Abstract
BACKGROUND:
Laparoscopic liver surgery is now an established practice in many institutions. It is a safe and feasible approach in experienced hands. Single incision laparoscopic surgery (SILS) has been performed for cholecystectomies, nephrectomies, splenectomies and obesity surgery. However, the use of SILS in liver surgery has been rarely reported. We report our initial experience in seven patients on single incision laparoscopic hepatectomy (SILH).
PATIENTS AND METHODS:
From October 2010 to September 2012, seven patients underwent single-incision laparoscopic liver surgery. The abdomen was approached through a 25 mm periumbilical incision. No supplemental ports were required. The liver was transected using a combination of LigaSure™ (Covidien-Valleylab. Boulder. USA), Harmonic Scalpel and Ligaclips (Ethicon Endo-Surgery, Inc.).
RESULTS:
Liver resection was successfully completed for the seven patients. The procedures consisted of two partial resections of segment three, two partial resections of segment five and three partial resections of segment six. The mean operative time was 98.3 min (range: 60-150 min) and the mean estimated blood loss was 57 ml (range: 25-150 ml). The postoperative courses were uneventful and the mean hospital stay was 5.1 days (range: 1-13 days). Pathology identified three benign and four malignant liver tumours with clear margins.
CONCLUSION:
SILH is a technically feasible and safe approach for wedge resections of the liver without oncological compromise and with favourable cosmetic results. This surgical technique requires relatively advanced laparoscopic skills. Further studies are needed to determine the potential advantages of this technique, apart from the better cosmetic result, compared to the conventional laparoscopic approach.
Keywords: Hepatectomy, laparoscopic liver resection, single incision laparoscopic hepatectomy (SILH), single incision laparoscopic surgery (SILS)
INTRODUCTION
Laparoscopic liver surgery is now widely practised in many institutions worldwide. In accordance with the Louisville statement the best indications are for solitary lesions 5 cm or less located in the periphery of the liver and laparoscopic left lateral lobectomy should be considered the standard of care.[1] The advantages of shorter hospital stay, decreased blood loss as well as the attainment of disease free and overall survival comparable to open liver resections in laparoscopic liver surgery has been well documented.[2] The natural progress to minimise incisions has seen the development of single incision laparoscopic surgery (SILS) in a number of surgical subspecialties.[3,4,5,6]
The use of SILS in single incision laparoscopic hepatectomy (SILH) is still in the early stages of development and little has been published on the matter. SILS and its derivative SILH pose a technical challenge to the surgeon due to the acute angle of triangulation and difficulty of manipulation. In contrast, the potential advantage of better cosmesis and shorter hospital stay makes it attractive in a select group of patients. This advantage must not be at the sacrifice of maintaining oncological principles and low morbidity and mortality rates. We describe here our initial experience with SILH with particular reference to morbidity, oncological clearance, advantages and challenges.
PATIENTS AND METHODS
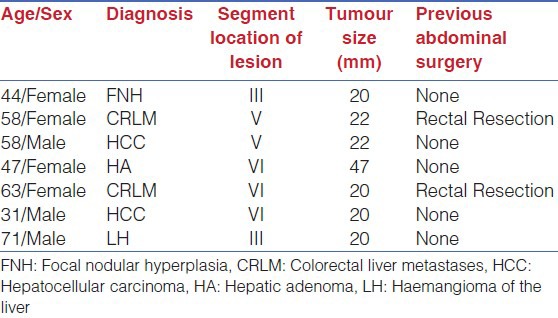
From October 2010 to September 2012, seven patients were selected by a consensus of senior surgeons to undergo SILH in our unit. These patients were otherwise considered suitable for laparoscopic liver resection. All patients had superficial lesions. Patient demographics, clinical history, preoperative diagnosis, laboratory examinations, radiological images, operating time, blood loss, hospital stay and histopathological results were reviewed from a prospective database. The patients’ preoperative demographics are listed in Table 1.
Table 1.
Demographics of seven patients who had single port liver resection for isolated liver lesions
Surgical Technique
Preoperative assessment and anaesthesia was routine as for all liver resections in our department. The patients were placed in the supine position with 20° reverse Trendelenberg position which is standard for all laparoscopic liver surgery at our institution. A 25 mm periumbilical skin incision was made and either a SILSPORT (Covidien-Valleylab. Boulder. USA.) or a Gelpoint (Applied Medical. Rancho Santa Margarita, CA. USA) was inserted under direct vision after breaching the peritoneal cavity. A pneumoperitoneum to 12 mmHg was created using carbon dioxide via the insufflation port on the SILSPORT system. The SILSPORT system has three 5 mm operating ports. One port was used to introduce a 5 mm 30° laparoscope (Karl Storz, Tuttlingen, Germany) and the two other 5 mm ports were used as the working ports to introduce various instruments during the procedure. In one patient a high definition (HD) flexible tip laparoscope (Olympus, Center Valley, PA, USA) was used. The transection line was marked on the liver surface with bipolar and liver parenchymal transection was done with Harmonic Scalpel (Ethicon Endo-Surgery, Inc.) and LigaSure (Covidien-Valleylab, Boulder, USA). Haemostasis was achieved with LigaSure, bipolar forceps and Ligaclips (Ethicon Endo-Surgery, Inc.). No Pringle manoeuvre was necessary. No additional ports were needed for any of the procedures.
Haemostasis was secured after the transection. The specimen was then retrieved in an endoscopic bag (Memo Bag, Teleflex medical, Park, Athlone, Ireland) and extracted from the abdomen via the umbilical port. In two patients who each had a concurrent cholecystectomy, a 10 Fr drain was inserted. After checking for haemostasis and biliary leak, the incision was closed with number 1 polydioxanone suture (PDS) (Ethicon Inc.) to the rectus sheath and a subcuticular 3/0 undyed monocryl (Ethicon Inc.) to the skin. Postoperatively, all patients were admitted to the ward.
RESULTS
There were four males and three females in our case series with a median age of 58 years (range: 31-71 years). All seven patients had peripheral lesions demonstrated on preoperative imaging and underwent non-anatomical resections. Three lesions were located in segment VI and two lesions were located in segment III and V each. Two of the seven patients had previous abdominal surgery for resection of colorectal cancer. Successful resection of the hepatic lesion via the SILSPORT was achieved in all patients without the need for the insertion of additional ports or conversion to an open procedure in any of the cases. Three of the patients had resections for a preoperative diagnosis of suspicious lesions on imaging which were histologically reported as adenomas. Four patients had resections for malignancy, including two each for hepatocellular cancer (HCC) with underlying cirrhosis and metastatic colorectal cancer (CRLM). The two patients with HCC each had a Child-Pugh score of A and early B. One patient had a synchronous resection of a colorectal liver metastasis via SILH and a pulmonary wedge resection via a thoracotomy for a lung metastasis. The median operating time was 110 minutes (range: 60-150 minutes). Median blood loss was 50 ml (range: 25-150 ml). The median size of the resected lesion was 20 mm (range: 20-47 mm). All operative margins were clear with a median resection margin of 2.5 mm (range: 2-8 mm) [Table 2]. In the two patients who had drains inserted at the time of the operation, these were removed on postoperative day 2.
Table 2.
Operative details with postoperative hospital stay and histological margins
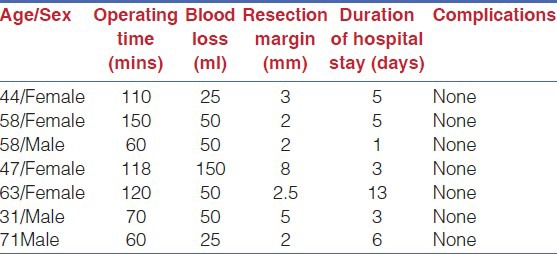
Postoperatively all patients had uncomplicated recoveries with a median hospital stay of 5 days (range: 1-13 days). Normal diet was resumed on the day of surgery. The patient who had synchronous pulmonary and liver resection had the longest hospital stay of 13 days. This delayed discharge was a result of the decision made by the thoracic surgeons who performed the pulmonary resection and not due to any complication of the hepatic resection. Excluding this patient, all other patients had a hospital stay of 6 days or less.
DISCUSSION
Laparoscopic liver surgery is now the mainstay of left lateral lobectomy and peripherally located lesions in many centres.[7] In addition, in experienced hands laparoscopic major hepatectomies have been shown to be feasible and safe with good oncological resection margins.[8,9,10] Laparoscopic hepatectomy has demonstrated a decreased hospital stay,[11] less blood loss[12] with mortality, morbidity and oncological outcomes comparable to that of open resections.[2] Recent interest in “scarless” surgery and the theoretical advantage of better preservation of collateral veins on the anterior abdominal wall in patients with underlying liver disease has seen some centres develop an interest in SILS.[13,14,15] In addition, in laparoscopic wedge resections of the liver one of the trocar sites usually needs to be enlarged to extract the specimen. The advantage of SILH in this setting is the ability to perform the same resection through the same size incision as that which would be necessary for specimen extraction without the need for an additional three or four ports. This, in theory, makes the procedure less invasive in these circumstances. Our outcome data appears to be comparable with other published literature on SILH.[16,17] In addition, the results are also comparable to published data on conventional laparoscopic minor hepatectomies (≤2 Couinaud segments)[18,19] supporting the view that SILH is as safe and as feasible as conventional laparoscopic liver resection.[20] In contrast, both Tan et al.[17] and Aldrighetti et al.[21] have reported on the use of SILS in left lateral lobectomies. In both their publications the blood loss was greater than in our case series. This is possibly due to the fact that the resection is larger and a number of patients had surgery for hepatocellular carcinoma (with the possibly attendant underlying cirrhosis). However, the case-matched study by Aldrighetti et al. suggests that there is no difference in outcome between SILH and conventional laparoscopic surgical resection of the left lateral lobe.
In SILH (laparoscopic liver surgery with SILS), cosmesis may have to be a compromise as the port site scar is not truly well hidden if it is above umbilicus. However, this technique does minimise the number of ports. In addition, for hepatectomies, the use of SILS has highlighted some technical challenges. These include the lack of adequate triangulation with difficulty in manipulation of the instruments and a parallel field of vision.[16] To overcome this, Tan et al. described a natural evolution in their technique for laparoendoscopic single site surgery in which they used longer bariatric instruments to compensate for overcrowding.[17] In our series we used standard laparoscopic instruments for all procedures and we concur that there are issues with overcrowding and lack of manipulative capabilities. The use of curved and articulating instruments as well as flexible endoscopes have helped to overcome some of these problems.[22,23]
Our series demonstrates that SILH is a safe, feasible and oncologically acceptable technique for liver resection with results comparable to standard laparoscopic liver resection in published series. However, patient selection is of paramount importance and we think that the Louisville statement should be adopted for SILH. Although others have reported SILH for left lateral lobectomy,[17,24] we think that in the learning phase SILH should only be attempted by experienced laparoscopic liver surgeons on tumours ≤5 cm located on the periphery of the liver.
Although cosmetic and postoperative recovery advantages of SILS in colorectal surgery has been reported,[25] it remains to be seen if this holds true for SILH. Continued development of laparoscopic instruments for SILS to improve manipulation will likely see further progress in this technique. In conclusion, SILH appears safe and feasible. Larger studies are needed, in particular, a randomised study comparing it to conventional laparoscopic techniques to demonstrate any potential advantages.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, et al. World Consensus Conference on Laparoscopic Surgery. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009;250:825–30. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831–41. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- 3.Aminsharifi AR, Goshtasbi B, Afsar F. Laparoendoscopic single-site nephrectomy using standard laparoscopic instruments: Our initial experience. Urol J. 2012;9:657–61. [PubMed] [Google Scholar]
- 4.Garg PK. Single incision laparoscopic cholecystectomy: Great start and a long way to go. J Minim Access Surg. 2012;8:163. doi: 10.4103/0972-9941.103133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palanivelu C, Vij A, Rajapandian S, Palanivelu P, Parthasarathi R, Vaithiswaran V, et al. Single incision laparoscopic colorectal resection: Our experience. J Minim Access Surg. 2012;8:134–9. doi: 10.4103/0972-9941.103118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raj PP, Senthilnathan P, Palanivelu C. Single port access sleeve is reasonable if done without any violation of basic principles. J Minim Access Surg. 2012;8:163–4. doi: 10.4103/0972-9941.103134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azagra JS, Goergen M, Brondello S, Calmes MO, Philippe P, Schmitz B. Laparoscopic liver sectionectomy 2 and 3 (LLS 2 and 3): Towards the “gold standard”. J Hepatobiliary Pancreat Surg. 2009;16:422–6. doi: 10.1007/s00534-009-0117-3. [DOI] [PubMed] [Google Scholar]
- 8.Gayet B, Cavaliere D, Vibert E, Perniceni T, Levard H, Denet C, et al. Totally laparoscopic right hepatectomy. Am J Surg. 2007;194:685–9. doi: 10.1016/j.amjsurg.2006.11.044. [DOI] [PubMed] [Google Scholar]
- 9.Huscher CG, Lirici MM, Chiodini S, Recher A. Current position of advanced laparoscopic surgery of the liver. J R Coll Surg Edinb. 1997;42:219–25. [PubMed] [Google Scholar]
- 10.O’Rourke N, Fielding G. Laparoscopic right hepatectomy: Surgical technique. J Gastrointest Surg. 2004;8:213–6. doi: 10.1016/j.gassur.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Cai XJ, Yang J, Yu H, Liang X, Wang YF, Zhu ZY, et al. Clinical study of laparoscopic versus open hepatectomy for malignant liver tumors. Surg Endosc. 2008;22:2350–6. doi: 10.1007/s00464-008-9789-z. [DOI] [PubMed] [Google Scholar]
- 12.Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F. Laparoscopic versus open liver resection of hepatic neoplasms: Comparative analysis of short-term results. Surg Endosc. 2008;22:2208–13. doi: 10.1007/s00464-008-0023-9. [DOI] [PubMed] [Google Scholar]
- 13.Chang SK, Tay CW, Bicol RA, Lee YY, Madhavan K. A case-control study of single-incision versus standard laparoscopic cholecystectomy. World J Surg. 2011;35:289–93. doi: 10.1007/s00268-010-0842-4. [DOI] [PubMed] [Google Scholar]
- 14.Seo IY, Lee JW, Rim JS. Laparoendoscopic single-site radical nephrectomy: A comparison with conventional laparoscopy. J Endourol. 2011;25:465–9. doi: 10.1089/end.2010.0465. [DOI] [PubMed] [Google Scholar]
- 15.Teoh AY, Chiu PW, Wong TC, Wong SK, Lai PB, Ng EK. A case-controlled comparison of single-site access versus conventional three-port laparoscopic appendectomy. Surg Endosc. 2011;25:1415–9. doi: 10.1007/s00464-010-1406-2. [DOI] [PubMed] [Google Scholar]
- 16.Pan M, Jiang Z, Cheng Y, Xu X, Zhang Z, Zhou C, et al. Single-incision laparoscopic hepatectomy for benign and malignant hepatopathy: Initial experience in 8 chinese patients. Surg Innov. 2012;19:446–51. doi: 10.1177/1553350612438412. [DOI] [PubMed] [Google Scholar]
- 17.Tan EK, Lee VT, Chang SK, Ganpathi IS, Madhavan K, Lomanto D. Laparoendoscopic single-site minor hepatectomy for liver tumors. Surg Endosc. 2012;26:2086–91. doi: 10.1007/s00464-011-2128-9. [DOI] [PubMed] [Google Scholar]
- 18.Tsinberg M, Tellioglu G, Simpfendorfer CH, Walsh RM, Vogt D, Fung J, et al. Comparison of laparoscopic versus open liver tumor resection: A case-controlled study. Surg Endosc. 2009;23:847–53. doi: 10.1007/s00464-008-0262-9. [DOI] [PubMed] [Google Scholar]
- 19.Gumbs AA, Tsai TJ, Hoffman JP. Initial experience with laparoscopic hepatic resection at a comprehensive cancer center. Surg Endosc. 2012;26:480–7. doi: 10.1007/s00464-011-1904-x. [DOI] [PubMed] [Google Scholar]
- 20.Gaujoux S, Kingham TP, Jarnagin WR, D’Angelica MI, Allen PJ, Fong Y. Single-incision laparoscopic liver resection. Surg Endosc. 2011;25:1489–94. doi: 10.1007/s00464-010-1419-x. [DOI] [PubMed] [Google Scholar]
- 21.Aldrighetti L, Ratti F, Catena M, Pulitano C, Ferla F, Cipriani F, et al. Laparoendoscopic single site (LESS) surgery for left-lateral hepatic sectionectomy as an alternative to traditional laparoscopy: Case-matched analysis from a single center. Surg Endosc. 2012;26:2016–22. doi: 10.1007/s00464-012-2147-1. [DOI] [PubMed] [Google Scholar]
- 22.Abe N, Takeuchi H, Ohki A, Aoki H, Masaki T, Mori T, et al. Single-incision multiport laparoendoscopic surgery using a newly developed short-type flexible endoscope: A combined procedure of flexible endoscopic and laparoscopic surgery. J Hepatobiliary Pancreat Sci. 2012;19:426–30. doi: 10.1007/s00534-011-0454-x. [DOI] [PubMed] [Google Scholar]
- 23.Jeong CW, Kim SH, Kim HT, Jeong SJ, Hong SK, Byun SS, et al. Insufficient Joint forces of first-generation articulating instruments for laparoendoscopic single-site surgery. Surg Innov. 2012 doi: 10.1177/1553350612468961. [DOI] [PubMed] [Google Scholar]
- 24.Aldrighetti L, Guzzetti E, Ferla G. Laparoscopic hepatic left lateral sectionectomy using the LaparoEndoscopic Single Site approach: Evolution of minimally invasive liver surgery. J Hepatobiliary Pancreat Sci. 2011;18:103–5. doi: 10.1007/s00534-010-0280-6. [DOI] [PubMed] [Google Scholar]
- 25.Vestweber B, Alfes A, Paul C, Haaf F, Vestweber KH. Single-incision laparoscopic surgery: A promising approach to sigmoidectomy for diverticular disease. Surg Endosc. 2010;24:3225–8. doi: 10.1007/s00464-010-1090-2. [DOI] [PubMed] [Google Scholar]


