Abstract
Objectives
Aim of this study was to prospectively determine the incidence and types of emergency department (ED) visits and admissions due to drug related problems (DRPs) at Riyadh Military Hospital (RMH), to assess the severity and preventability of these drug related admissions or visits, and to identify the drugs and patient groups that are most commonly involved.
Method
Patients (n = 300) were selected randomly from patients presented to the ED during the study period (one month). Computerized randomization program was used to select ten beds daily on different areas and times. Patient was eligible to be included if either visited ED or admitted through it due to DRPs.
Results
During the study period, 300 patients presented to ED were randomly selected with a mean age of 47.8 ± 27.7 years. One hundred and forty of them were females (46.67%) and 160 were male patients (53.33%). Of these 300 patients, 56 (18.7%) were presented to ED due to DRPs, and 244 (81.3%) patients were presented to ED due to non-drug related problems (NDRPs). About ninety-three percent (n = 52) of the DRP group were exposed to hospital admission while only 7.1% (n = 4) were ED visits (Fig. 2). Male to female ratio in ED visits was 3:1 while it was 9.7:8.9 in the ED admission group.
Conclusion
The prospective design of this study, sample size, and randomization increases the likelihood that our estimates are accurate and increase the generalizability of our findings. Most DRPs attributed to hospital admissions or visits were avoidable. Direct patient contact with pharmacist and family physician was beneficial in providing a safe and effective therapy. Corrective, preventive and educational strategies should concentrate on the most frequently reported populations, diseases and medications. The study addresses the proper use of medications to ensure the best outcomes of pharmacological interventions. Finally, more studies with longer duration focusing on DRPs in Saudi Arabia are needed.
Keywords: Emergency, Admission, Visit, Drug, Related, Problem, Hospital
1. Introduction
Nowadays medication use is increasing world-wide. (WHO, 2011; IMS, May 2011) The United States Food and Drug Administration (USFDA) has approved more than 10000 drugs and Saudi National Formulary currently lists more than 6000 drugs. (IMS, April 2011; Bawazir et al., 2009) The reasons may be the introduction of vast number of agents by the advanced pharmaceutical industry in addition to the wide spectrum of diseases that increased demands for intensifying therapeutic challenges. (El-bagir, 1997) When people use medications, any number of outcomes is possible. Most commonly, the patient benefits from pharmacotherapeutic interventions; however, adverse events, ranging from minor side effects to death, may occur. Any deviation from the intended beneficial effect of a medication results in a drug related problem (DRP). (Johnson and Bootman, 1995).
One or more DRPs may develop in a given patient after the initial drug therapy. Although many DRPs can be resolved without a major impact on patient’s health, some of them can be associated with significant morbidity and mortality. (Hepler and Strand, 1990; Classen et al., 1997) Hepler and Strand defined DRP as an event or circumstance involving drug treatment that actually or potentially interferes with the patients experiencing an optimum outcome of medical care. (Hepler and Strand, 1990) They also classified DRPs into eight general categories, which include untreated indication, treatment without indication, improper drug selection, too little drug, too much drug, noncompliance, adverse drug reaction (ADR), and drug interaction (Strand et al., 1990).
It has been estimated that DRPs account for 17 million emergency department (ED) visits and 8.7 million hospital admissions annually in the United States. (Johnson and Bootman, 1995) Between 1995 and 2000, a probability model estimated that costs associated with morbidity and mortality secondary to DRPs have more than doubled from US$ 76.6 billion to more than US$ 177.4 billion. (Johnson and Bootman, 1995; Ernst and Grizzle, 2001) Although a considerable number of studies were carried out determining the prevalence and incidence of DRPs, studies published to date are unable to offer precise information about the frequency of DRPs (McKenney and Harrison, 1976). Winterstein and colleagues (2002) found that 7.1% of hospital admissions result from DRPs, of which 59% were considered preventable. (Winterstein et al., 2002) Zed et al. (2008) concluded that DRPs counted for 12% of emergency department visits and 68% of them were considered preventable. Rates of hospital admissions were higher and the length of hospital stay appears to be longer among patients whose visits were drug-related than among patients who presented for other reasons (Zed et al., 2008).
Adverse drug reactions (ADRs) are an important cause of morbidity and hospital admissions among the elderly (Nebeker et al., 2004). A meta-analysis of observational studies revealed that a considerable part of all hospital admissions is related to ADRs. ADRs were mainly associated with age, sex, genetic polymorphism, polypharmacy, and co-morbidity (Beijer and de Blaey, 2002). The World Health Organization (WHO) defines adverse drug reaction as any harmful, unintended reactions to medicines that occur at doses normally used for prophylaxis, diagnosis or treatment (WHO, 2008). Patterns and types of drug use, misuse, and abuse vary widely across communities, metro areas, regions, and states and these differing patterns across varied geographic areas must be understood if appropriate prevention and treatment interventions are to be undertaken. As the front line of pre hospital care for individuals experiencing acute adverse consequences of drug use, emergency departments (EDs) provide valuable insights into the more serious aspects of certain patterns of drug use (Office of Applied Studies, 2010).
DRPs are common among older people after hospital discharge and are relevant since they threaten patient’s safety. (Nolan and O’Malley, 1988) In fact, the incidence of hospital admissions and visits increased with age and especially elders are more prone to drug related visits to hospitals, some studies evaluated age as a variable. (Nolan and O’Malley, 1988) However, elderly patients may have multiple disease states and may use a wide variety of drugs, increasing the potential for altered responsiveness to drugs and a higher incidence of adverse effects compared with younger patients (Montamat et al., 1989). In United States of America, estimates on drug-related visits to hospital emergency departments (ED) are obtained from the Drug Abuse Warning Network (DAWN), (Zed et al., 2008) a public health surveillance system managed by the Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services (HHS) and there was no such mechanism in Saudi Arabia.
Although El-bagir (1997) found that DRPs constitute a minor problem in Saudi Arabia, (El-bagir, 1997), Al Olah and Al Thiab (2008) found that DRPs constitute serious problems in health care life of people in Saudi Arabia (Al Olah and Al Thiab, 2008). However they agreed that there is a potential for their increase in the future (El-bagir, 1997; Al Olah and Al Thiab, 2008). Accordingly, the aim of our study is to prospectively determine the incidence and types of ED visits and admissions due to DRPs at Riyadh Military Hospital (RMH). Secondary objectives include assessment of the severity and preventability of these drug related admissions or visits and identifying the drugs and patient groups that are most commonly involved.
2. Methods
This prospective cohort observational study was conducted at an ED in a military hospital (RMH), Riyadh, Saudi Arabia. The study was carried out over a period of one month from 17th September to 16th October 2011 and was approved by the Clinical Research Committee at RMH. RMH is a tertiary referral hospital and the ED is physically divided into three areas: “acute care” for major and serious problems, “stabilized” for stable cases and “fast-track”. Ethical approval was obtained from clinical and research center at RMH.
According to ED statistics, about 10,000 patients are seen monthly. A sample of 300 patients was selected randomly from patients presented to the ED during the one month period specified. Randomization was carried out by using a computerized randomization program to select ten beds daily on different areas and times randomly. The patient is eligible to be included if either visited ED or admitted through it due to DRPs during the study period. The data were collected to determine the incidence of admissions through the ED due to DRPs, types of DRPs, and to assess the preventability of admissions due to DRPs. All the required information were taken by one of the authors (Hanan) from the patient file and/or patient interviewing using the data collection sheet designed especially for this purpose (Fig. 1). These information include chief complaint, past medical history, medication history, and allergy status. Laboratory results (e.g. drug level) and results of diagnostic tests were used when required.
Figure 1.
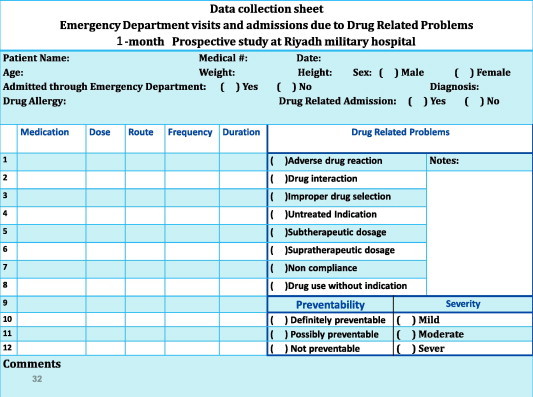
Data collection sheet.
The definitions used in this study, as described in similar studies, (Al Olah and Al Thiab, 2008; Malhotra et al., 2001) are as the following:
DRPs were defined according to the Strand et al. classification mentioned earlier in the introduction (Strand et al., 1990). Adverse drug reaction–any response that is noxious and unintended and that occurs at doses normally used in humans for prophylaxis, diagnosis, or treatment, excluding a failure to accomplish the intended purpose (Karch and Lasagna, 1975). A drug interaction is a medical problem resulting from a drug–drug, drug–food, or drug–laboratory interaction; Drug non-compliance–the extent to which the patient’s drug taking behavior (in terms of taking medication) coincides with the prescription (Haynes et al., 1979); Failure to receive drugs is a medical problem that resulted from not receiving a drug (e.g., for pharmaceutical, psychological, sociological, or economic reasons); Improper drug selection was the taking of a wrong drug (other than one prescribed by the physician); Drug overdose was a medical problem treated with too much of the correct drug (toxicity); Untreated indication was a medical problem that required drug therapy (an indication for drug use), but for which the patient was not receiving a drug; Drug-related visits were defined as ED visits caused by DRPs; Drug related hospital admission–Admission caused by any undesirable clinical manifestation that is consequent to and caused by the administration of a particular drug. The clinical manifestation may be a clinical sign, symptom, or abnormal laboratory test or it may be a cluster of abnormal signs, symptoms, or tests. (McKenney and Harrison, 1976; Col et al., 1990).
DRPs were defined as ‘definitely preventable’ if the patient (1) did not take a drug that is known to reduce or prevent the symptoms according to the prescribed directions, (2) had a known allergy, (3) had a disease for which the drug was contraindicated, and (4) took a drug that was not indicated, and possibly avoidable if there is a failure to monitor by a physician at reasonable time intervals and inadequate monitoring due to inability to see a physician (e.g., financial difficulties) (Nelson and Talbert, 1996). Severity was classified as mild (laboratory abnormality or symptom not requiring treatment), moderate (laboratory abnormality or symptom requiring treatment or admission to hospital or resulting in nonpermanent disability), severe (abnormality or symptom that was life-threatening or resulted in permanent disability) or fatal (Singh et al., 2011). Simple statistics were used for analysis and description of the data. All statistical parameters were analyzed by using Microsoft Excel 2007.
3. Results
During the study period, 300 patients presented to ED were randomly selected with a median age of 51 with an interquartile range of 47 years. One hundred and forty of them were females (46.67%) and 160 were male patients (53.33%). Of these 300 patients, 56 (18.7%) were presented to ED due to DRPs, and 244 (81.3%) patients were presented to ED due to non drug related problems (NDRPs). About ninety-three percent (n = 52) of the DRP group were exposed to hospital admission while only 7.1% (n = 4) were ED visits (Fig. 2). Male to female ratio in ED visits is 3:1 while it is 9.7:8.9 in the ED admission group (Table 1). Additionally, Table 1 shows the distribution of the DRP group into visits or admissions according to the age groups and gender in addition to the incidence of both admissions and visits according to the gender in both DRP and NDRP groups. Male to female ratio is 8:7 in the study population and it is 1.5:1.3 in the DRP group (Table 1).
Figure 2.
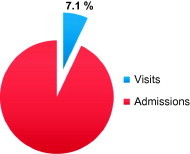
Showing admissions and visits due to DRPs.
Table 1.
Description of the study population according to gender.
| Male (%) | Female (%) | Total (%) | ||
|---|---|---|---|---|
| 1- Demographic data of patients | ||||
| Number (%) | 160 (53.33) | 140 (46.67) | 300 | |
| Age (median/interquartile range) years | 47/48.75 | 55/46.75 | 51 /47 | |
| 2- The incidence of drug related admissions or visits to RMH ED in both groups, DRPs or NDRPs, according to the gender. | ||||
| DRPs Number (%) | 30 (53.57) | 26 (46.43) | 56 (18.67) | |
| NDRPs Number (%) | 130(53.28) | 114(46.72) | 244(81.33) | |
| Total Number (%) | 160 (53.33) | 140 (46.67) | 300 (100) | |
| 3- Admissions and visits to hospital in both groups, DRPs or NDRPs, according to gender | ||||
| Admissions | ||||
| NDRPs (DRPs) | 139 (29) | 112 (23) | 251 (52) | |
| Visits | ||||
| NDRPs (DRPs) | 21 (1) | 28 (3) | 49 (4) | |
| Total | ||||
| NDRPs (DRPs) | 160 (30) | 140 (26) | 300 (56) | |
| 4- Admissions and visits to hospital due to DRPs according to gender | ||||
| Admissions | ||||
| Number | 29 | 23 | 52 | |
| % within gender | 96.7 | 88.5 | 92.9 | |
| % within admissions or visits | 55.8 | 44.2 | 100 | |
| Visits | ||||
| Number | 1 | 3 | 4 | |
| % within gender | 3.3 | 11.5 | 7.1 | |
| % within admissions or visits | 25.0 | 75.0 | 100 | |
| Total | ||||
| Number | 30 | 26 | 56 | |
| % within gender | 100 | 100.0 | 100.0 | |
| % within admissions or visits | 53.6 | 46.4 | 100 | |
| 5- Average number of medications in patients with DRPs according to gender | ||||
| Number of medications Mean ± SD | 5.96 ± 3.97 | 6.27 ± 4 | ||
| 6- Drug related problems in different age groups for both sexes | ||||
| Age group | ||||
| Pediatric(<12 years) DRP number (% within Age group) | 5 (62.5) | 3 (37.5) | 8 (100) | |
| Adults (12–65 years) DRP number (% within Age group) | 13 (48.1) | 14 (51.9) | 27 (100) | |
| Elderly (>65 years) DRP number (% within Age group) | 12 (57.1) | 9 (42.9) | 21 (100) | |
| Total DRPs (%) | 30 (53.6) | 26 (46.4) | 56 (100) | |
Out of 244 patients who were presented to ED for NDRPs, only 18.4% (n = 45) were ED visits and 81.7% (n = 199) were hospital admissions. The percentage of ED presentation due to DRPs was high in adults of 48.1% (n = 27), followed by elderly of 37.50% (n = 21), and finally pediatrics of 14.29% (n = 8) (Table 2).
Table 2.
Incidence and age group classification of drug related admissions or visits to RMH.
| Group | Visits number (% total visits) | Admission number (% total admissions) | Total number (% total) |
|---|---|---|---|
| 1- The incidence of drug related admissions or visits to RMH ED | |||
| DRPs | 4 (8.2%) | 52 (20.7%) | 56 (18.7%) |
| NDRPs | 45 (91.8%) | 199 (79.3%) | 244 (81.3%) |
| Total | 49 (100%) | 251 (100%) | 300 (100%) |
| Age group | Visits (% within Age group) | Admissions (% within Age group) | Total (% within Age group) |
| 2- Admissions and visits due to DRPs in different age group | |||
| Pediatric(<12 years) | 1 | 7 | 8 |
| (12.5) | (87.5) | (100) | |
| Adults (12–65 years) | 3 | 24 | 27 |
| (11.1) | (88.9) | (100) | |
| Elderly (>65 years) | 0 | 21 | 21 |
| (0.0) | (100.0) | (100.0) | |
| Total (%) | 4 | 52 | 56 |
| (7.1) | (92.9) | (100) | |
The most common DRPs was due to adverse drug reactions (ADRs) (30.4%) and patients’ non-compliance (30.4%), followed by untreated indication (10.7%), then drug interactions ; supratherapeutic and subtherapeutic dose (7.1% for each), followed by improper drug selection (5.4%) and the least contribution was for drug use without indication (1.8%). The contribution of each of the DRPs to cause ED admissions and visits in both male and female patients was shown in Fig. 3. It is to be noted that ADR incidence is almost double in female patients than male (11:6). Drug interactions presented only in elderly patients while non compliance and ADRs are the most prominent DRPs in adults and pediatric patients respectively. Importantly, ADRs in pediatric patients contribute to 50% of all ADRs identified in the study subjects (Table 3).
Figure 3.
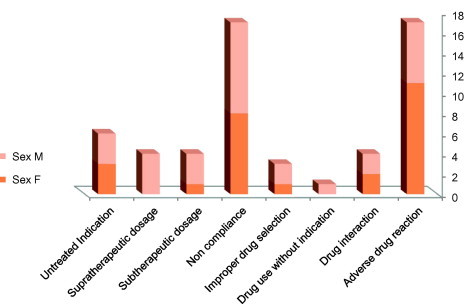
Types of DRPs with distribution between males and females.
Table 3.
Identified types and incidence of DRPs in ED at RMH and categorization according to gender, age group, preventability and severity.
| DRPs | Gender |
Age group |
Preventability |
Severity |
Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Pediatric | Adults | Elderly | Definitely preventable | Definitely preventable | Definitely preventable | Mild | Moderate | Severe | ||
| Adverse drug reaction | ||||||||||||
| % within DRPs | 11 | 6 | 4 | 8 | 5 | 1 | 8 | 8 | 7 | 9 | 1 | 17 |
| % within Group | 64.7 | 35.3 | 5.9 | 47.1 | 47.1 | 41.2 | 52.9 | 5.9 | 100.0 | |||
| 42.3 | 20.0 | 50.0 | 29.6 | 23.8 | 5.6 | 100.0 | 26.7 | 33.3 | 33.3 | 12.5 | 30.4 | |
| Drug interaction | 2 | 2 | 0 | 0 | 4 | 0 | 0 | 4 | 0 | 3 | 1 | 4 |
| % within DRPs | 50.0 | 50.0 | 0.0 | 0.0 | 100.0 | 0.0 | 75.0 | 25.0 | 100.0 | |||
| % within Group | 7.7 | 6.7 | 0.0 | 0.0 | 19.0 | 0.0 | 0.0 | 100.0 | 0.0 | 11.1 | 12.5 | 7.1 |
| Drug use without indication | 0 | 1 | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| % within DRPs | 0.0 | 100.0 | 100.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 | 100 | |||
| % within Group | 0.0 | 3.3 | 12.5 | 7.4 | 0.0 | 5.6 | 0.0 | 0.0 | 0.0 | 3.7 | 0.0 | 1.8 |
| Improper drug selection | 1 | 2 | 0 | 2 | 4 | 0 | 0 | 3 | 2 | 1 | 0 | 3 |
| % within DRPs | 33.3 | 66.7 | 0.0 | 0.0 | 100.0 | 66.7 | 33.3 | 0.0 | 100 | |||
| % within Group | 3.8 | 6.7 | 0.0 | 7.4 | 19.0 | 0.0 | 0.0 | 10.0 | 9.5 | 3.7 | 0.0 | 5.4 |
| Non compliance | 8 | 9 | 1 | 1 | 2 | 12 | 0 | 5 | 7 | 7 | 3 | 17 |
| % within DRPs | 47.1 | 52.9 | 70.6 | 0.0 | 29.4 | 41.2 | 41.2 | 17.6 | 100.0 | |||
| % within Group | 30.8 | 30.0 | 12.5 | 3.7 | 9.5 | 66.7 | 0.0 | 16.7 | 33.3 | 25.9 | 37.5 | 30.4 |
| Subtherapeutic dosage | ||||||||||||
| % within DRPs | 1 | 3 | 1 | 3 | 0 | 0 | 0 | 4 | 2 | 2 | 0 | 4 |
| % within Group | 25.0 | 75.0 | 0.0 | 0.0 | 100.0 | 50.0 | 50.0 | 0.0 | 100.0 | |||
| 3.8 | 10.0 | 12.5 | 11.1 | 0.0 | 0.0 | 0.0 | 13.3 | 9.5 | 7.4 | 0.0 | 7.1 | |
| Supratherapeutic dosage | 0 | 4 | 1 | 10 | 6 | 3 | 0 | 1 | 1 | 2 | 1 | 4 |
| % within DRPs | 0.0 | 100.0 | 75.0 | 0.0 | 25.0 | 25.0 | 50.0 | 25.0 | 100.0 | |||
| % within Group | 0.0 | 13.3 | 12.5 | 37.0 | 28.6 | 16.7 | 0.0 | 3.3 | 4.8 | 7.4 | 12.5 | 7.1 |
| Untreated Indication | 3 | 3 | 0 | 1 | 0 | 1 | 0 | 5 | 2 | 2 | 2 | 6 |
| % within DRPs | 50.0 | 50.0 | 16.7 | 0.0 | 83.3 | 33.3 | 33.3 | 33.3 | 100.0 | |||
| % within Group | 11.5 | 10.0 | 0.0 | 3.7 | 0.0 | 5.6 | 0.0 | 16.7 | 9.5 | 7.4 | 25.0 | 10.7 |
| Total | 26 | 30 | 8 | 27 | 21 | 18 | 8 | 30 | 21 | 27 | 8 | 56 |
| % within DRPs | 46.4 | 53.6 | 32.1 | 14.3 | 53.6 | 37.5 | 48.2 | 14.3 | 100.0 | |||
| % within Group | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
Regarding the preventability of DRPs, 32.1% of them were considered definitely preventable, 53.6% were considered possibly preventable and only 14.3% were considered definitely non-preventable. All definitely non preventable DRPs belong to ADRs while other DRPs are of varying degrees of either preventable or possibly preventable. With regard to the severity of DRPs, only 14.3% were considered severe, 48.2% were considered moderate and 37.5% were considered mild. Non compliance is responsible for 37.5% of severe DRPs, followed by untreated indication (25%) and 12.5% for ADRs, drug interactions and supratherapeutic dose (Table 3). The most common drug groups associated with DRPs were antihypertensive agents (21.5%), anticoagulants (14.3%), immunosuppressants (12.5%) and chemotherapeutic agents (10.7%) (Fig. 4). The most common diagnosis associated with DRPs was hypertension (8.9%), diabetes mellitus (8.9%), stroke (7.1%), urinary tract infection (5.4%), drug overdose (5.4%), and febrile neutropenia (5.4%). The full list of diagnosis associated with DRPs is in Table 4. There is no significant difference between male and female groups with respect to identified DRPs and average number of medications. The identified number of DRPs in the male group was 30 with the average number of medications of 5.96 ± 3.97 while in the female group the identified number of DRPs is 26 and the average number of medications is 6.27 ± 4 (Table 1).
Figure 4.
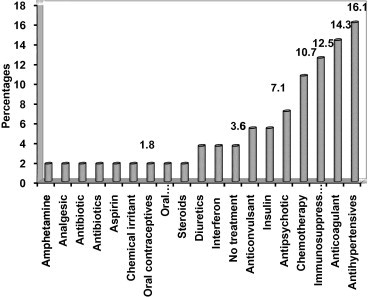
Identified drug groups associated with DRPs.
Table 4.
Diagnosis associated with DRPs.
| Diagnosis | Number (%) |
|---|---|
| Bronchial asthma (BA) | 1 (1.8) |
| Bulla pemphis | 1 (1.8) |
| Congestive heart failure (CHF) | 1 (1.8) |
| Diabetic foot/(DM) | 1 (1.8) |
| Drug induced psychosis | 1 (1.8) |
| Deep vein thrombosis (DVT) | 1 (1.8) |
| Gallstone | 1 (1.8) |
| Hodgkin lymphoma (HL) | 1 (1.8) |
| Increase INR | 1 (1.8) |
| Increase liver enzyme | 1 (1.8) |
| Hypotension | 1 (1.8) |
| Drug overdose | 1 (1.8) |
| Persistent colic | 1 (1.8) |
| Severe anemia | 1 (1.8) |
| Transient ischemic attack (TIA) | 1 (1.8) |
| Crohn’s disease (CD) | 1 (1.8) |
| Drug overdose | 2 (3.6) |
| Hyperglycemia/ (DM) | 2 (3.6) |
| Hypoglycemia/ (DM) | 2 (3.6) |
| Gastroenteritis | 2 (3.6) |
| Gastrointestinal basidiobolomycosis (GIB) | 2 (3.6) |
| Intracranial hemorrhage | 2 (3.6) |
| Electrolyte disturbance | 2 (3.6) |
| Multiple sclerosis (MS) | 2 (3.6) |
| Neuroleptic malignant syndrome (NMS) | 2 (3.6) |
| Sickle-cell anemia/Vaso-occlusive crisis | 2 (3.6) |
| Seizure | 2 (3.6) |
| Febrile neutropenia (FN) | 3 (5.4) |
| Community acquired pneumonia (CAP) | 3 (5.4) |
| Urinary tract infection (UTI) | 3 (5.4) |
| Stroke | 4 (7.1) |
| Hypertension | 5 (8.9) |
4. Discussion
Drug-related visits to the ED constitute a significant problem that contributes to the overall pressure on our health care system. DRPs are a serious and costly issue (Johnson and Bootman, 1995; Ernst and Grizzle, 2001) faced by health care professionals and the health care system in Saudi Arabia (Al Olah and Al Thiab, 2008). In recent years patient safety has become a major concern for health care providers, and medication management is one of its more relevant aspects. Prospective studies on DRPs identified that approximately 10–28% of ED visits were due to DRPs but retrospective studies identified them in the range of 0.86–10.6%. (Winterstein et al., 2002; Zed et al., 2008; Budnitz et al., 2006; Patel and Zed, 2002) This considerable variation in the incidence of drug-related visits to hospital emergency room is due to variable objectives, definitions and methods applied to the studies (Patel and Zed, 2002; Juntti-Patinen et al., 2006). Our study results show that drug-related hospital admissions and visits account for 18.7% of total ED admissions and visits (92.9% of them admissions and 7.1% visits) which means drug related admissions constitute 17.3% of total ED admissions. Hospital admissions of patients who visited the ED with a drug-related problem were estimated to be 8.6–24.2% and were associated with increased costs to health care systems (Patel and Zed, 2002). Moreover, the incidence of drug related hospital admissions in Saudi Arabia is increasing since El-Bagir (1997), Al-Olah et al. (2008) and our study reported the incidence of drug related hospital admissions to be 11%, 14.7% and 17.3% respectively (El-bagir, 1997; Al Olah and Al Thiab, 2008). The results of this study are consistent with international studies suggesting that the incidence of admissions through the ED due to DRPs in RMH is similar to that in other countries (Johnson and Bootman, 1995; Nelson and Talbert, 1996; Einarson, 1993; Ives et al., 1987; Hanlon et al., 2004). This brings to attention the importance of medicine management and reinforcing the patient centered care to ensure the best outcomes of pharmacotherapeutic interventions. The need for direct patient contact by pharmacists and family physicians is obvious and a collaborative and interdisciplinary patient centered care model is most beneficial to providing safe and effective therapy (Tom, 2001).
The most often encountered DRPs were patient’s non-compliance and ADRs which are consistent with the previous national study and international studies (Al Olah and Al Thiab, 2008; Patel and Zed, 2002). Moreover, both non-compliance and ADRs have been consistently cited as the primary reasons for drug related morbidity regardless of study setting. In our study, 32.1% of DRPs were assessed to be definitely preventable which is much less than those previously reported by Al-Olah and colleague (83%) that can be explained by methodological differences in both studies (Al Olah and Al Thiab, 2008). Possibly preventable DRPs were 53.6% which is comparable to international studies in developed countries which suggest that approximately 50% of DRPs were preventable (Nelson and Talbert, 1996).
The study revealed that the incidence of adult hospital admissions due to DRPs is higher if compared to elderly and pediatrics. However, elderly population is only 2.9 % of the Saudi population (UN, 2006) which means that the incidence is much higher among elderly population. Elderly patients may have multiple disease states and may use a wide variety of drugs, increasing the potential for altered responsiveness to drugs and a higher incidence of adverse effects compared to younger patients. (Malhotra et al., 2001; Montamat et al., 1989) Moreover, a substantial proportion of the elderly patients is non-compliant; estimates varying from 26% to 59% (Malhotra et al., 2001). However, better patient education about drug side effects and the pros and cons of unconventional therapies can help in decreasing noncompliance.
The high number of drugs per patient means that the likelihood of DRPs increases as the number of drugs prescribed rises which assures the direct relation between the number of drugs prescribed and both ED visits and admissions due to DRPs (Malhotra et al., 2001). Importantly, a greater number of medications would increase the potential for adverse drug reactions and poor adherence. Therefore, minimizing the total number of medications that individual patients receive might therefore reduce drug-related visits to the emergency department. This is consistent with the well known principle of geriatric clinical pharmacology: prescribe simpler regimens with fewer pills to be taken each day.
The pattern of severity of the patient outcomes associated with drug-related hospitalization is different from previous work (Singh et al., 2011). Singh et al. found that about 75% considered moderate where, in our study, it is only about the half of identified DRPs. In contrary, our study showed a higher percentage of severe outcomes (14.3%) compared to only 6.78% in Singh et al. study. Moreover, these severe outcomes were noticed with both non compliance and untreated indications which necessitate enforcing the possible corrective actions. Based on our study, particular effort should be made to prevent DRPs in hypertensive patients, stroke patients, diabetic patients, and in cases of seizure and fever in neutropenic patients. In addition, enforced counseling and education are needed for patients receiving antihypertensives, anticoagulants, chemotherapy, and immunosuppressant and over the counter drugs (OTC) and study involved patients presented at ED.
5. Conclusion
The prospective design of this study, sample size, and randomization increases the likelihood that our estimates are accurate and increase the generalizability of our findings. Most DRPs attributed to hospital admissions or visits were classified avoidable. Direct patient contact with pharmacist and family physician is beneficial to providing a safe and effective therapy. Corrective, preventive and educational strategies should concentrate on the most frequently reported populations, diseases and medications. The study addresses the proper use of medications to ensure the best outcomes of pharmacological interventions. Finally, more studies with longer duration focusing on DRPs in Saudi Arabia are needed.
6. Limitations
A significant number of patients with minor DRPs have been missed from the outpatient department and other major departments. In addition, short duration of the study and the fact that all data were collected in a single institution are the limitations of our work.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al Olah Y.H., Al Thiab K.M. Admission through the emergency department due to drug related problems. Ann. Saudi Med. 2008;28(6):426–429. doi: 10.5144/0256-4947.2008.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bawazir, SA, Alkharfy, KM, Al-shaqha, WM, Aminn, H, Alnaim, L, Aldhari, F, Albabtain, M, (Eds.) 2009. Saudi National Formulary, fourth ed., Saudi Food & Drug Authority and Saudi Pharmaceutical Society. Lexi-Comp, Inc., Hudson, Ohio.
- Beijer H.J., de Blaey C.J. Hospitalizations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm. World Sci. 2002;24(2):46–54. doi: 10.1023/a:1015570104121. [DOI] [PubMed] [Google Scholar]
- Budnitz D.S., Pollock D.A., Weidenbach K.N. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296:1858–1866. doi: 10.1001/jama.296.15.1858. [DOI] [PubMed] [Google Scholar]
- Classen D.C., Pestotnik S.L., Evans R.S., Lloyd J.F., Burke J.P. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA. 1997;277(4):301–306. [PubMed] [Google Scholar]
- Col N., Fanwle J.E., Krinholm P. The role of medication noncompliance and adverse drug reactions in hospitalization of the elderly. Arch. Intern. Med. 1990;150:841–845. [PubMed] [Google Scholar]
- Einarson T.R. Drug-related hospital admissions. Ann. Pharmacother. 1993;27:832–840. doi: 10.1177/106002809302700702. [DOI] [PubMed] [Google Scholar]
- El-bagir A.M. Drug-associated admissions to a district hospital in Saudi Arabia. J. Clin. Pharm. Ther. 1997;22(1):61–66. doi: 10.1046/j.1365-2710.1997.8375083.x. [DOI] [PubMed] [Google Scholar]
- Ernst F.R., Grizzle A.J. Drug-related morbidity and mortality: updating the cost of- illness model. J. Am. Pharm. Assoc. 2001;41:192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- Hanlon J.T., Lindbland C.I., Gray S.L. Can clinical pharmacy services have a positive impact on drug-related problems and health outcomes in community-based older adults? Am. J. Geriatr. Pharmacother. 2004;2(1):3–13. doi: 10.1016/s1543-5946(04)90002-5. [DOI] [PubMed] [Google Scholar]
- Haynes R.B., Taylor D.W., Sackette D.I., editors. Compliance in Health Care. Johns Hopkins University Press; Baltimore: 1979. [Google Scholar]
- Hepler C.D., Strand L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Hosp. Pharm. 1990;47:533–543. [PubMed] [Google Scholar]
- IMS, 2011. The use of medicines in the United States: review of 2010, IMS Institute for healthcare informatics.
- IMS, 2011. The global use of medicines: outlook through 2015, IMS institute for healthcare informatics.
- Ives T.J., Bentz E.J., Gwyther R.E. Drug-related admissions to a family medicine service. Arch. Intern. Med. 1987;147:1117–1120. [PubMed] [Google Scholar]
- Johnson J.A., Bootman J.L. Drug-related morbidity and mortality: a cost of illness model. Arch. Intern. Med. 1995;155:1949–1956. [PubMed] [Google Scholar]
- Juntti-Patinen L., Kuitunen T., Pere P., Neuvonen P.J. Drug-related visits to a district hospital emergency room. Basic Clin. Pharmacol. Toxicol. 2006;98(2):212–217. doi: 10.1111/j.1742-7843.2006.pto_264.x. [DOI] [PubMed] [Google Scholar]
- Karch F.E., Lasagna L. Adverse drug reactions. A critical review. JAMA. 1975;12:1236–1241. [PubMed] [Google Scholar]
- Malhotra S., Karan R.S., Pandhi P., Jain S. Drug related medical emergencies in the elderly: role of adverse drug reactions and non compliance. Postgrad. Med. J. 2001;77(913):703–707. doi: 10.1136/pmj.77.913.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenney J.M., Harrison W.L. Drug-related hospital admissions. Am. J. Hosp. Pharm. 1976;33:792–795. [PubMed] [Google Scholar]
- Montamat S.C., Cusack B.J., Verstal R.E. Management of drug therapy in the elderly. N. Engl. J. Med. 1989;321:303–309. doi: 10.1056/NEJM198908033210507. [DOI] [PubMed] [Google Scholar]
- Nebeker J.R., Barach P., Samore M.H. Clarifying adverse drug events: a clinician’s guide to terminology, documentation, and reporting. Ann. Intern. Med. 2004;140:795–801. doi: 10.7326/0003-4819-140-10-200405180-00009. [DOI] [PubMed] [Google Scholar]
- Nelson K.M., Talbert R.L. Drug-related hospital admissions. Pharmacotherapy. 1996;16:701–707. [PubMed] [Google Scholar]
- Nolan L., O’Malley K. Prescribing for the elderly part I: sensitivity of the elderly to adverse drug reactions. J. Am. Geriatr. Soc. 1988;36:142–147. doi: 10.1111/j.1532-5415.1988.tb01785.x. [DOI] [PubMed] [Google Scholar]
- Office of Applied Studies, 2010. Substate estimates from the 2006–2008 national surveys on drug use and health. Rockville, MD: substance abuse and mental health services administration. Available at <http://oas.samhsa.gov/substate2k10/toc.cfm>.
- Patel P., Zed P.J. Drug-related visits to the emergency department: how big is the problem? Pharmacotherapy. 2002;22(7):915–923. doi: 10.1592/phco.22.11.915.33630. [DOI] [PubMed] [Google Scholar]
- Singh H., Kumar B.N. The incidence and nature of drug-related hospital admission: a 6-month observational study in a tertiary health care hospital. J. Pharmacol. Pharmacother. 2011;2(1):17–20. doi: 10.4103/0976-500X.77095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand L.M., Cipolle R., Morley P.C. Drug related problems: their structure and function. DICP Ann. Pharmacother. 1990;24:1093–1097. doi: 10.1177/106002809002401114. [DOI] [PubMed] [Google Scholar]
- Tom English. Drug-related problem: once A $76 6 billion headache, now a $ 177.4 billion migraine. Pharmacy Today. 2001;7(3) [Google Scholar]
- WHO (World Health Organization), 2008. Medicines: safety of medicines – adverse drug reactions. Fact sheet N 293.http://www.who.int/mediacentre/factsheets/fs293/en/.
- WHO, 2011. The world medicines situation report 3. utg. www.who.int/medicines/areas/policy/world_medicines_situation/en/index.html.
- Winterstein A.G., Sauer B.C., Helper C.D. Ann. Pharmacother. 2002;36:1238–1248. doi: 10.1345/aph.1A225. [DOI] [PubMed] [Google Scholar]
- Zed P.Z., Riyad B.A. Incidence, severity and preventability of medication-related visits to the emergency department: a prospective study. CMAJ. 2008;178(12):1563–1569. doi: 10.1503/cmaj.071594. [DOI] [PMC free article] [PubMed] [Google Scholar]



