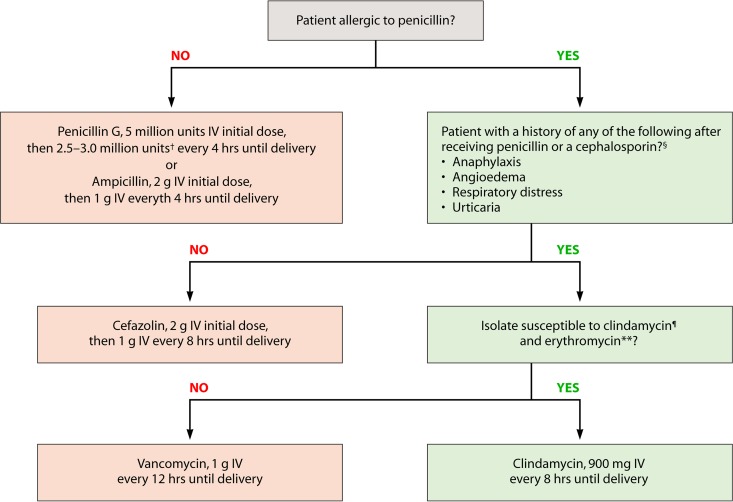
FIG 3.
CDC-recommended regimens for intrapartum antibiotic prophylaxis for prevention of early-onset GBS disease. IV, intravenously. *, broader-spectrum agents, including an agent active against GBS, might be necessary for treatment of chorioamnionitis. †, doses ranging from 2.5 to 3.0 million units are acceptable for the doses administered every 4 hours following the initial dose. The choice of dose within that range should be guided by which formulations of penicillin G are readily available to reduce the need for pharmacies to specially prepare doses. §, penicillin-allergic patients with a history of anaphylaxis, angioedema, respiratory distress, or urticaria following administration of penicillin or a cephalosporin are considered to be at high risk for anaphylaxis and should not receive penicillin, ampicillin, or cefazolin for GBS intrapartum prophylaxis. For penicillin-allergic patients who do not have a history of those reactions, cefazolin is the preferred agent because pharmacologic data suggest it achieves effective intra-amniotic concentrations. Vancomycin and clindamycin should be reserved for penicillin-allergic women at high risk for anaphylaxis.
 , if laboratory facilities are adequate, clindamycin and erythromycin susceptibility testing should be performed on prenatal GBS isolates from penicillin-allergic women at high risk for anaphylaxis. If no susceptibility testing is performed or the results are not available at the time of labor, vancomycin is the preferred agent for GBS intrapartum prophylaxis for penicillin-allergic women at high risk for anaphylaxis. **, resistance to erythromycin is often but not always associated with clindamycin resistance. If an isolate is resistant to erythromycin, it might have inducible resistance to clindamycin, even if it appears susceptible to clindamycin. If a GBS isolate is susceptible to clindamycin and resistant to erythromycin and testing for inducible clindamycin resistance has been performed and is negative (no inducible resistance), then clindamycin can be used for GBS intrapartum prophylaxis instead of vancomycin. (Adapted from reference 102.)
, if laboratory facilities are adequate, clindamycin and erythromycin susceptibility testing should be performed on prenatal GBS isolates from penicillin-allergic women at high risk for anaphylaxis. If no susceptibility testing is performed or the results are not available at the time of labor, vancomycin is the preferred agent for GBS intrapartum prophylaxis for penicillin-allergic women at high risk for anaphylaxis. **, resistance to erythromycin is often but not always associated with clindamycin resistance. If an isolate is resistant to erythromycin, it might have inducible resistance to clindamycin, even if it appears susceptible to clindamycin. If a GBS isolate is susceptible to clindamycin and resistant to erythromycin and testing for inducible clindamycin resistance has been performed and is negative (no inducible resistance), then clindamycin can be used for GBS intrapartum prophylaxis instead of vancomycin. (Adapted from reference 102.)