Abstract
Little information is available publicly on invasive meningococcal disease (IMD) in elderly people in Australia. This study analysed IMD notifications data from New South Wales between 1993 and 2012 to determine the distribution of IMD among people aged 65 years and older and to describe the characteristics of IMD in this age group compared to younger age groups with respect to notification trends, serogroup distribution and mortality rates. Following introduction of a childhood vaccination programme against meningococcal type C in 2003, notification rates in all age groups decreased, but the proportion of IMD notifications in people aged 65 years and over rose significantly (from 4% to 6%, P = 0.01). Mortality rates from IMD in those aged 65 years and older were significantly higher than overall rates (32% compared to 5%, P < 0.01). Serogroup Y accounted for 23% of infections in the elderly compared to 3% in people aged under 65 years (P < 0.01). As the population ages, the elderly may account for a higher number of IMD cases in Australia. Protocols at the state and national level should be updated to provide guidance on the clinical and public health management of elderly people with IMD.
Introduction
Invasive disease caused by Neisseria meningitidis occurs when bacteria enter a normally sterile site such as blood (causing septicaemia) or cerebrospinal fluid (causing meningitis).1 Transmission is by respiratory droplets and up to 10% of the population may harbour Neisseria meningitidis in their nasopharynx without disease.1 Asymptomatic carriage is higher in household contacts of patients with meningococcal disease (12.4%).2 In Australia, the highest rates of invasive meningococcal disease (IMD) are among children under 5 years and young adults between 15 and 24 years of age.3
Five serogroups (A, B, C, W135 and Y) are responsible for the majority of IMD worldwide,4 with serogroups B and C the most commonly reported in Australia.1 Serogroup C vaccine is the only meningococcal vaccine routinely offered to all children in Australia under the National Immunization Programme. The national meningococcal C vaccination programme, introduced in Australia in January 2003, comprises ongoing inclusion of the vaccine in the National Immunization Programme schedule at one year of age, as well as a catch-up programme until 2006 for children aged 2–19 years.3,4 Large decreases have since been observed in serogroup C infections, with a 92% decline in the number of notifications of this serotype in the 15–24 year age group.4 Across all age groups, notification of IMD in Australia decreased by half from a rate of 2 per 100 000 to 1 per 100 000 population between 2004 and 2010.1
The state of New South Wales (NSW; the largest Australian state) has a population of over 7.2 million; 1 million (14%) are aged 65 years and over. The population is ageing, and the number of people in this age group grew by 22% between 2001 and 2011.5 Throughout Australia, the proportion of the population aged 65 years and over is projected to increase to just under a quarter of the total population by 2056.6 Confirmed and probable cases of IMD in NSW have been notifiable by clinicians and laboratories since 1990 under the NSW Public Health Act (Box 1). Case notification and surveillance data are entered into the NSW Notifiable Conditions and Information Management System, including details on age and serogroup information where available.7
Box 1. Meningococcal disease case definitions, New South Wales, Australia.
|
Case |
Definition |
| Confirmed | Requires either laboratory definitive evidence, OR laboratory suggestive evidence AND clinical evidence. Laboratory definitive evidence • Isolation of Neisseria meningitidis from a normally sterile site; OR • Detection of specific meningococcal DNA sequences in a specimen from a normally sterile site by nucleic acid amplification testing. Laboratory suggestive evidence • Detection of Gram negative diplococci in Gram stain of specimen from a normally sterile site or from a suspicious skin lesion; OR • High titre IgM or significant rise in IgM or IgG titres to outer membrane protein antigens of Neisseria meningitidis. Clinical evidence • A disease which is compatible with invasive meningococcal disease in the opinion of the treating clinician. |
| Probable | Requires clinical evidence only: • The absence of evidence for other causes of clinical symptoms; AND EITHER • Clinically compatible disease including haemorrhagic rash; OR • Clinically compatible disease AND close contact with a confirmed case within the previous 60 days. |
Little has been reported on IMD incidence in the elderly internationally, with no reports published in Australia. In late 2012, the Hunter New England Local Health District in northern NSW was notified of a case of IMD in a resident of an aged care facility. The response to this case revealed a lack of published guidance with respect to the public health management of IMD in the elderly, particularly in the definition of close contacts and administration of clearance treatment.
The aim of the current epidemiological investigation was to examine IMD trends in NSW with a particular focus on the proportion of notifications in people aged 65 years and over, mortality rates and serogroup distribution. Implications for the prevention and management of IMD are also discussed.
Methods
IMD notification data for the period 1993 to 2012 for NSW were sourced from the NSW Ministry of Health. Analysis was performed using Microsoft Excel, Statistical Analysis Software (SAS) Enterprise Guide 5.1 (SAS Institute Inc. Seattle, WA, USA) and STATA 11 (Stata Corp. 2009, College Station, TX, USA). IMD notification rates were calculated using mid-year NSW population data from the Australian Bureau of Statistics and proportions were compared using the χ2 (χ2) test.
Annualized notification rates by age groups (10–14, 0–14, 15–24, 25–64 year olds and people aged 65 years and over) were compared over two periods, 1993 to 2002 and 2003 to 2012, corresponding to periods before and after introduction of the national childhood meningococcal C vaccination programme in 2003. The 0–14 year age group was further divided into 0–4, 5–9 and 10–14 years. Wider age ranges were chosen to facilitate comparison between people aged 65 years and over and younger age groups, particularly those aged under 25 who are considered most at risk of IMD. Rate ratios and 95% confidence intervals were calculated for each age group to compare 2003 to 2012 notification rates with 1993 to 2002.
Analysis by serogroup was conducted for 2003 to 2012, the years for which serogroup information was recorded for more than 70% of notifications; cases diagnosed by polymerase chain reaction were not further typed. Case fatality rates (CFRs) were also limited to 2008 and 2012 due to missing data before this time.
This project used de-identified data routinely collected under the NSW Public Health Act. The project was further deemed a quality improvement exercise and an ethics waiver was granted by the Hunter New England Local Health District Human Research Ethics Committee.
Results
Notifications by age group
Between 1993 and 2012, there were 2995 notifications of IMD in NSW. Annual notifications peaked at 253 in 2000, decreasing to 66 in 2012 (Fig. 1). The age group with the highest number of notifications each year was 0–14 year olds; the lowest was observed for the 65 years and over age group (Fig. 1).
Fig. 1.
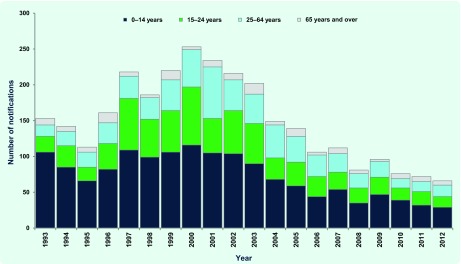
Invasive meningococcal disease notifications by year and age group, New South Wales, Australia, 1993 to 2012
Over the 20-year period, there were 153 notifications (5.1%) in those aged 65 years and over. The proportion of IMD notifications for those aged 65 years and over significantly increased from 4% in the period 1993–2002 to 6% in the period 2003–2012 (P = 0.01). Although annualized rates per 100 000 population decreased significantly across all age groups between 1993–2002 and 2003–2012, the decrease was primarily for younger age groups compared with those aged 65 years and over (Table 1).
Table 1. Changes in invasive meningococcal disease notification rates by age group, New South Wales, Australia, 1993 to 2002 and 2003 to 2012.
| Age group (years) | 1993 to 2002 | 2003 to 2012 | Rate ratio (95% confidence interval) | P-value | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | Rate per 100 000 | n | % | Rate per 100 000 | |||
| 0–14 | 978 | 51.5 | 74.1 | 497 | 45.2 | 37.04 | 0.50 (0.45–0.56) | < 0.001 |
| 0–4 | 701 | 36.9 | 159.8 | 371 | 33.8 | 82.79 | 0.52 (0.46–0.59) | < 0.001 |
| 5–9 | 151 | 8.0 | 34.1 | 76 | 6.9 | 17.18 | 0.50 (0.38–0.66) | < 0.001 |
| 10–14 | 126 | 6.6 | 28.7 | 50 | 4.5 | 11.08 | 0.39 (0.28–0.53) | < 0.001 |
| 15–24 | 479 | 25.3 | 54.3 | 267 | 24.3 | 28.34 | 0.52 (0.45–0.61) | < 0.001 |
| 25–64 | 357 | 18.8 | 10.8 | 264 | 24.0 | 7.12 | 0.66 (0.56–0.77) | < 0.001 |
| 65 and over | 82 | 4.3 | 10.2 | 71 | 6.5 | 7.37 | 0.72 (0.53–0.99) | 0.045 |
| Total | 1896 | 100.0 | 30.0 | 1099 | 100.0 | 15.81 | 0.53 (0.49–0.57) | < 0.001 |
Case fatality rates
Mortality data were available for 366 of 390 IMD notifications between 2008 and 2012, with 19 deaths recorded: three in 0–14 year olds, one in 15–24 year olds, 10 in 25–64 year olds and six in those aged 65 years and over. The CFR for those aged 65 years and over was significantly higher than the overall CFR (32% [6/19] compared with 5% [19/366]; P < 0.01) and also than the CFR for the 0–4 year old age group (1% [3/127]; P < 0.01), those historically at greatest risk of mortality.
Notifications by serogroup
Between 2003 and 2012, serogroup information was available for 64/71 (90%) notifications in those aged 65 years and over and for 787/1028 (77%) notifications in people under 65 years of age. During this period, there was a gradual reduction in the proportion of infections caused by serogroup C and an increase primarily in the proportion caused by serogroup B (Fig. 2).
Fig. 2.
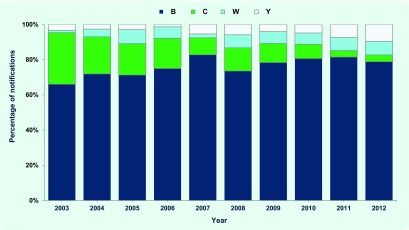
Invasive meningococcal disease notifications by year and serogroup, New South Wales, Australia, 2003 to 2012
Of the 64 notifications in those aged 65 years and older, 30 (47%) were serogroup B, 10 (16%) were serogroup C, 15 (23%) were serogroup Y and 9 were (14%) serogroup W. For those under 65 years of age, 605 (77%) were serogroup B, 125 (16%) were serogroup C, 21 (3%) were serogroup Y and 35 (4%) were serogroup W. The difference in proportions attributable to serogroup Y infection between the two age groups was statistically significant (P < 0.01).
Across all age groups, the proportion of IMD notifications attributable to serogroup Y significantly increased from 3% (17/539) in the period 2003–2007 to 6% (19/312) in the period 2008–2012 (P > 0.05). For those aged under 65 years, the proportion of notifications attributable to serogroup Y experienced a slight but steady increase between 2003 and 2012, while for older age groups there was variability from year to year (Fig. 3).
Fig. 3.
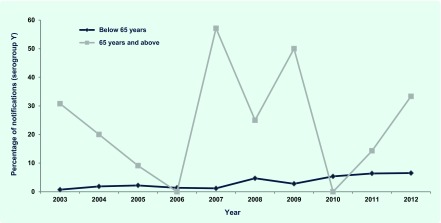
Proportion of invasive meningococcal disease notifications attributable to serogroup Y by year and age group, New South Wales, Australia, 2003 to 2012
Discussion
The absolute number of IMD cases in NSW residents aged 65 years and over has remained low over the past 20 years, and rates for all age groups have decreased, most likely as a result of the herd immunity effect of the childhood meningococcal C vaccination programme. However, the 65 years and over age group constituted an increasing proportion of all notifications had a higher proportion of infections of serogroup Y. Almost one third of cases resulting in death.
An increase in the proportion of IMD due to serogroup Y has occurred in NSW during the past 10 years. This has been previously reported throughout Australia, although statistical significance was not demonstrated.8 Research in the United States of America and United Kingdom has also found a higher prevalence of serogroup Y in older people.9,10 Higher CFRs have previously been reported in older people with IMD (particularly among those with underlying medical conditions) and among serogroup Y cases even after controlling for age.9–11 This may explain the higher CFR in older persons in this study; they had a higher proportion of infection with serogroup Y.
Potential increases in the number of IMD cases among the elderly, as a result of an ageing population, have implications not only for the clinical management of these cases but also for the public health response. The current Guidelines for the early clinical and public health management of meningococcal disease in Australia recommend provision of clearance antibiotics to household contacts or household-like contacts in settings such as schools or universities but do not specifically address aged care or residential facilities.12 A similar lack of specificity is also found in other national and regional guidelines (Table 2) with no particular guidelines on meningococcal disease available for the Western Pacific Region.
Table 2. Recommendations on use of chemoprophylaxis in general and in aged care facilities following a case of invasive meningococcal disease – various guidelines.
| Country or Region | Guideline | Recommendations on use of chemoprophylaxis in general and in aged care facilities |
|---|---|---|
| Australia | Guidelines for the early clinical and public health management of meningococcal disease in Australia. Canberra, Australian Government of Health and Ageing and Communicable Diseases Network Australia, October 2007.12 | “The household contacts of a case, including recent visitors who have stayed overnight in the 7 days preceding the onset of the case’s illness should receive clearance antibiotics and vaccination. … Those who share the same dormitory, military barrack or hostel bunkroom as a case are, in effect, household contacts.” p39 No specific mention of aged care facilities. |
| United Kingdom |
Guidance for public health management of meningococcal disease in the United Kingdom. London, Health Protection Agency United Kingdom, March 2012 (http://www.hpa.org.uk/webc/hpawebfile/hpaweb_c/1194947389261). |
“Chemoprophylaxis should be offered to close contacts of cases… in the following categories: (a) Those who have had prolonged close contact with the case in a household type setting during the seven days before onset of illness. Examples of such contacts would be those living and/or sleeping in the same household (including extended household)….Prophylaxis not indicated (unless already identified as close contacts) for …residents of nursing/residential homes.” p22 |
| United States of America |
Prevention and Control of Meningococcal Disease: Recommendations of the Advisory Committee on Immunization Practices. Atlanta, United States Centers for Disease Control and Prevention, March 2013 (http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6202a1.htm). |
“Antimicrobial chemoprophylaxis of close contacts of a patient with invasive meningococcal disease is important to prevent secondary cases. Close contacts include: (1) household members (2) child-care centre contacts, and (3) anyone directly exposed to the patient’s oral secretions... … in the 7 days before symptom onset.” p23 No specific mention of aged care facilities. |
| Canada | Guidelines for the Prevention and Control of Meningococcal Disease. Ottawa, Public Health Agency of Canada, May 2005 (http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/05vol31/31s1/). | “Chemoprophylaxis should be provided to close contacts … .” p7. Close contacts defined as including: – household contacts of a case – persons who share sleeping arrangements with a case. p3 No specific mention of nursing homes other than as potential location for organization based outbreaks. p4 |
| New Zealand | Communicable Disease Control Manual – Neisseria meningiditis invasive disease. Wellington, New Zealand Ministry of Health, May 2012 (http://www.health.govt.nz/publication/communicable-disease-control-manual-2012). | Contact defined as, “Anyone who has had unprotected contact with upper respiratory tract or respiratory droplets from the case during the 7 days before onset of illness to 24 hours after onset of effective treatment.” p3 “Public health follow-up is important for household contacts and contacts that have had similarly close exposure. Examples of such contacts are: • those sleeping at least one night in the same household, dormitory, military barrack, student hostel bunkroom (not residents of nursing or residential homes who sleep in separate rooms) as the case ….” p4 |
| Europe | Public health management of sporadic cases of invasive meningococcal disease and their contacts. Stockholm, European Centre for Disease Prevention and Control, October 2010 (http://www.ecdc.europa.eu/en/publications/publications/1010_gui_meningococcal_guidance.pdf). | “Chemoprophylaxis with an antibiotic regime that eradicates carriage is recommended for household contacts of a case of IMD.” p12 No definition of “household contacts” or mention of aged care facilities specifically. |
Outbreaks in residential aged care facilities have been reported, but specific studies are limited and provide contradictory advice.13 Prophylaxis was administered following a case of meningococcal disease in an aged care facility in the United States of America in 1997; a further case was then reported in a patient who had refused prophylaxis.14 A carriage study in the United Kingdom conducted after a case of meningococcal disease was diagnosed in a nursing home conversely found that no residents or caregivers had the same sero-subtype of Neisseria meningitidis as the index case, and the study concluded that prophylaxis was not necessary in such settings.15
The analyses on serogroup and mortality presented in this study should be interpreted with caution given the amount of missing information, particularly between 1993 and 2002 and because the estimates among older people are based on relatively small numbers. It is also likely that mortality was underestimated across all age groups, given the difficulty in determining a single cause of death. However, as IMD is a notifiable and serious disease, affected patients are likely to present in a health -care setting and be tested and notified by a treating physician, thus the notification data should approximate incidence.
Conclusion
The epidemiology of IMD in NSW, Australia has changed following the introduction of the childhood vaccination programmes, with a higher proportion of infections in those aged 65 years and over attributable to serogroup Y. Similar analysis should be conducted at the national and regional levels to determine whether similar trends are occurring across Australia and other countries that have introduced childhood meningococcal C vaccination programmes. As the Australian population is ageing, there may be increases in the number of notifications of IMD among people aged 65 years and over, including cases and potentially outbreaks in aged care facilities. Such an increase would have serious implications given the higher mortality rates in this group. National protocols should be updated to provide clinical and public health guidance for this age group.
Acknowledgements
Praveena Gunaratnam is employed as a trainee on the NSW Public Health Officer Training Programme, funded by the NSW Ministry of Health. She undertook this work based at the Hunter New England Population Health. The Programme is offered in partnership with the University of NSW.
Conflict of Interest
None declared.
Funding
None.
References
- 1.NNDSS Annual Report Writing Group Australia’s notifiable disease status, 2010. Communicable Diseases Intelligence. 2012;36:1–69. [PubMed] [Google Scholar]
- 2.Kristiansen BE, Tveten Y, Jenkins A. Which contacts of patients with meningococcal disease carry the pathogenic strain of Neisseria meningitidis? A population based study. BMJ (Clinical Research Ed.) 1998;317:621–5. doi: 10.1136/bmj.317.7159.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Government Department of Health and Ageing and the National Health and Medical Research Council. The Australian Immunisation Handbook 9th Edition Canberra, Australian Government Department of Health and Ageing, 2008 (http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/78CDF41C283426A8CA2574E40020CCAB/$File/handbook-9.pdf, accessed 15 September 2013).
- 4.Halperin SA, et al. The changing and dynamic epidemiology of meningococcal disease. Vaccine. 2012;30(Suppl 2):B26–36. doi: 10.1016/j.vaccine.2011.12.032. [DOI] [PubMed] [Google Scholar]
- 5.Population by Age and Sex. Regions of Australia, 2011 Cat No 3235.0. Canberra, Australian Bureau of Statistics, 2012. [Google Scholar]
- 6.Australian Social Trends. September 2009 Cat No 4102.0. Canberra, Australian Bureau of Statistics, 2009. [Google Scholar]
- 7.Control Guideline. Meningococcal Disease, last updated: 01 July 2012 Australia, New South Wales Health, 2012 (http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/mening.aspx, accessed 15 September 2013).
- 8.Lahra MM, Enriquez RP. Annual report of the Australian Meningococcal Surveillance Programme, 2011. Communicable Diseases Intelligence. 2012;36:E251–62. [PubMed] [Google Scholar]
- 9.Cohn AC, et al. Changes in Neisseria meningitidis disease epidemiology in the United States, 1998–2007: implications for prevention of meningococcal disease. Clinical Infectious Diseases. 2010;50:184–91. doi: 10.1086/649209. [DOI] [PubMed] [Google Scholar]
- 10.Ladhani SN, et al. Invasive meningococcal capsular group Y disease, England and Wales, 2007–2009. Emerging Infectious Diseases. 2012;18:63–70. doi: 10.3201/eid1801.110901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Prevention and Control of Meningococcal Disease: Recommendations of the Advisory Committee on Immunization Practice. Morbidity and Mortality Weekly Report 201362http://www.cdc.gov/mmwr/pdf/rr/rr6202.pdfaccessed 15 September 2013 [Google Scholar]
- 12.Australian Government Department of Health and Ageing and Communicable Diseases Network Australia. Guidelines for the early clinical and public health management of meningococcal disease in Australia Canberra, Australian Government Department of Health and Ageing, 2009 (http://www.health.gov.au/internet/main/publishing.nsf/Content/4DFF673115F66413CA257BF00020630F/$File/meningococcal-guidelines.pdf, accessed 15 September 2013).
- 13.Brooks R, et al. Increased case-fatality rate associated with outbreaks of Neisseria meningitidis infection, compared with sporadic meningococcal disease, in the United States, 1994–2002. Clinical Infectious Diseases. 2006;43:49–54. doi: 10.1086/504804. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Outbreaks of group B meningococcal disease–Florida, 1995 and 1997. Morbidity and Mortality Weekly Report, 1998, 47:833–837. pmid:9780239. [PubMed]
- 15.Irwin DJ, et al. Carriage of Neisseria meningitidis in residents and staff at a residential home for elderly people following a case of invasive disease. Communicable Disease and Public Health. 2000;3:172–4. [PubMed] [Google Scholar]


