Abstract
The aim of this study was to compare the intraoperative difference in anatomic details between loupe-assisted and microscopic varicocelectomy within the same spermatic cord. Between April 2011 and August 2011, 26 men with 33 sides containing grade 2-3 varicocele were enrolled in this study. First, one surgeon performed the open inguinal varicocelectomy under × 3.5 loupe magnification. The presumed vascular channels and lymphatics were isolated and marked without ligation. Another surgeon then microsurgically dissected and checked the same spermatic cord using an operating microscope to judge the results in terms of the ligation of the internal spermatic veins and the preservation of the arteries and lymphatics. There were significant differences in the average number of internal spermatic arteries (1.51 vs 0.97), internal spermatic veins (5.70 vs 4.39) and lymphatics (3.52 vs 1.61) between the microscope and loupe-assisted procedures (P < 0.001, P < 0.001, P < 0.001, respectively). Meanwhile, in varicocele repair with loupe magnification, an average of 1.30 ± 1.07 (43/33) internal spermatic veins per side were missed, among the overlooked veins, 1.12 ± 0.93 (37/33) were adhered to the preserved testicular artery, as well as 0.55 ± 0.79 lymphatics and 0.36 ± 0.55 arteries that were to be ligated. In conclusion, microscopic varicocelectomy could preserve more internal spermatic arteries and lymphatics and could ligate more veins than the loupe-assisted procedure. To some degree, loupe magnification is inadequate for the reliable identification and dissection of the tiny vessels of the spermatic cord, as most of the overlooked veins were adhered to the preserved testicular artery.
Keywords: intraoperative difference, loupe-assisted, microscopic, varicocelectomy
INTRODUCTION
Even in the era of intracytoplasmic sperm injection, varicocelectomy still plays an important role in treating infertile men with palpable varicocele and impaired semen quality.1,2 The effectiveness of varicocele repair in the improvement or resolution of testicular pain is also exciting.3
There is a variety of treatment options for varicocele.4 Many experts perform inguinal or subinguinal varicocele repair by employing loupes or an operating microscope for the preservation of arterial and lymphatic vessels, while reducing the risk of persistence or recurrence the varicocele.5,6,7 Several studies reported that microscopic varicocelectomy was superior to loupe-assisted varicocele repair.8,9 Unfortunately, these studies focused on the postoperative ‘outcome’, but not the intraoperative anatomic difference. To investigate and quantify this difference between the microscope and loupe-assisted procedures, first, we mimicked ‘loupe-assisted inguinal varicocelectomy’ by identifying, dissecting and marking but not ligating the vessels; then, we microsurgically checked, dissected and analyzed the ‘results’ in the same spermatic cord with an operating microscope.
MATERIALS AND METHODS
Patients
Between April 2011 and August 2011, 26 men with 33 sides containing grade 2-3 varicoceles were enrolled in this study. Of these patients, 19 had a unilateral varicocele (left) and seven had bilateral varicoceles; patients with a grade 1 or subclinical varicocele and a recurrent varicocele were excluded. Among the patients, 14 (53.8%) had scrotal pain, 11 (42.3%) had infertility and 1 (3.9%) had both conditions. The average age was 28.9 years (ranging from 16 to 37 years). Preoperative evaluation of the patients who had infertility consisted of testicular volume, serum testosterone and follicle-stimulating hormone (FSH) determinations and at least three semen analyses. The research protocol was approved by the ethics committee of our hospital, and all patients provided written informed consent.
Technique
The surgical techniques (loupe-assisted and microscopic) have been described previously with our modification.6,10 Briefly, an approximately 2 cm incision over the inguinal canal between the external and internal inguinal ring was made. Next, the external oblique aponeurosis was opened, and the spermatic cord was identified, encircled with a Babcock clamp and then placed over a Penrose drain without delivery of the testis. The internal spermatic vessels were progressively exposed. One surgeon (Xiao-Peng Liu) first performed the open inguinal varicocelectomy under × 3.5 loupe magnification (GSX-II, Tianjin Medical Optical Instrument Factory, China); the presumed vascular channels and lymphatics were isolated and marked but not ligated (Figure 1). Next, a Zeiss (Carl Zeiss, D-73466 Oberkochen, Germany) or Leica (Leica MS2, CH -9435 Heerbrugg, Switzerland) operating microscope was brought into the operative field. Another surgeon (Yan Zhang) performed a full microsurgical dissection at the same spermatic cord with the operating microscope under × 8 to × 15 magnification to check and judge the results in terms of the ligation of the internal spermatic veins and the preservation of the arteries and lymphatics (Figure 2). The testicular artery (ies) was confirmed by visualization of a clear pulsatile movement, with loupe or microscope magnification and sometimes with the use of papverine. Lastly, all of the internal spermatic and cremasteric veins were microsurgically ligated.
Figure 1.
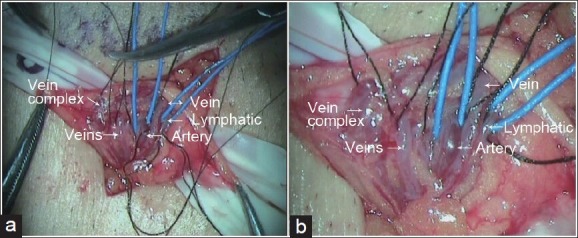
Results in loupe-assisted and microscopic procedures. The presumed internal spermatic veins, lymphatics and arteries were marked and circled; (a) shows the loupe-assisted field (photo through Leica operating microscope (× 1.25); the surgeon did not use this microscope but used a × 3.5 loupe to facilitate the operation) and (b) shows the same field under an operating microscope (×8)
Figure 2.
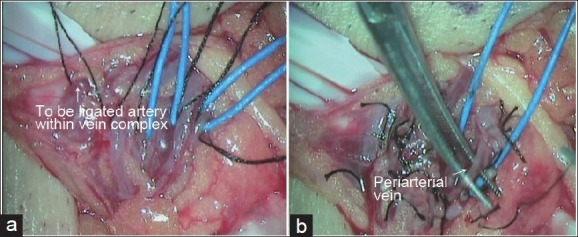
(a) Shows the artery to be ligated within the vein complex using the ocular loupe magnification procedure and (b) shows the missed periarterial veins following the loupe-assisted procedure
Statistical analysis
The number of veins, arteries and lymphatics found using the loupe-assisted and microscopic procedures were compared using a standard chi-square test. P < 0.05 was considered to indicate a significant difference between two groups.
RESULTS
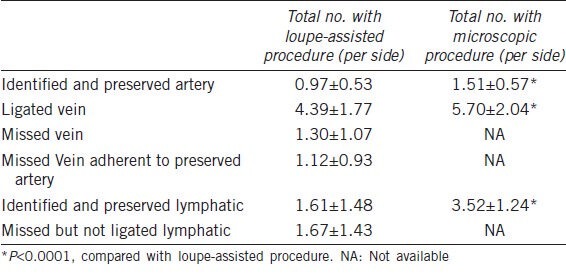
There were significant differences in the average number of internal spermatic arteries (1.51 vs 0.97), internal spermatic veins (5.70 vs 4.39) and lymphatics (3.52 vs 1.61) between microscope and loupe-assisted procedures (P < 0.001, P < 0.001, P < 0.001, respectively). Meanwhile, in varicocele repair with loupe magnification, an average of 1.30 ± 1.07 (43/33) internal spermatic veins per side were missed; among the overlooked veins, 1.12 ± 0.93 (37/33) were adherent to the preserved testicular artery, and 0.55 ± 0.79 lymphatics and 0.36 ± 0.55 arteries were to be ligated. A total of six internal spermatic arteries and an average number of 1.67 ± 1.43 lymphatics were neither identified nor ligated in varicocelectomy using the magnifying loupe. Additionally, in one case, the vasal vessels were to be ligated using this approach (Table 1).
Table 1.
Intraoperative anatomical difference between microscopic and loupe-assisted varicocelectomy
DISCUSSION
An ideal varicocelectomy procedure should have optimal results with minimal complications, such as varicocele recurrence or persistence, hydrocele formation and testicular artery injury.6
The most common cause of persistent or recurrent varicocele is through the internal spermatic veins.11 Recurrent varicocele was 8% and 14.9%, respectively, in adult patients after an inguinal or a subinguinal approach using a magnifying loupe.9 In a comparative study, the postoperative recurrence rates were 0%, 2.9% and 8.8% in microsurgical, loupe-assisted and macroscopic varicocelectomy, respectively. In our study, approximately 22.9% (43/188) of spermatic veins were missed in varicocelectomy using a magnifying loupe and 19.7% (37/188) were adherent to the testicular artery; this accounted for 86.0% (37/43) of the total missed veins. Our previous investigation showed that 33.2% (90/271) of spermatic veins were overlooked in non-magnified varicocelectomy; 68.9% (62/90) of the missed veins were adherent to the testicular artery.10 Although there is some debate as to the significance of small venules adherent to the artery. We routinely ligated them as Goldstein described.
Hydrocele was reported due to the ligation of the lymphatics and is associated with reduced testicular function.12,13,14 In this study, 14.3% (18/126) of lymphatics were to be ligated for incorrect identification in our ‘loupe-assisted varicocelectomy’. Although Amelar7 expressed confidence using a × 4 to × 6 ocular loupe for varicocele repair, the 3% hydrocele rate is higher than the microscopic procedure, which is no higher than 1%.15
Whether the testicular arteries should be preserved during the surgical repair of varicocele is still controversial.16,17,18 There are several reasons why we routinely preserve the testicular arteries using an operating microscope in clinical practice. First, several investigators who have argued that ligation of the testicular artery during varicocele repair did not induce testicular atrophy have never demonstrated that preservation of the testicular arteries can impair spermatogenesis. On the contrary, doctors who confirmed the value of the preservation of the testicular arteries have simultaneously proven that ligation of the testicular artery can damage testicular function. Second, some patients may be candidates for vasectomy or vasovasostomy (vasoepididymostomy). If the internal spermatic artery has been inadvertently ligated in varicocelectomy, the intraoperative injury of the deferential artery may cause testicular atrophy. The incidence of accidental testicular artery ligation in microsurgical varicocelectomy was approximately 1%,19 and in the loupe magnification (×2.5) procedure, the incidence is approximately 12%, even with help of intraoperative Doppler.20 In adult varicocelectomy research using a magnifying loupe (×3.5), inadvertent injury of the spermatic artery that could not be identified occurred in eight of 47 (17%) subinguinal and four of 50 (8%) inguinal dissections.9 In subinguinal varicocele repair for the treatment of prepubertal and pubertal patients; Silveri et al.21 reported that in approximately 26% (12/46) of cases, they were unable to easily identify arteries by loupe magnification (×3), and thus, had to use the microscopic procedure. Injury of the spermatic artery remains 24% (12/50) in the loupe-assisted procedure according to our results, and it was 45.7% (32/70) using traditional open surgery.10
In our study, different surgeons performed different procedures independently to avoid a subjective preference and biased results in the end. We also admitted the methodological bias because that the microsurgical technique was always performed after the loupe approach, so we could not report fewer vessels including arteries, veins or lymphatics due to the order. We found that the average number of internal spermatic arteries is 1.51 per side, which is similar to the results of Beck et al.22,23,24 (the average number, 1.4–1.6), but different from the study by Jarow et al.25 (the average number, 2). Further studies with large sample are needed to elucidate the difference.
The internal spermatic veins in our study varied from several reported results,22,23,26 which is possibly due to our higher level of dissection in inguinal approach compared to Goldstein.22 Another possible explanation of the differences between those findings and our study is that they used a subinguinal incision.27 Intraoperative Doppler ultrasound evaluation would be more convincing,23,25 although we did not use this technique in China. The other limitation of our study may be that there were no matched series of loupe-assisted varicocelectomies to compare the clinical outcome. It is difficult to persuade some patients to accept the loupe-assisted technique without portraying it as a more ‘advanced’ microscopic varicocelectomy technique.
CONCLUSIONS
Loupe magnification is very useful in open varicocele repair. However, microscopic varicocelectomy can preserve more internal spermatic arteries and lymphatics and ligate more veins than the loupe-assisted procedure. To some degree, loupe magnification is inadequate for the reliable identification and dissection of the tiny vessels of the spermatic cord, as most of the overlooked veins are adhered to the preserved testicular artery.
AUTHOR CONTRIBUTIONS
YZ, HZ and XPL were responsible for the concept and framework of the paper. HZ, XJY, WTH, HJX and LYL participated in collecting the data. XXR and HZ participated in evaluating the data. YZ and HZ were responsible for the artwork. YZ wrote the paper. YZ, HZ, XPL and LYL were responsible for the final editing. XG supervised the study. All the authors read and approved the final manuscript.
COMPETING INTERESTS
The authors declare that they have no competing interests.
ACKNOWLEDGMENTS
This work was partially supported by the National Natural Science Foundation of China (No. 30972996) and Guangdong Province Science and Technology Project (No. 2011B061300007).
REFERENCES
- 1.American Urological Association. Report on Varicocele and Infertility (2001) (Reviewed and validity confirmed 2012) [Last accessed on 2013 Nov 10]. Available from: http://www.auanet.org/common/pdf/education/clinical-guidance/Varicocele-Archive.pdf .
- 2.Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, et al. European Association of Urology guidelines on Male Infertility: the 2012 update. Eur Urol. 2012;62:324–32. doi: 10.1016/j.eururo.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 3.Shridharani A, Lockwood G, Sandlow J. Varicocelectomy in the treatment of testicular pain: a review. Curr Opin Urol. 2012;22:499–506. doi: 10.1097/MOU.0b013e328358f69f. [DOI] [PubMed] [Google Scholar]
- 4.Cayan S, Shavakhabov S, Kadioğlu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 5.Marmar JL, DeBenedictis TJ, Praiss D. The management of varicoceles by microdissection of the spermatic cord at the external inguinal ring. Fertil Steril. 1985;43:583–8. doi: 10.1016/s0015-0282(16)48501-8. [DOI] [PubMed] [Google Scholar]
- 6.Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol. 1992;148:1808–11. doi: 10.1016/s0022-5347(17)37035-0. [DOI] [PubMed] [Google Scholar]
- 7.Amelar RD. Early and late complications of inguinal varicocelectomy. J Urol. 2003;170(2 Pt 1):366–9. doi: 10.1097/01.ju.0000074975.79734.17. [DOI] [PubMed] [Google Scholar]
- 8.Cayan S, Acar D, Ulger S, Akbay E. Adolescent varicocele repair: long-term results and comparison of surgical techniques according to optical magnification use in 100 cases at a single university hospital. J Urol. 2005;174:2003–6. doi: 10.1097/01.ju.0000176488.44895.7b. [DOI] [PubMed] [Google Scholar]
- 9.Gontero P, Pretti G, Fontana F, Zitella A, Marchioro G, et al. Inguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia: which technique is preferable in clinical practice? Urology. 2005;66:1075–9. doi: 10.1016/j.urology.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Liu X, Zhang H, Ruan X, Xiao H, Huang W, et al. Macroscopic and microsurgical varicocelectomy: what's the intraoperative difference? World J Urol. 2013;31:603–8. doi: 10.1007/s00345-012-0950-x. [DOI] [PubMed] [Google Scholar]
- 11.Murray RR, Jr, Mitchell SE, Kadir S, Kaufman SL, Chang R, et al. Comparison of recurrent varicocele anatomy following surgery and percutaneous balloon occlusion. J Urol. 1986;135:286–9. doi: 10.1016/s0022-5347(17)45615-1. [DOI] [PubMed] [Google Scholar]
- 12.Szabo R, Kessler R. Hydrocele following internal spermatic vein ligation: a retrospective study and review of the literature. J Urol. 1984;132:924–5. doi: 10.1016/s0022-5347(17)49950-2. [DOI] [PubMed] [Google Scholar]
- 13.Kocvara R, Dolezal J, Hampl R, Povýsil C, Dvorácek J, et al. Division of lymphatic vessels at varicocelectomy leads to testicular oedema and decline in testicular function according to the LH-RH analogue stimulation test. Eur Urol. 2003;43:430–5. doi: 10.1016/s0302-2838(03)00051-4. [DOI] [PubMed] [Google Scholar]
- 14.Schwentner C, Radmayr C, Lunacek A, Gozzi C, Pinggera GM, et al. Laparoscopic varicocele ligation in children and adolescents using isosulphan blue: a prospective randomized trial. BJU Int. 2006;98:861–5. doi: 10.1111/j.1464-410X.2006.06428.x. [DOI] [PubMed] [Google Scholar]
- 15.Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, et al. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011;108:1157–72. doi: 10.1111/j.1464-410X.2010.09959.x. [DOI] [PubMed] [Google Scholar]
- 16.Riccabona M, Oswald J, Koen M, Lusuardi L, Radmayr C, et al. Optimizing the operative treatment of boys with varicocele: sequential comparison of 4 techniques. J Urol. 2003;169:666–8. doi: 10.1097/01.ju.0000047086.34953.82. [DOI] [PubMed] [Google Scholar]
- 17.Zheng YQ, Zhang XB, Zhou JQ, Cheng F, Rao T, et al. The effects of artery-ligating and artery-preserving varicocelectomy on the ipsilateral testes in rats. Urology. 2008;72:1179–84. doi: 10.1016/j.urology.2008.03.035. [DOI] [PubMed] [Google Scholar]
- 18.Zampieri N, Zuin V, Corroppolo M, Chironi C, Cervellione RM, et al. Varicocele and Adolescents: semen Quality after 2 Different Laparoscopic Procedures. J Androl. 2007;28:727–33. doi: 10.2164/jandrol.107.002600. [DOI] [PubMed] [Google Scholar]
- 19.Chan PT, Wright EJ, Goldstein M. Incidence and postoperative outcomes of accidental ligation of the testicular artery during microsurgical varicocelectomy. J Urol. 2005;173:482–4. doi: 10.1097/01.ju.0000148942.61914.2e. [DOI] [PubMed] [Google Scholar]
- 20.Cuda SP, Musser JE, Belnap CM, Thibault GP. Incidence and clinical significance of arterial injury in varicocele repair. BJU Int. 2011;107:1635–7. doi: 10.1111/j.1464-410X.2010.09643.x. [DOI] [PubMed] [Google Scholar]
- 21.Silveri M, Adorisio O, Pane A, Colajacomo M, De Gennaro M. Subinguinal microsurgical ligation--its effectiveness in pediatric and adolescent varicocele. Scand J Urol Nephrol. 2003;37:53–4. doi: 10.1080/00365590310008703. [DOI] [PubMed] [Google Scholar]
- 22.Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992;148:1190–4. doi: 10.1016/s0022-5347(17)36857-x. [DOI] [PubMed] [Google Scholar]
- 23.Cocuzza M, Pagani R, Coelho R, Srougi M, Hallak J. The systematic use of intraoperative vascular Doppler ultrasound during microsurgical subinguinal varicocelectomy improves precise identification and preservation of testicular blood supply. Fertil Steril. 2010;93:2396–9. doi: 10.1016/j.fertnstert.2009.01.088. [DOI] [PubMed] [Google Scholar]
- 24.Wang XK, Wang HZ, Fu DJ, Lai MK. Microanatomy of the spermatic cords during microsurgical inguinal varicocelectomy: initial experience in Asian men. Asian J Androl. 2012;14:897–9. doi: 10.1038/aja.2012.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jarow JP, Ogle A, Kaspar J, Hopkins M. Testicular artery ramification within the inguinal canal. J Urol. 1992;147:1290–2. doi: 10.1016/s0022-5347(17)37545-6. [DOI] [PubMed] [Google Scholar]
- 26.Mirilas P, Mentessidou A. Microsurgical subinguinal varicocelectomy in children, adolescents, and adults: surgical anatomy and anatomically justified technique. J Androl. 2012;33:338–49. doi: 10.2164/jandrol.111.013052. [DOI] [PubMed] [Google Scholar]
- 27.Hopps CV, Lemer ML, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a microscopic study of the inguinal versus subinguinal approach. J Urol. 2003;170(6 Pt 1):2366–70. doi: 10.1097/01.ju.0000097400.67715.f8. [DOI] [PubMed] [Google Scholar]


