Abstract
Background:
The societal consequences of drug abuse (DA) are severe and well documented, the World Health Organization recommending tracking of population trends for effective policy responses in treatment of DA and delivery of health care services. However, to correctly identify possible sources of DA change, one must first disentangle three different time-related influences on the need for treatment due to DA: age effects, period effects and cohort effects.
Methods:
We constructed our main Swedish national DA database (spanning four decades) by linking healthcare data from the Swedish Hospital Discharge Register to individuals, which included hospitalisations in Sweden for 1975-2010. All hospitalized DA cases were identified by ICD codes. Our Swedish national sample consisted of 3,078,129 men and 2,921,816 women. We employed a cross-classified multilevel logistic regression model to disentangle any net age, period and cohort effects on DA hospitalization rates.
Results:
We found distinct net age, period and cohort effects, each influencing the predicted probability ofhospitalisation for DA in men and women. Peak age for DA in both sexes was 33-35 years; net period effects showed an increase in hospitalisation for DA from 1996 to 2001; and in birth cohorts 1968-74, we saw a considerable reduction (around 75%) in predicted probability of hospitalisation for DA.
Conclusions:
The use of hospital admissions could be regarded as a proxy of the population's health service use for DA. Our results may thus constitute a basis for effective prevention planning, treatment and other appropriate policy responses.
Keywords: Sweden, drug abuse, age-period-cohort effects, longitudinal, trends
1. INTRODUCTION
The overall health, social and financial costs of drug abuse (DA) are well documented (United Nations Office on Drugs and Crime, 2012), with the World Health Organization (WHO) recommending tracking of population trends in DA for appropriate policy responses and effective prevention planning, treatment and delivery of health services (WHO, 2000).
A previous study compared the use of health services between chronic drug users and non-drug users and found that chronic drug users consumed significantly more inpatient and emergency care but less outpatient care relative to non-drug users. The same study also found that the total health care cost per individual was higher among chronic drug users (French et al., 2000). Another study found that chronic drug use in those aged 18-44 years who were admitted to hospital was 14% (Smothers and Yahr, 2005). This indicates that it is highly relevant to study hospital admissions in the context of DA, which was the purpose of the present study.
There are several individual and contextual predictors of hospital admissions for DA, such as ethnicity (Leao et al., 2006; Patterson et al., 1999), socioeconomic factors (Kendler et al., 2012), having health care insurance (DiCola et al., 2013; Santora and Hutton, 2008) and neighborhood characteristics (Kendler et al., 2013a; Sundquist and Frank, 2004). However, individual and contextual DA risk factors may exert different levels of influence in different time periods. Established DA monitoring agencies in the United States (Johnston et al., 2011) and Europe (European Monitoring Centre for Drugs and Drug Addiction, 2012) have reported fluctuations in DA over past decades, which make it difficult to predict the use of health services over time. It is, therefore, important to disentangle three different time-related influences: age effects, period effects and cohort effects.
Age effects reflect variation in risk of DA attributable to the ageing process. Conversely, period effects reflect variations in risk of DA that influence all age groups simultaneously, e.g., period-specific changes in the popularity and availability of substances of abuse (Nyabadza and Hove-Musekwa, 2010; Smith, 2006; Yu, 2012). Finally, cohort effects reflect variation in risk of DA among individuals who are defined by some shared historical experience, such as year or decade of birth.
The three time-related influences are not independent and are inherently confounded (Degenhardt et al., 2008; Holdcraft and Iacono, 2004; Mason et al., 1973; Roxburgh et al., 2010). The most appropriate solution is, therefore, to consider all three effects simultaneously by performing an Age-Period-Cohort analysis (Smith, 2008).
Only three studies have employed Age-Period-Cohort analyses in the field of DA, all focusing on only one specific substance (marijuana) and utilising national cross-sectional survey data (Kerr et al., 2007; Miech and Koester, 2012; Piontek et al., 2012). However, survey data can be inherently biased (Johnson and Fendrich, 2005), especially when estimating health care use among individuals with DA. There is therefore a need for studies using relevant proxies for health care use for DA, such as hospital admissions.
In Sweden, data from multiple nationwide registries and healthcare data can be linked via the unique 10-digit personal identification number assigned at birth (or immigration) to all Swedish residents. This has enabled the creation of a unique Swedish national-level DA dataset, spanning many decades and avoiding the problems of reporting bias common to survey-based data (Kendler et al., 2013b, 2012). However, results obtained from registry-based data used in age-period-cohort analyses are only valid if assessment of the outcome under investigation is also stable, accurate and complete over time. Of all the Swedish DA data available, only the Hospital Discharge Register fulfils these criteria. It contains data on all individual hospital admissions from all regions in Sweden and spans over four decades. The use of hospital admissions is a relevant proxy of the population’s health service use for DA, which may constitute a basis for effective prevention planning, treatment and other appropriate anti-DA policy responses (WHO, 2000).
The aim of this study was to investigate the net effects of age, period and cohort on overall DA hospitalization rates within the total Swedish population, from 1975 to 2010. We hypothesised that the net effect of age on DA hospitalization rates would be strongest in young adults, with rates later declining in line with age-related psychological and sociological life course changes. We further hypothesised that DA hospitalization rates would be influenced by significant net period effects, as changes (for example) in substance popularity or national health policy occurred over time. As this study spanned four decades, we also expected to identify net birth cohort effects on DA hospitalization rates.
2. METHODS
We formed our database from the national Swedish Hospital Discharge Register, linking them to individuals using Swedish 10-digit personal ID numbers. We identified DA cases using main and secondary diagnosis ICD codes (ICD8: Drug dependence (304); ICD9: Drug psychoses (292) and Drug dependence (304); and ICD10: Mental and behavioural disorders due to psychoactive substance use (F11-F19), excluding alcohol (F10) or tobacco (F17)). This study was approved on 30th November 2011 by the Regional Ethical Review Board in Lund, Sweden (approval no. 2011/675).
2.1 Sample
We based all Age-Period-Cohort analyses on individuals aged fifteen years or more, born between 1950 and 1994. We divided the population into fifteen three-year birth cohorts (1950-1952, 1953-1955 … 1992-1994). We also created twelve three-year periods (1975-1977, 1978-1980… 2008-2010) within which to estimate our overall DA hospitalization rates. Individuals born in the first five cohorts had the potential to be recorded as drug abusers across all twelve periods; individuals born in the last birth cohort (1992-1994) across the final two periods only. For each period, we estimated a three-year DA hospitalization rate within each birth cohort from hospital discharge diagnoses that contained any of the ICD codes previously described. As past DA research has identified that men are approximately twice more likely to use and abuse illicit substances than women (Fothergill and Ensminger, 2006; Hicks et al., 2007; Kloos et al., 2009; Wetherington, 2007), we stratified our sample according to gender.
In total, we had 48,267,747 observations from the total Swedish population: 24,734,203 for males and 23,533,544 for females. For each of the twelve periods, we calculated the age of each individual as the ‘middle’ period year minus the year of birth. For example, in period 2 (1978-1980), a person born in 1950 would be considered aged 29 years (their age in year 1979). Individuals had to be alive at the beginning of each period in order to be included in the analyses for that period.
2.2 Statistical analysis
We used a cross-classified multilevel logistic regression model to disentangle the Age-Period-Cohort effects (Fielding and Goldstein, 2006; Yang and Land, 2008) with age being the only fixed effect. Such a model comprises observations nested within a cross-classification of two different hierarchies and takes into account any ‘cohort’ and ‘period’ influences on DA. We estimated two variance components, one for period and one for cohort. We addressed the linear dependency problem (Mason et al., 1973) by including a non-linear (quadratic) age effect in the model (‘age squared’).
We present the variance components attributed to the different classifications and the sum of the two variance components, together with a 95% credible interval (CI), as the intraclass correlation (ICC). The ICC measures the correlation between the responses of individuals from the same period/cohort, and may be interpreted as the proportion of the total residual variation in DA that is due to differences between periods and/or cohorts. We calculated the ICC using the latent variable method (Snijders and Busker, 1999), which assumes the existence of a latent individual variable that follows a logistic distribution with a variance equal to 3.29 (π2 ÷ 3).
As the number of observations exceeded 24 million for each gender, we took a random 10% sample for the estimation process. We repeated our analyses using a further three random 10% samples to ensure the robustness of our results. All statistical analyses were performed using SAS 9.2 (SAS Institute Inc, 2008) and MLwiN (Rasbash et al., 2012).
An ancillary analysis was performed to disentangle net age, period and cohort effects using all available Swedish DA data sources (see supplemental material) in an attempt to reflect the overall need for treatment for DA in the Swedish population over four decades.
3. RESULTS
The estimated hospitalization rates for DA across each birth cohort and period, stratified by sex, is shown in Tables 1a and 1b as percentages. Patterns of hospitalization rates within each cohort over the thirteen study periods relate to the age curves shown in Fig.1. Hospitalization rates for DA will below, in some cases, be referred to as only “DA”.
Table 1a.
Percentages of the Swedish male population hospitalized for DA for different birth cohorts across different time periods
| Period |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | 1975-77 | 1978-80 | 1981-83 | 1984-86 | 1987-89 | 1990-92 | 1993-95 | 1996-98 | 99-2001 | 2002-04 | 2005-07 | 2008-10 |
| 1950-1952 | 0.39 | 0.31 | 0.27 | 0.27 | 0.27 | 0.28 | 0.28 | 0.32 | 0.31 | 0.25 | 0.23 | 0.20 |
| 1953-1955 | 0.35 | 0.36 | 0.30 | 0.34 | 0.37 | 0.36 | 0.39 | 0.42 | 0.40 | 0.36 | 0.29 | 0.29 |
| 1956-1958 | 0.20 | 0.27 | 0.32 | 0.34 | 0.39 | 0.39 | 0.43 | 0.49 | 0.46 | 0.40 | 0.37 | 0.36 |
| 1959-1961 | 0.05 | 0.11 | 0.23 | 0.28 | 0.36 | 0.40 | 0.40 | 0.52 | 0.50 | 0.45 | 0.40 | 0.41 |
| 1962-1964 | 0 | 0.02 | 0.10 | 0.20 | 0.31 | 0.39 | 0.42 | 0.52 | 0.52 | 0.45 | 0.42 | 0.42 |
| 1965-1967 | . | 0 | 0.02 | 0.08 | 0.17 | 0.28 | 0.33 | 0.42 | 0.45 | 0.41 | 0.38 | 0.40 |
| 1968-1970 | . | . | 0 | 0.01 | 0.08 | 0.16 | 0.24 | 0.35 | 0.39 | 0.38 | 0.34 | 0.37 |
| 1971-1973 | . | . | . | 0 | 0.03 | 0.11 | 0.19 | 0.33 | 0.38 | 0.36 | 0.37 | 0.37 |
| 1974-1976 | . | . | . | . | 0 | 0.05 | 0.12 | 0.32 | 0.43 | 0.44 | 0.43 | 0.45 |
| 1977-1979 | . | . | . | . | . | 0 | 0.06 | 0.28 | 0.51 | 0.52 | 0.55 | 0.58 |
| 1980-1982 | . | . | . | . | . | . | 0 | 0.10 | 0.38 | 0.53 | 0.63 | 0.68 |
| 1983-1985 | . | . | . | . | . | . | . | 0.01 | 0.14 | 0.36 | 0.57 | 0.70 |
| 1986-1988 | . | . | . | . | . | . | . | . | 0.02 | 0.12 | 0.43 | 0.72 |
| 1989-1991 | . | . | . | . | . | . | . | . | . | 0.01 | 0.15 | 0.51 |
| 1992-1994 | . | . | . | . | . | . | . | . | . | . | 0.02 | 0.20 |
Table 1b.
Percentages of the Swedish female population hospitalized for DA for different birth cohorts across different time periods
| Period |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | 1975-77 | 1978-80 | 1981-83 | 1984-86 | 1987-89 | 1990-92 | 1993-95 | 1996-98 | 99-2001 | 2002-04 | 2005-07 | 2008-10 |
| 1950-1952 | 0.13 | 0.10 | 0.11 | 0.12 | 0.10 | 0.10 | 0.10 | 0.19 | 0.21 | 0.18 | 0.14 | 0.12 |
| 1953-1955 | 0.16 | 0.13 | 0.14 | 0.13 | 0.13 | 0.13 | 0.13 | 0.22 | 0.25 | 0.20 | 0.18 | 0.14 |
| 1956-1958 | 0.13 | 0.14 | 0.14 | 0.14 | 0.13 | 0.16 | 0.16 | 0.24 | 0.28 | 0.23 | 0.21 | 0.20 |
| 1959-1961 | 0.05 | 0.09 | 0.11 | 0.11 | 0.13 | 0.13 | 0.15 | 0.26 | 0.30 | 0.25 | 0.24 | 0.21 |
| 1962-1964 | 0.01 | 0.02 | 0.07 | 0.09 | 0.11 | 0.14 | 0.15 | 0.24 | 0.28 | 0.26 | 0.23 | 0.25 |
| 1965-1967 | . | 0 | 0.02 | 0.06 | 0.10 | 0.12 | 0.14 | 0.22 | 0.25 | 0.24 | 0.23 | 0.24 |
| 1968-1970 | . | . | 0 | 0.02 | 0.07 | 0.07 | 0.09 | 0.17 | 0.22 | 0.21 | 0.18 | 0.20 |
| 1971-1973 | . | . | . | 0 | 0.03 | 0.07 | 0.09 | 0.18 | 0.21 | 0.20 | 0.19 | 0.20 |
| 1974-1976 | . | . | . | . | 0.01 | 0.03 | 0.07 | 0.19 | 0.24 | 0.20 | 0.17 | 0.20 |
| 1977-1979 | . | . | . | . | . | 0.01 | 0.04 | 0.21 | 0.30 | 0.26 | 0.23 | 0.23 |
| 1980-1982 | . | . | . | . | . | . | 0.01 | 0.10 | 0.31 | 0.34 | 0.29 | 0.28 |
| 1983-1985 | . | . | . | . | . | . | . | 0.02 | 0.18 | 0.34 | 0.35 | 0.37 |
| 1986-1988 | . | . | . | . | . | . | . | . | 0.04 | 0.18 | 0.38 | 0.43 |
| 1989-1991 | . | . | . | . | . | . | . | . | . | 0.04 | 0.21 | 0.43 |
| 1992-1994 | . | . | . | . | . | . | . | . | . | . | 0.04 | 0.20 |
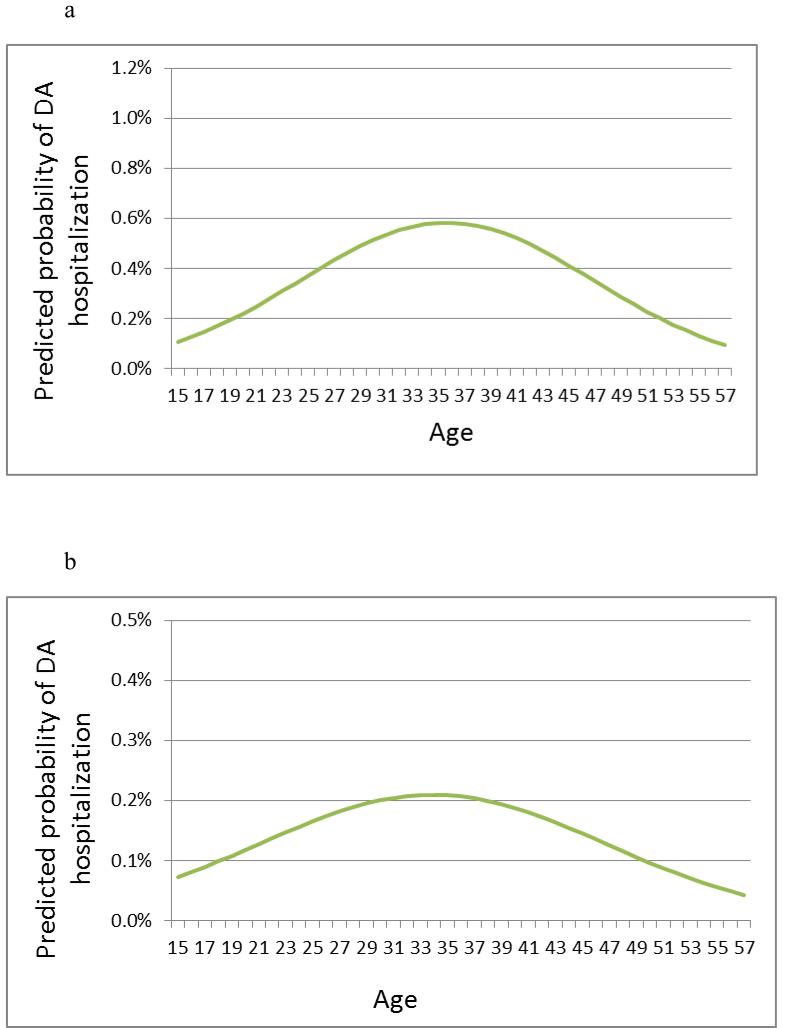
Figure 1.
Predicted probability of hospitalization for DA by age. (a) Men. (b) Women.
3.1 Net Age effects
3.1.1 Men
The net effects of centred ‘age’ and ‘age-squared’ on DA are shown in Table 2 as odds ratios (ORs). ‘Age’ was positively associated with DA, whereas the quadratic term was negatively associated (OR = 1.062 and 0.996, respectively). These ORs correspond to the predicted probability curve shown in Figure 1a, which represents the total net effect of age on overall DA hospitalization rates during the study period (1975-2010) for all men born in Sweden in 1950-94. The predicted probability is about 0.1% at 15 years of age, rising steadily to 0.6% by age 35 before steadily declining, i.e. 0.6% of all Swedish men aged 35 years are recorded for hospitalization due to DA.
Table 2.
Results from cross-classified multilevel regression analysis of net effects of age, period and cohort on hospitalization for DA in Swedish men and women (1975-2010)
| Males | Females | |
|---|---|---|
|
Fixed effects (Odds
Ratios) |
||
| Age (centred) | 1.062 (1.047-1.079) | 1.034 (1.018-1.054) |
| Age 2 | 0.996 (0.995-0.996) | 0.997 (0.997-0.997) |
| Random effects | ||
| Period | 0.045 (0.013-0.173) | 0.206 (0.067-0.637) |
| Cohort | 0.132 (0.052-0.396) | 0.147 (0.059-0.437) |
| ICC (%) | ||
| Period | 1.3 | 5.3 |
| Cohort | 3.8 | 4.2 |
| Period+Cohort | 5.1 | 9.5 |
3.1.2 Women
The net effects of age on DA in women are also shown in Table 2 as ORs, with similar patterns of association seen in women as in men (OR = 1.034 and 0.997, respectively).Figure 1b represents the total net effect of age on the predicted probability of DA hospitalization rates during the study period for all women born in Sweden in 1950-94; by 33 years of age, 0.2% of all Swedish women are recorded for hospitalization due to DA.
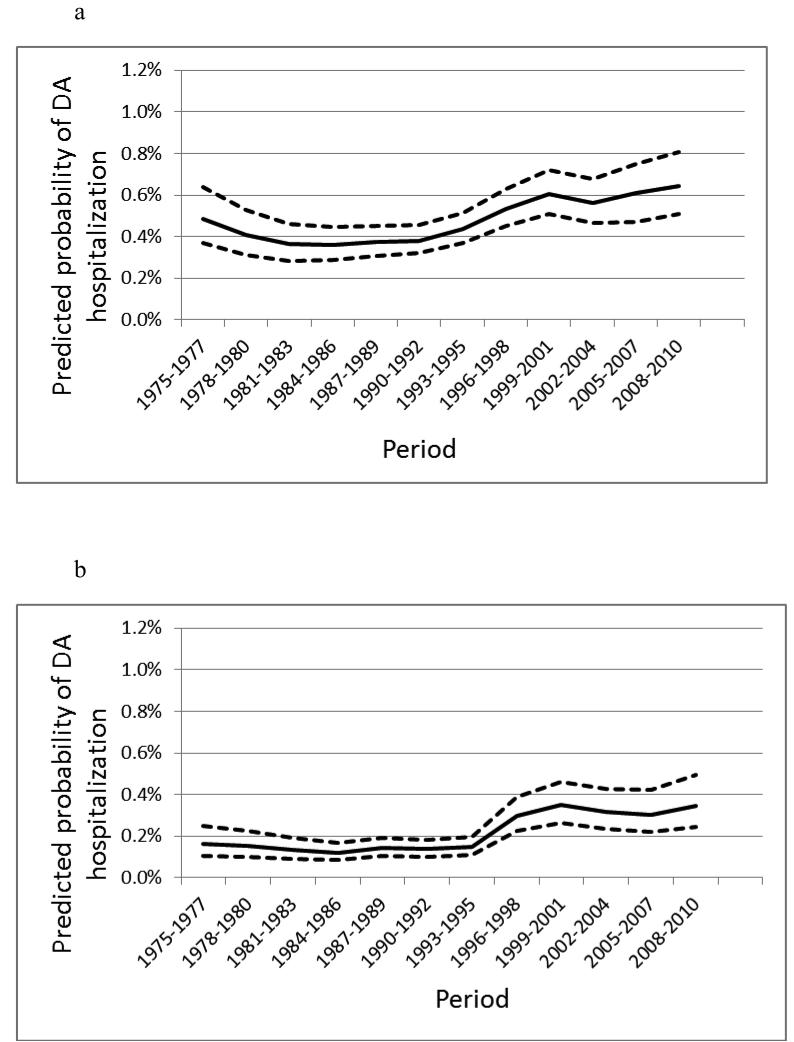
3.2 Net period effects
3.2.1 Men
Figure 2a shows that for men born in Sweden between 1950 and 1994, the predicted probability of hospitalization for DA was 0.5% in 1975. It declined to 0.35% by 1984 and then rose steadily to reach 0.6% by 2001. The curve remained relatively stable from this point until the end of the study period (2010). Period (and cohort) effects were treated as random effects in the model, the variance component being partitioned accordingly. The ICC for net period effects for men was 1.3% (see Table 2).
Figure 2.
Predicted probability of hospitalization for DA by period. (a) Men. (b) Women.
3.2.2 Women
Figure 2b shows the net period effects on DA hospitalization rates in women born in Sweden between 1950 and 1994. The predicted probability of DA hospitalization rates remained relatively stable for women (at 0.2%) from 1975 to 1995 and then rose to 0.3% by 2001; thereafter, DA hospitalization rates remained relatively stable. The ICC for net period effects for women was 5.3% (see Table 2).
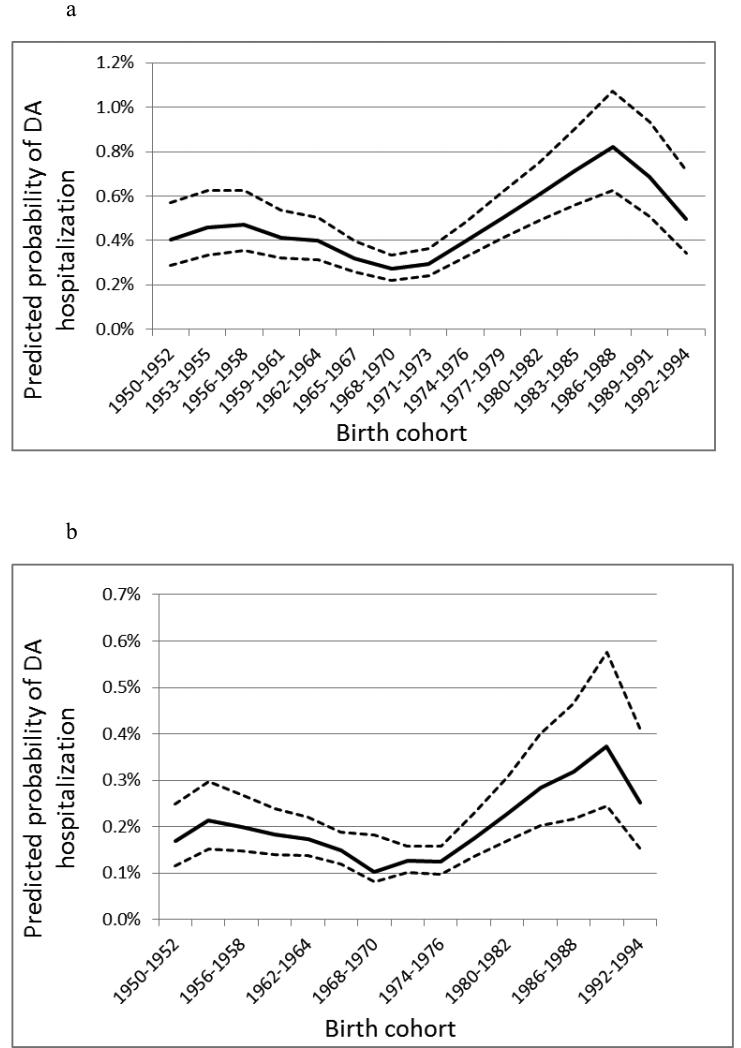
3.3 Net cohort effects
3.3.1 Men
Figure 3a shows that the predicted probability for DA hospitalization rates in Swedish men born in 1950-1958 was 0.4-0.5%. As new cohorts were born, this probability declined, reaching its lowest point (≈ 0.3%) for men born in 1968-1973. Men born to subsequent cohorts showed a steady rise in predicted probability, reaching a new peak of 0.8% for the 1986-1988 cohorts. This subsequently declined to 0.5% in the 1992-1994 cohort. The ICC for net male cohort effects was 3.8% (Table 2).
Figure 3.
Predicted probability of hospitalization for DA by birth cohort. (a) Men. (b) Women.
3.3.2 Women
As shown in Figure 3b, the predicted probability of DA hospitalization rates in all Swedish women born between 1950 and 1964 was 0.2%. This probability declined, reaching a low of ≈ 0.1% for 1968-1977 cohorts. In subsequent cohorts, there was a steady rise in DA hospitalization rates, peaking at 0.4% for the 1988-1991 birth cohort. The curve showed a decline to 0.3% for the last cohort (1992-1994). The ICC for net female cohort effects was 4.2% (Table 2).
3.4 Ancillary analysis
The results of Age-Period-Cohort analyses of all available Swedish DA data are shown as supplementary material (Tables S1a-b and S2, plus Figs. S1a-b, S2a-b and S3a-b1). All curves were similar to those described above, with predicted probability percentages being somewhat augmented, as expected when using a greater number of DA data sources. The peak age for registration due to DA was lower for men (now 31 years). There was a noticeably steeper rise in the period effects curve from 1997 compared with the two-register analysis. The cohort effect curves maintained their U shape.
4. DISCUSSION
The aim of this study was to investigate the net effects of age, period and cohort on overall DA hospitalization rates, used as a proxy for health care use for DA, from 1975 – 2010 across the total Swedish population in cohorts born in 1950-1994.
4.1 Age, period and cohort effects
We found a distinct net effect of age, with the probability of DA hospitalization steadily declining as age increased over 35 years. The results fall in line with suggested age effects found in most previous studies on DA (European Monitoring Centre for Drugs and Drug Addiction, 2011, 2012; Kerr et al., 2007; Miech and Koester, 2012; Perkonigg et al., 2006; Piontek et al., 2012; Chen and Kandel, 1995; Robins, 1980).
There were also period effects. The predicted probability for being hospitalized for DA in Sweden remained steady between 1975 and 1996. Around 1997, however, the predicted probability rose and then plateaued again by 2001 in both genders. The rise in the period curve coincided with a changeover of ICD9 to ICD10 codes in 1997, which could partly explain this rise. However, the severe economic recession experienced by Sweden at the beginning of the 1990s was followed by a reduction in anti-DA programmes and projects (SOU, 2000; United Nations Office on Drugs and Crime, 2007). Despite difficulties establishing ‘…a direct and causal relationship between policy measures and results’ (United Nations Office on Drugs and Crime, 2007), it is noteworthy that the rise in predicted probability in DA hospitalization seen from the mid-1990s onwards coincides with the economic crisis in Sweden and the demotion of the drug issue as a political priority (SOU, 2000). Sweden joining the European Union in 1995 is another period effect, which could have led to an increase in the influx of illicit substances (Garoupa, 1997).
Those individuals belonging to the 1968-1974 birth cohorts had the lowest predicted probabilities for DA hospitalization. Compared to subsequent birth cohorts, this represents a drop of 75% for both sexes between 1968 and 1974. Sweden’s own drug surveillance agency (Centralförbundet för alkohol- och narkotikaupplysning - ‘CAN’) supports our findings, reporting a drop of over 50% in overall DA in 16-19 year-old high school students between 1984 and 1994 (Centralförbundet för alkohol- och narkotikaupplysning, 2012), these same students belonging to the 1968-1976 birth cohorts. Other sources also report reductions in DA among 15-16-year-old Swedish students between 2002 and 2007 (Centralförbundet för alkohol- och narkotikaupplysning, 2012; United Nations Office on Drugs and Crime, 2007). However, latter cohorts may not have had the sufficient time to develop drug problems that could lead to hospital admission due to DA, which makes the results for latter cohorts more uncertain.
4.2 Health care use and DA
Although a few studies and reports have focused on age, period, and cohort effect on DA, this is the first study to the best of our knowledge that has examined age, period, and cohort effects on health care use for DA, measured by hospitalizations. We judged that hospitalizations would be the most relevant measure in the assessment of these effects, as several previous studies have shown that individuals with DA consume inpatient and emergency care to a larger extent than outpatient care (French et al., 2000). In addition, chronic drug use is relatively common among those aged 18-44 years who are admitted to hospital (Smothers and Yahr, 2005). Our findings represent a novel contribution as they indicate that health care use for DA is influenced by age, period and cohort effects. They are therefore useful for health care planning and preventive measures in different age groups and cohorts.
Previous research on health care use and the cost of medical care for DA is scarce in comparison with the literature on predictors and consequences of DA (Alexandre et al., 2001; French et al., 2001). However, studies on health care use for DA are important as they can provide clues for effective preventive measures. For example, individuals with DA tend to seek emergency care to a higher extent than outpatient care. This provides a significant opportunity for hospitals to recognize and refer drug users to relevant preventive and outpatient care. The underlying mechanisms behind drug users’ health seeking behaviour may be explained by several reasons. One is that some health care providers may not regard DA as a chronic health condition (Rivers et al., 1999). Another plausible reason is that persons with DA may not prioritize their need of health care until their condition is in the need of emergency services. Policies that support inexpensive and accessible outpatient care for drug users may sometimes help stopping medical conditions from becoming more severe and in the need of hospital care. However, more research is needed on this topic.
4.3 Strengths and limitations
A major strength of our study is its annual sampling of a national population from 1975-2010 and the employment of multiple data sources in the ancillary analysis to reflect the overall need for treatment for DA. Our hospital data are nearly 100% complete for DA diagnoses from 1975 to 2010. For all hospitalisations, only 0.4% of personal identification numbers and 0.9% of all main diagnoses were missing. This enabled us to perform the most comprehensive Age-Period-Cohort study in the field of DA hospitalizations to date. Despite this, there are several limitations of our study that should also be discussed.
While using registry data has the important advantage of not requiring accurate respondent recall and reporting, the risk for time-dependent bias due to registry effects remains. In addition, only a subset of individuals who are drug abusers would ever require medical treatment for DA, which means that hospitalizations alone do not capture the actual need of medical treatment for DA in the population. Use of different data sources also implies that findings from different studies are not directly comparable (Olsson et al., 2001; Folkhälsoinstitut, 2010). Our aim was to investigate overall DA hospitalization rates (as opposed to any substance-specific outcomes) across Sweden over four decades. Despite previous research showing a large amount of sharing of risk factors across different drugs of abuse (Kendler et al., 2003), our combined DA outcome may have introduced certain time-dependent bias, as substance popularity and/or availability is likely to have varied over four decades. For example, times when the use of amphetamines or opiates was more popular could result in more hospitalisations than during times when cannabis was the more popular/more available substance (Arendt et al., 2011). Furthermore, as the natural history of DA and its longer-term consequences varies depending on substance of choice (Chen and Kandel, 1995; Hser et al., 2001), our combined DA measure would not capture any of these differences. A further limitation is our assumption that age, period and cohort are the only temporal considerations regarding DA hospitalizations. In reality, the situation is probably much more complex, with possible modifications of specific effects over time.
4.4 Conclusions
Our study is the only Age-Period-Cohort drug abuse study to date that annually has sampled a total population over four decades. Our results reveal unique net effects of age, period and cohort on overall health care use for DA, defined as hospitalization rates. Based on our results, current and future policy may further benefit from new initiatives in order to achieve a reduction in overall DA hospitalization rates.
Supplementary Material
Acknowledgements
This work was supported by grants from the National Institute of Drug Abuse (R01 DA030005), the Swedish Research Council (2012-2378 (awarded to JS), K2009-70X-15428-05-3 (KS) and K2012-70X-15428-08-3 (KS)), the Swedish Council for Working Life and Social Research (2007-1754 (JS)) and the Swedish Council for Information on Alcohol and Other Drugs (KS), as well as ALF funding from Region Skåne awarded to JS and KS.
Role of Funding Source: Funding for this study was provided by NIDA Grant R01 DA030005, the Swedish Research Council Grant 2012-2378MH and K2012-70X-15428-08-3, and the Swedish Council for Working Life and Social Research Grant 2007-1754; the aforementioned bodies had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors: Giuseppe N. Giordano, Henrik Ohlsson, Kenneth Kendler, Marilyn Winkleby, Kristina Sundquist and Jan Sundquist. Authors KK and HO designed the study and wrote the protocol. Author GNG managed the literature searches and summaries of previous related work. Authors KS and JS provided all data sources. Author HO undertook the statistical analysis, and authors GNG and HO wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest: No conflict declared
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
REFERENCES
- Alexandre PK, Roebuck MC, French MT, Chitwood DD, McCoy CB. Problem drinking, health services utilization, and the cost of medical care. Rec. Dev. Alcohol. 2001;15:285–298. doi: 10.1007/978-0-306-47193-3_16. [DOI] [PubMed] [Google Scholar]
- Arendt M, Munk-Jorgensen P, Sher L, Jensen SO. Mortality among individuals with cannabis, cocaine, amphetamine, MDMA, and opioid use disorders: a nationwide follow-up study of Danish substance users in treatment. Drug Alcohol Depend. 2011;114:134–139. doi: 10.1016/j.drugalcdep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- Centralförbundet för alkohol- och narkotikaupplysning . Drug tendencies in Sweden 2011. Stockholm: 2012. p. 93. Drogutvecklingen i Sverige 2011. [Google Scholar]
- Chen K, Kandel DB. The natural-history of drug-use from adolescence to the mid-thirties in a general-population sample. Am. J. Public Health. 1995;85:41–47. doi: 10.2105/ajph.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Chiu W-T, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, de Girolamo G, Gureje O, Huang Y, Karam A, Kostyuchenko S, Lepine JP, Mora MEM, Neumark Y, Ormel JH, Pinto-Meza A, Posada-Villa J, Stein DJ, Takeshima T, Wells JE. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. Plos Med. 2008;5:1053–1067. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiCola LA, Gaydos LM, Druss BG, Cummings JR. Health insurance and treatment of adolescents with co-occurring major depression and substance use disorders. J. Am. Acad. Child Adolesc. Psychiatry. 2013;52:953–960. doi: 10.1016/j.jaac.2013.06.012. [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction . Annual Report on the State of the Drugs Problem in Europe. Lisbon: 2011. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction . Annual Report on the State of the Drugs {roblem in Europe. Lisbon: 2012. http://www.emcdda.europa.eu/publications/searchresults?action=list&type=PUBLICATIONS&SERIES_PUB=w36.accessed on 17th October 2012>. [Google Scholar]
- Fielding A, Goldstein H. Cross-Classified and Multiple Membership Structures in Multilevel Models: An Introduction and Review. DfES Publications; Nottingham, UK: 2006. [Google Scholar]
- Folkhälsoinstitut S. Narkotikabruket i Sverige (Drug use in Sweden) Östersund, Sweden: 2010. p. 16. [Google Scholar]
- Fothergill KE, Ensminger ME. Childhood and adolescent antecedents of drug and alcohol problems: a longitudinal study. Drug Alcohol Depend. 2006;82:61–76. doi: 10.1016/j.drugalcdep.2005.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French MT, McGeary KA, Chitwood DD, McCoy CB. Chronic illicit drug use, health services utilization and the cost of medical care. Soc. Sci. Med. 2000;50:1703–1713. doi: 10.1016/s0277-9536(99)00411-6. [DOI] [PubMed] [Google Scholar]
- French MT, Roebuck MC, McGeary KA, Chitwood DD, McCoy CB. Using the drug abuse screening test (DAST-10) to analyze health services utilization and cost for substance users in a community-based setting. Subst. Use Misuse. 2001;36:927–946. doi: 10.1081/ja-100104096. [DOI] [PubMed] [Google Scholar]
- Garoupa N. Optimal law enforcement and the economics of the drug market: some comments on the Schengen Agreements. Intl. Rev. Law Econ. 1997;17:521–535. [Google Scholar]
- Hicks BM, Blonigen DM, Kramer MD, Krueger RF, Patrick CJ, Iacono WG, McGue M. Gender differences and developmental change in externalizing disorders from late adolescence to early adulthood: a longitudinal twin study. J. Abnorm. Psychol. 2007;116:433–447. doi: 10.1037/0021-843X.116.3.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holdcraft LC, Iacono WG. Cross-generational effects on gender differences in psychoactive drug abuse and dependence. Drug Alcohol Depend. 2004;74:147–158. doi: 10.1016/j.drugalcdep.2003.11.016. [DOI] [PubMed] [Google Scholar]
- Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch. Gen. Psychiatry. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- Johnson T, Fendrich M. Modeling sources of self-report bias in a survey of drug use epidemiology. Ann. Epidemiol. 2005;15:381–389. doi: 10.1016/j.annepidem.2004.09.004. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2010: Volume I, Secondary School Students. Institute for Social Research; Ann Arbor: 2011. [Google Scholar]
- Kendler KS, Maes HH, Sundquist K, Ohlsson H, Sundquist J. Genetic and family and community environmental effects on drug abuse in adolescence: a Swedish National Twin and Sibling Stud. Am. J. Psychiatry. 2013a;30:12101300. doi: 10.1176/appi.ajp.2013.12101300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Ohlsson H, Sundquist K, Sundquist J. Within-family environmental transmission of drug abuse: a Swedish National Study. JAMA Psychiatry. 2013b;70:235–242. doi: 10.1001/jamapsychiatry.2013.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch. Gen. Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Sundquist K, Ohlsson H, Palmer K, Maes H, Winkleby MA, Sundquist J. Genetic and familial-environmental influences on risk for drug abuse: a National Swedish Adoption Study. Arch. Gen. Psychiatry. 2012;69:690–697. doi: 10.1001/archgenpsychiatry.2011.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age-period-cohort influences on trends in past year marijuana use in the US from the 1984, 1990, 1995 and 2000 National Alcohol Surveys. Drug Alcohol Depend. 2007;86:132–138. doi: 10.1016/j.drugalcdep.2006.05.022. [DOI] [PubMed] [Google Scholar]
- Kloos A, Weller RA, Chan R, Weller EB. Gender differences in adolescent substance abuse. Curr. Psychiatry Rep. 2009;11:120–126. doi: 10.1007/s11920-009-0019-8. [DOI] [PubMed] [Google Scholar]
- Leao TS, Johansson LM, Sundquist K. Hospitalization due to alcohol and drug abuse in first- and second-generation immigrants: a follow-up study in Sweden. Subst. Use Misuse. 2006;41:283–296. doi: 10.1080/10826080500409100. [DOI] [PubMed] [Google Scholar]
- Mason KO, Mason WM, Winsborough HH, Kenneth Poole W. Some methodological issues in cohort analysis of archival data. Am. Sociol. Rev. 1973;38:242–258. [Google Scholar]
- Miech R, Koester S. Trends in U.S., past-year marijuana use from 1985 to 2009: an age-period-cohort analysis. Drug Alcohol Depend. 2012;124:259–267. doi: 10.1016/j.drugalcdep.2012.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyabadza F, Hove-Musekwa SD. From heroin epidemics to methamphetamine epidemics: modelling substance abuse in a South African province. Math. Biosci. 2010;225:132–140. doi: 10.1016/j.mbs.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Olsson B, Wahren CA, Byqvist S. Det tunga narkotikamissbrukets omfattning i Sverige (The extent of heavy drug use in Sweden) Centralförbundet för alkohol- och narkotikaupplysning; Stockholm: 2001. [Google Scholar]
- Patterson KM, Holman CD, English DR, Hulse GK, Unwin E. First-time hospital admissions with illicit drug problems in indigenous and non-indigenous Western Australians: an application of record linkage to public health surveillance. Aust. N. Z. J. Public Health. 1999;23:460–463. doi: 10.1111/j.1467-842x.1999.tb01298.x. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Pfister H, Hoefler M, Froehlich C, Zimmermann P, Lieb R, Wittchen H-U. Substance use and substance use disorders in a community sample of adolescents and young adults: incidence, age effects and patterns of use. Eur. Addict. Res. 2006;12:187–196. doi: 10.1159/000094421. [DOI] [PubMed] [Google Scholar]
- Piontek D, Kraus L, Pabst A, Legleye S. An age-period-cohort analysis of cannabis use prevalence and frequency in Germany. J. Epidemiol. Community Health. 2012;1990-2009;66:908–913. doi: 10.1136/jech-2011-200180. [DOI] [PubMed] [Google Scholar]
- Rasbash J, Charlton C, Browne W, Healy M, Cameron B. MLwiN Version 2.27. Centre for Multilevel Modelling, University of Bristol; 2012. [Google Scholar]
- Rivers JE, Komaroff E, Kibort AC. Access to health and human services for drug users: an urban/rural community systems perspective. Subst. Use Misuse. 1999;34:707–725. doi: 10.3109/10826089909037239. [DOI] [PubMed] [Google Scholar]
- Robins LN. The natural history of drug abuse Acta Psychiatr. Scand. 1980;62:7–20. doi: 10.1111/j.1600-0447.1980.tb10426.x. [DOI] [PubMed] [Google Scholar]
- Roxburgh A, Hall WD, Degenhardt L, McLaren J, Black E, Copeland J, Mattick RP. The epidemiology of cannabis use and cannabis-related harm in Australia 1993-2007. Addiction. 2010;105:1071–1079. doi: 10.1111/j.1360-0443.2010.02903.x. [DOI] [PubMed] [Google Scholar]
- Santora PB, Hutton HE. Longitudinal trends in hospital admissions with co-occurring alcohol/drug diagnoses, 1994-2002. J. Subst. Abuse Treat. 2008;35:1–12. doi: 10.1016/j.jsat.2007.08.002. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc . SAS ONLINE DOC Version 9.3. SAS Institute Inc; Cary, NC: 2008. [Google Scholar]
- Smith DE. An upper/downer perfect storm: the coming world-wide drug epidemic. J. Psychoactive Drugs. 2006;38:535–536. doi: 10.1080/02791072.2006.10400593. [DOI] [PubMed] [Google Scholar]
- Smith HL. Advances in age-period-cohort analysis. Sociol. Methods Res. 2008;36:287–296. [Google Scholar]
- Smothers BA, Yahr HT. Alcohol use disorder and illicit drug use in admissions to general hospitals in the United States. Am. J. Addict. 2005;14:256–267. doi: 10.1080/10550490590949433. [DOI] [PubMed] [Google Scholar]
- Snijders T, Busker R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modelling. Sage Publications; London: 1999. [Google Scholar]
- SOU Vägvalet - den narkotikapolitiska utmaningen - 'Crossroads - the drug policy challenge'. 2000. p. 33.
- Sundquist K, Frank G. Urbanization and hospital admission rates for alcohol and drug abuse: a follow-up study of 4.5 million women and men in Sweden. Addiction. 2004;99:1298–1305. doi: 10.1111/j.1360-0443.2004.00810.x. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime . Sweden’s Successful Drug Policy: A Review of the Evidence. New York: 2007. [Google Scholar]
- United Nations Office on Drugs and Crime . World Drug Report. New York: 2012. [Google Scholar]
- Wetherington CL. Sex-gender differences in drug abuse: a shift in the burden of proof? Exp. Clin. Psychopharmacol. 2007;15:411–417. doi: 10.1037/1064-1297.15.5.411. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Guide to Drug Abuse Epidemiology. Geneva: 2000. [Google Scholar]
- Yang Y, Land KC. Age-period-cohort analysis of repeated cross-section surveys - fixed or random effects? Sociol. Methods Res. 2008;36:297–326. [Google Scholar]
- Yu H-YE. The prescription drug abuse epidemic. Clin. Lab. Med. 2012;32:361–377. doi: 10.1016/j.cll.2012.06.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.