A, Yuzuriha H, Ueno N, Katsuura G, Fujimiya M, et al. Characterization of the effects of pancreatic polypeptide in the regulation of energy balance. Gastroenterology. 2003:1241325–36. doi: 10.1016/s0016-5085(03)00216-6. [DOI] [PubMed] [Google Scholar]
- 125.Batterham RL, Le Roux CW, Cohen MA, Park AJ, Ellis SM, Patterson M, et al. Pancreatic polypeptide reduces appetite and food intake in humans. J Clin Endocrinol Metab. 2003;88:3989–92. doi: 10.1210/jc.2003-030630. [DOI] [PubMed] [Google Scholar]
- 126.Jesudason DR, Monteiro MP, McGowan BM, Neary NM, Park AJ, Philippou E, et al. Low-dose pancreatic polypeptide inhibits food intake in man. Br J Nutr. 2007;97:426–9. doi: 10.1017/S0007114507336799. [DOI] [PubMed] [Google Scholar]
- 127.Berntson GG, Zipf WB, O’Dorisio TM, Hoffman JA, Chance RE. Pancreatic polypeptide infusions reduce food intake in Prader-Willi syndrome. Peptides. 1993;14:497–503. doi: 10.1016/0196-9781(93)90138-7. [DOI] [PubMed] [Google Scholar]
- 128.Liu YL, Semjonous NM, Murphy KG, Ghatei MA, Bloom SR. The effects of pancreatic polypeptide on locomotor activity and food intake in mice. Int J Obes (Lond) 2008;32:1712–5. doi: 10.1038/ijo.2008.160. [DOI] [PubMed] [Google Scholar]
- 129.Tan TM, Field BC, Minnion JS, Cuenco-Shillito J, Chambers ES, Zac-Varghese S, et al. Pharmacokinetics, adverse effects and tolerability of a novel analogue of human pancreatic polypeptide, PP 1420. Br J Clin Pharmacol. 2012;73:232–9. doi: 10.1111/j.1365-2125.2011.04082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Carraway R, Leeman SE. Characterization of radioimmunoassayable neurotensin in the rat. Its differential distribution in the central nervous system, small intestine, and stomach. J Biol Chem. 1976;251:7045–52. [PubMed] [Google Scholar]
- 131.Kitabgi P. Prohormone convertases differentially process pro-neurotensin/neuromedin N in tissues and cell lines. J Mol Med (Berl) 2006;84:628–34. doi: 10.1007/s00109-006-0044-6. [DOI] [PubMed] [Google Scholar]
- 132.Feurle GE, Müller B, Rix E. Neurotensin induces hyperplasia of the pancreas and growth of the gastric antrum in rats. Gut. 1987;28(Suppl):19–23. doi: 10.1136/gut.28.suppl.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wood JG, Hoang HD, Bussjaeger LJ, Solomon TE. Neurotensin stimulates growth of small intestine in rats. Am J Physiol. 1988;255:G813–7. doi: 10.1152/ajpgi.1988.255.6.G813. [DOI] [PubMed] [Google Scholar]
- 134.Rosell S, Rökaeus A. The effect of ingestion of amino acids, glucose and fat on circulating neurotensin-like immunoreactivity (NTLI) in man. Acta Physiol Scand. 1979;107:263–67. doi: 10.1111/j.1748-1716.1979.tb06472.x. [DOI] [PubMed] [Google Scholar]
- 135.Sandoval SL, Kulkosky PJ. Effects of peripheral neurotensin on behavior of the rat. Pharmacol Biochem Behav. 1992;41:385–90. doi: 10.1016/0091-3057(92)90115-v. [DOI] [PubMed] [Google Scholar]
- 136.Cooke JH, Patterson M, Patel SR, Smith KL, Ghatei MA, Bloom SR, Murphy KG. Peripheral and central administration of xenin and neurotensin suppress food intake in rodents. Obesity (Silver Spring) 2009;17:1135–43. doi: 10.1038/oby.2008.652. [DOI] [PubMed] [Google Scholar]
- 137.Schmidt PT, Näslund E, Grybäck P, Jacobsson H, Hartmann B, Holst JJ, Hellström PM. Peripheral administration of GLP-2 to humans has no effect on gastric emptying or satiety. Regul Pept. 2003;116:21–5. doi: 10.1016/s0167-0115(03)00175-7. [DOI] [PubMed] [Google Scholar]
- 138.Scott RB, Kirk D, MacNaughton WK, Meddings JB. GLP-2 augments the adaptive response to massive intestinal re-section in rat. Am J Physiol. 1998;275:G911–21. doi: 10.1152/ajpgi.1998.275.5.G911. [DOI] [PubMed] [Google Scholar]
- 139.Chance WT, Balasubramaniam A, Stallion A, Fischer JE. Anorexia following the systemic injection of amylin. Brain Res. 1993;607:185–8. doi: 10.1016/0006-8993(93)91505-m. [DOI] [PubMed] [Google Scholar]
- 140.Lutz TA, Del Prete E, Scharrer E. Reduction of food intake in rats by intraperitoneal injection of low doses of amylin. Physiol Behav. 1994;55:891–5. doi: 10.1016/0031-9384(94)90076-0. [DOI] [PubMed] [Google Scholar]
- 141.Ratner R, Whitehouse F, Fineman MS, Strobel S, Shen L, Maggs DG, et al. Adjunctive therapy with pramlintide lowers HbA1c without concomitant weight gain and increased risk of severe hypoglycemia in patients with type 1 diabetes approaching glycemic targets. Exp Clin Endocrinol Diabetes. 2005;113:199–204. doi: 10.1055/s-2005-837662. [DOI] [PubMed] [Google Scholar]
- 142.Rushing PA, Hagan MM, Seeley RJ, Lutz TA, Woods SC. Amylin: a novel action in the brain to reduce body weight. Endocrinology. 2000;141:850–3. doi: 10.1210/endo.141.2.7378. [DOI] [PubMed] [Google Scholar]
- 143.Whitehouse F, Kruger DF, Fineman M, Shen L, Ruggles JA, Maggs DG, et al. A randomized study and open-label extension evaluating the long-term efficacy of pramlintide as an adjunct to insulin therapy in type 1 diabetes. Diabetes Care. 2002;25:724–30. doi: 10.2337/diacare.25.4.724. [DOI] [PubMed] [Google Scholar]
- 144.Ghourab S, Beale KE, Semjonous NM, Simpson KA, Martin NM, Ghatei MA, et al. Intracerebroventricular administration of vasoactive intestinal peptide inhibits food intake. Regul Pept. 2011;172:8–15. doi: 10.1016/j.regpep.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 145.James WP, Caterson ID, Coutinho W, Finer N, Van Gaal LF, Maggioni AP, et al. Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med. 2010;363:905–17. doi: 10.1056/NEJMoa1003114. [DOI] [PubMed] [Google Scholar]
- 146.Christensen R, Kristensen PK, Bartels EM, Bliddal H, Astrup A. Efficacy and safety of the weight-loss drug rimonabant: a meta-analysis of randomised trials. Lancet. 2007;370:1706–13. doi: 10.1016/S0140-6736(07)61721-8. [DOI] [PubMed] [Google Scholar]
- 147.Rucker D, Padwal R, Li SK, Curioni C, Lau DC. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007;335:1194–9. doi: 10.1136/bmj.39385.413113.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61. doi: 10.1056/NEJMoa066603. [DOI] [PubMed] [Google Scholar]
- 149.Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 150.Dixon AF, Dixon JB, O’Brien PE. Laparoscopic adjustable gastric banding induces prolonged satiety: a randomized blind crossover study. J Clin Endocrinol Metab. 2005;90:813–9. doi: 10.1210/jc.2004-1546. [DOI] [PubMed] [Google Scholar]
- 151.Kenler HA, Brolin RE, Cody RP. Changes in eating behavior after horizontal gastroplasty and Roux-en-Y gastric bypass. Am J Clin Nutr. 1990;52:87–92. doi: 10.1093/ajcn/52.1.87. [DOI] [PubMed] [Google Scholar]
- 152.Chan JL, Heist K, DePaoli AM, Veldhuis JD, Mantzoros CS. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest. 2003;111:1409–21. doi: 10.1172/JCI17490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85. doi: 10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- 154.Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76. doi: 10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.IDF position statment. International Diabetes Federation; 2011. Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes. [Google Scholar]
- 156.Kellum JM, Kuemmerle JF, O’Dorisio TM, Rayford P, Martin D, Engle K, et al. Gastrointestinal hormone responses to meals before and after gastric bypass and vertical banded gastroplasty. Ann Surg. 1990;211:763–70. doi: 10.1097/00000658-199006000-00016. discussion 770–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.le Roux CW, Aylwin SJ, Batterham RL, Borg CM, Coyle F, Prasad V, et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. AnnSurg. 2006;243:108–14. doi: 10.1097/01.sla.0000183349.16877.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246:780–5. doi: 10.1097/SLA.0b013e3180caa3e3. [DOI] [PubMed] [Google Scholar]
- 159.le Roux CW, Borg C, Wallis K, Vincent RP, Bueter M, Goodlad R, et al. Gut hypertrophy after gastric bypass is associated with increased glucagon-like peptide 2 and intestinal crypt cell proliferation. Ann Surg. 2010;252:50–6. doi: 10.1097/SLA.0b013e3181d3d21f. [DOI] [PubMed] [Google Scholar]
- 160.Chambers AP, Jessen L, Ryan KK, Sisley S, Wilson-Pérez HE, Stefater MA, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141:950–8. doi: 10.1053/j.gastro.2011.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Neary NM, Small CJ, Druce MR, Park AJ, Ellis SM, Semjonous NM, et al. Peptide YY3-36 and glucagon-like peptide-17-36 inhibit food intake additively 2. Endocrinology. 2005;146:5120–7. doi: 10.1210/en.2005-0237. [DOI] [PubMed] [Google Scholar]
- 162.Field BC, Wren AM, Peters V, Baynes KC, Martin NM, Patterson M, et al. PYY3-36 and oxyntomodulin can be additive in their effect on food intake in overweight and obese humans. Diabetes. 2010;59:1635–9. doi: 10.2337/db09-1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Daugaard JR, Meier E, Riber D, Bæk CÆ, Larsen KS. The new dual Glucagon-GLP-1 Agonist ZP2929 improves glycemic control and reduces body weight in murine models of obesity and type 2 Diabetes. Poster at ADA; Orlando: Jun, 2010. [Google Scholar]
- 164.Chu ZL, Jones RM, He H, Carroll C, Gutierrez V, Lucman A, et al. A role for beta-cell-expressed G protein-coupled receptor 119 in glycemic control by enhancing glucose-dependent insulin release. Endocrinology. 2007;148:2601–9. doi: 10.1210/en.2006-1608. [DOI] [PubMed] [Google Scholar]
- 165.Overton HA, Babbs AJ, Doel SM, Fyfe MC, Gardner LS, Griffin G, et al. Deorphanization of a G protein-coupled receptor for oleoylethanolamide and its use in the discovery of small-molecule hypophagic agents. Cell Metab. 2006;3:167–75. doi: 10.1016/j.cmet.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 166.Jones RM, Leonard JN, Buzard DJ, Lehmann J. GPR119 agonists for the treatment of type 2 diabetes. Expert Opin Ther Pat. 2009;19:1339–59. doi: 10.1517/13543770903153878. [DOI] [PubMed] [Google Scholar]
- 167.Shah U, Kowalski TJ. GPR119 agonists for the potential treatment of type 2 diabetes and related metabolic disorders. Vitam Horm. 2010;84:415–48. doi: 10.1016/B978-0-12-381517-0.00016-3. [DOI] [PubMed] [Google Scholar]