Abstract
Background
Europe is at the peak of an epidemic of malignant pleural mesothelioma and the burden of disease is likely to continue rising in the large areas of the world where asbestos remains unregulated. Patients with mesothelioma present with thoracic symptoms and radiological changes so respiratory physicians take a leading role in diagnosis and management. Belief that the modest survival times reported after radical surgery, whether alone or as part of multimodal therapy, are longer than they it would have been without surgery relies on data from highly selected, uncontrolled, retrospectively analysed case series. The only randomised study, the Mesothelioma and Radical Surgery (MARS) trial showed no benefit. A simple modelling study of registry patients, described here, shows that an impression of longer survival is eroded when patients who were never candidates for operation on grounds of histology, performance status and age are sequentially excluded from the model.
Conclusion
Whenever the question arises `Might an operation help me?' there are two responses that can and should be given. The first is that there is doubt about whether there is any survival or symptomatic benefit from surgery but we know that there is harm. The second is that there are on-going studies, including two randomised trials, which patients should be informed about. The authors suggest that the default position for clinicians should be to encourage recruitment into these trials.
Keywords: Mesothelioma, Thoracic Surgery
Europe is at the peak of an epidemic of malignant pleural mesothelioma1–3 and the burden of disease is likely to continue rising in the large areas of the world where asbestos remains unregulated.4 5 Respiratory physicians perforce take a lead role in diagnosis and management; patients with mesothelioma present with thoracic symptoms and radiological changes. Whenever the question arises ‘Might an operation help me?’ there are two responses that can and should be given. The first is that we are unsure whether there is any benefit from surgery but that there is harm. The second is that there are ongoing studies, including two randomised trials, which patients should be encouraged to learn more about.6
Two forms of extirpative surgery have been performed since the 1970s: extrapleural pneumonectomy (EPP) and lung sparing resection, now commonly referred to as pleurectomy decortication (P/D).6 They have been the subject of systematic reviews7 8 and the searches for each found 58 reports in the form of uncontrolled follow-up studies from which were selected 34 and 26 publications, respectively, for analysis of survival and perioperative data. These retrospective cohort studies are the commonest form of surgical reporting, providing survival data for a single surgeon or an institution's series of operations, but without control data for direct comparison. The review of EPP7 opens with a statement that overall survival is less than 12 months, citing a 1989 report of survival among patients diagnosed from 1965 to 19849 and a randomised trial of chemotherapy, which clearly states that the patients studied were not eligible for surgery.10 Setting the scene with inappropriate survival data, typically from another era, is characteristic of the scene setting introductions to these surgical reports. The implication that longer survival among the cohort of operated patients being reported is attributable to surgery neglects the fact that the operation was not a chance or random occurrence. Surgery is linked to a rigorous and well-informed process of patient selection. A disarmingly simple study illustrates the phenomenon.11
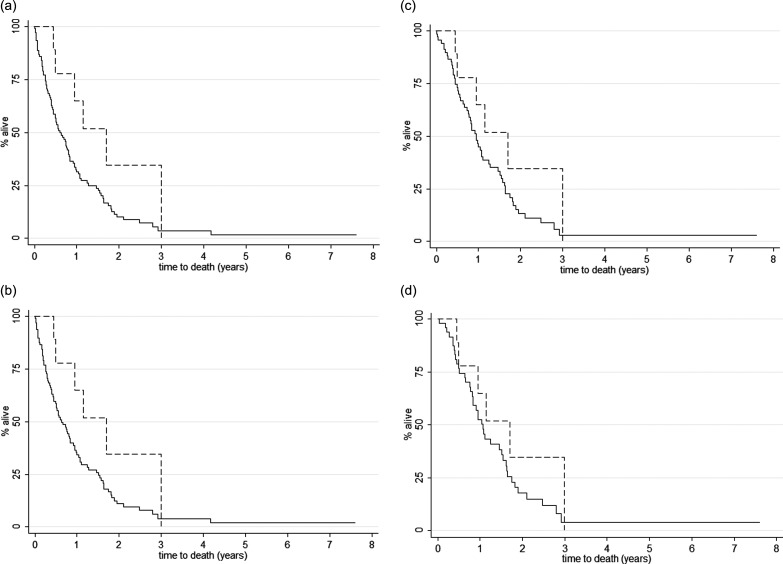
Ten patients had been selected to have EPP from among 123 patients diagnosed with mesothelioma between November 2002 and November 2011in the Cancer Registry of York Teaching Hospital, an area with a high and still increasing incidence.111 For all 123 patients, date of birth, date of diagnosis, histological diagnosis, performance status (PS), alive/dead status and date of death were retrievable from the registry. The Kaplan Meier (KM) survival estimate for the 10 patients who had EPP is shown in each successive graph (figure 1) accompanied by KM survival subsets of the 113 who did not have EPP, derived by stepwise exclusion of patients, recorded in the database, with characteristics that would have precluded them from having EPP (figure 1, table 1).
Figure 1.
In the York Cancer Registry 2002–2011, three factors know to be used in selection/exclusion of patients for cancer surgery were among the data fields: histological type, performance status (PS) and age. These were used to successively exclude patients who were not comparable with those selected to have surgery. Survival in patients having EPP, N=10 (dashed line) is compared to survival in: a) Patients not having EPP, N=113 (solid line); b) Patients without sarcomatoid histology not having EPP, N=102 (solid line); c) Patients without sarcomatoid histology and with PS 0 or 1 not having EPP, N=73 (solid line). Patients without sarcomatoid histology, with PS 0 or 1 and aged <76.2 years not having EPP, N=49 (solid line).
Table 1.
Stepwise exclusion of patients, recorded in the database, with characteristics which would have precluded EPP
| N | Median survival (Months) | IQR survival (Months) | |
|---|---|---|---|
| All Non-EPP | 113 | 6.1 | 2.2–12.8 |
| Excluding Sarcomatoid histology | 102 | 6.15 | 2.2–13.3 |
| Then excluding PS 2, 3 or 4* | 73 | 9.6 | 4.8–18.1 |
| Then excluding age >76.2 years | 49 | 11.4 | 5.9–19.4 |
| Patients who had EPP | 10 | 12.6 | 5.6–17.7 |
*Patients with PS missing are included.
EPP, extrapleural pneumonectomy; PS, performance status.
Step 1: Sarcomatoid histology is an adverse prognostic feature,12 and none of the patients operated had that pathology, so 11 patients with sarcomatoid histology have to be excluded from comparison.
Step 2: Poor PS (0–4 where 4 is worst) is a clinical reason for exclusion from major surgery within a trimodal package, including both high dose radiotherapy and chemotherapy.12 Only patients with known PS 0 or 1 were operated on, so a further 29 patients with documented PS 2, 3 or 4 should be excluded from comparison.
Step 3: The oldest patient having EPP was 76.2 years (an unusually advanced age for this surgery7), so a further 24 patients older than that age were next excluded from comparison.
It is thus evident that well over half the non-operated patients in York were never candidates for surgery on explicit criteria recorded in the database. Our exclusions are in each case conservative. If other factors available to those making the clinical decision, such as tumour bulk, invasiveness and lymph node involvement, had been balanced between the operated and non-operated patients, the narrowing gap in the survival analysis is likely to have diminished further.
In the Mesothelioma and Radical Surgery (MARS) trial in which patients were randomly allocated to have or to not have EPP the survival difference was in favour of not having surgery (HR 2.75). This was statistically unlikely to have been a chance finding (p=0.016).13 Note though that MARS was not a shot in the dark. From published data already available in 2004, it was evident that there was unlikely to be a large effect size in favour of EPP. The power calculation for the MARS trial was based on contemporary survival in non-operated patients14 and a systematic review of EPP at the time15 and 670 randomised patients were required to be reasonably sure of not missing a survival advantage attributable to EPP16 hence MARS opened as a feasibility study with the stated intent that the data would contribute to full trial if it went ahead. In the event, after 50 patients had been randomised, benefit from EPP appeared improbable. The admissibility of MARS as evidence (a small trial reporting results from its feasibility phase) has been contested17 18 and the criticisms rebutted19 20 and MARS is an instance of the Lilford maxim ‘some unbiased evidence is clearly better than none’.21
The debate has moved on. EPP cohort studies published in 2007–2009 reported median survival times of 10, 12, 13 and 14 months,22–25 while P/D has been associated with similar or better reported outcomes23 26 and less impairment of quality of life.27 We cannot be sure from the existing forms of evidence whether it is that P/D is more effective or that it is just less damaging, and hence, it is the subject of two trials.6 The European Organisation for Research and Treatment of Cancer (EORTC) will conduct a randomised trial in which all patients have both P/D and four cycles of neoadjuvant chemotherapy (cisplatin/pemetrexed). It is the sequence (surgery before vs surgery after chemotherapy) that is under test. This study is intended to evaluate which is safer and more feasible.6 It cannot test whether P/D offers benefits compared with no surgery since P/D is in both arms. The MARS-2 trial will address that question. It will investigate survival and patient reported outcomes with extended P/D following chemotherapy versus chemotherapy only.28
It will be some time before we have results from these trials. Meanwhile how can respiratory physicians best advise their patients? The National Collaborative Cancer Network Guidelines for Patients (‘an alliance of 21 of the world's leading cancer centers’) includes both P/D and EPP in its 2012 Guidelines for Patients.29 The International Mesothelioma Interest Group (IMIG) advise that surgical cytoreduction is indicated when macroscopic complete resection is deemed achievable and that the type of surgery (EPP or P/D) depends on clinical factors and on individual surgical judgment and expertise.18 The IMIG statement is under the heading ‘Clinical Guidelines’ but is in reality a position statement from the most eminent and experienced surgeons working with this cancer. Ten of the twelve IMIG authors are surgeons and 7 of their 10 citations are to IMIG conference abstracts, which feature uncontrolled follow-up studies of highly selected patients. The IMIG statement contrasts with recommendations from the Guidelines International Network (GIN) that there should be a balanced panel, a formal literature search, and objective and even-handed evaluation of evidence.30
Surgical follow-up studies are a form of reporting with many pitfalls.31 Only patients with most favourable disease characteristics and the best PS are able to pass through the multiple layers of referral and case selection. One further pitfall that leads to overoptimistic interpretation of follow-up studies where there is more than one treatment in sequence is that having subsequent treatment is conditional on surviving and being well enough after a previous treatment. The effect is revealed in an analysis32 of published data. Among 945 patients with mesothelioma,25 four groups were identified by ascending level of intervention: 387 had no surgery; 174 had a thoracotomy but no resection; 177 had resection but no adjuvant treatment; and 207 had resection as part of multimodality treatment. Mean survival was similar for the first three groups at 16.8, 17.8 and 17 months, respectively. Those who had surgery as part of multimodality treatment had a mean survival of 32.9 months but no part of the survival difference can be ascribed with certainty to any one of its components: increased survival is in part due to repeated selection of the fittest patients. A further concern is that in that practice, about one in five patients had thoracotomy without resection, which is in keeping with the IMIG position that the choice of operation depends on ‘individual surgical judgment and expertise’.25 In this very variable disease, we would prefer to have objective evidence of effectiveness.
It seems improbable that a P/D operation will ever remove all of the cancer if the more extensive EPP consistently fails to do so.33 This appears to be implicitly accepted in the phrase ‘macroscopic complete resection’ in the knowledge that there is a consistent finding of microscopic extension of mesothelioma to the resection margin.33 Nevertheless, the words curative and curative-intent appear repeatedly in the International Association for the Study of Lung Cancer mesothelioma database report,12 and when surveyed, a third of thoracic surgeons believed that cure was possible.34 Rena and Casadio (2011) observe ‘This is strange, considering that to date there is no report of a single patient surviving (malignant pleural mesothelioma).The problem is that the sense of the action ‘to cure’ is not clear to all or it is differently thought about in the thoracic surgeons community.’35
Does surgery provide net benefit with respect to pain, respiratory symptoms, quality of life and other patient reported outcomes? This information cannot be retrieved from the existing systematic reviews.7 8 A recent prospective study reported a substantial impairment of quality of life following surgery, worse for EPP than P/D, and only after P/D did quality of life return to baseline, and that took 12 months.27 Similar findings for respiratory function have now been reported.36 There appears to be a place for an approach in which treatment is moderated and in which the primary outcome shifts from survival to giving the patient the best remaining months or years.37 If patients are to be considered for surgery, given the lack of good quality evidence, recruitment into one or other of the two trials should be considered as the default position by respiratory physicians, surgeons and oncologists.38
Footnotes
Contributors: AD and RS devised the illustrative study. FF did the analysis. TT provided the first draft and final editing. FF and AD contributed to the development of the piece. RS received a HYMS Medical Student Bursary to present a preliminary report. TT was Chief Investigator of the Mesothelioma and Radical Surgery (MARS) trial. All authors agree with the final version.
Funding: Hull York Medical School Student Bursary to RS. FF is part funded by the British Heart Foundation.
Competing interests: None
Provenance and peer review: Not commissioned; internally peer reviewed.
Data sharing statement: The registry data used will be available on request.
References
- 1.Peto J, Hodgson JT, Matthews FE, et al. Continuing increase in mesothelioma mortality in Britain. Lancet 1995;345:535–9 [DOI] [PubMed] [Google Scholar]
- 2.La Vecchia C, Decarli A, Peto J, et al. An age, period and cohort analysis of pleural cancer mortality in Europe. Eur J Cancer Prev 2000;9:179–84 [PubMed] [Google Scholar]
- 3.Hodgson JT, McElvenny DM, Darnton AJ, et al. The expected burden of mesothelioma mortality in Great Britain from 2002 to 2050. Br J Cancer 2005;92:587–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsao AS, Wistuba I, Roth JA, et al. Malignant pleural mesothelioma. J Clin Oncol 2009;27:2081–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang X, Yano E, Qiu H, et al. A 37-year observation of mortality in Chinese chrysotile asbestos workers. Thorax 2012;67:106–10 [DOI] [PubMed] [Google Scholar]
- 6.Hiddinga BI, van Meerbeeck JP. Surgery in mesothelioma—where do we go after Mars? J Thorac Oncol 2013;8:525–9 [DOI] [PubMed] [Google Scholar]
- 7.Cao CQ, Yan TD, Bannon PG, et al. A systematic review of extrapleural pneumonectomy for malignant pleural mesothelioma. J Thorac Oncol 2010;5:1692–703 [DOI] [PubMed] [Google Scholar]
- 8.Teh E, Fiorentino F, Tan C, et al. A systematic review of lung-sparing extirpative surgery for pleural mesothelioma. J R Soc Med 2011;104:69–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruffie P, Feld R, Minkin S, et al. Diffuse malignant mesothelioma of the pleura in Ontario and Quebec: a retrospective study of 332 patients. J Clin Oncol 1989;7:1157–68 [DOI] [PubMed] [Google Scholar]
- 10.Vogelzang NJ, Rusthoven JJ, Symanowski J, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol 2003;21:2636–44 [DOI] [PubMed] [Google Scholar]
- 11.Smith R, Datta AK, Ten year follow up of mesothelioma in North Yorkshire. Thorax 2012:A150–A151 [Google Scholar]
- 12.Rusch VW, Giroux D, Kennedy C, et al. Initial analysis of the international association for the study of lung cancer mesothelioma database. J Thorac Oncol 2012;7:1631–9 [DOI] [PubMed] [Google Scholar]
- 13.Treasure T, Lang-Lazdunski L, Waller D, et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol 2011;12:763–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan C, Swift S, Gilham C, et al. Survival in surgically diagnosed patients with malignant mesothelioma in current practice. Thorax 2002;57iii:36 [Google Scholar]
- 15.Treasure T, Sedrakyan A. Pleural mesothelioma: little evidence, still time to do trials. Lancet 2004;364:1183–5 [DOI] [PubMed] [Google Scholar]
- 16.Treasure T, Waller D, Swift S, et al. Radical surgery for mesothelioma. BMJ 2004;328:237–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weder W, Stahel RA, Baas P, et al. The MARS feasibility trial: conclusions not supported by data. Lancet Oncol 2011;12:1093–4 [DOI] [PubMed] [Google Scholar]
- 18.Rusch V, Baldini EH, Bueno R, et al. The role of surgical cytoreduction in the treatment of malignant pleural mesothelioma: meeting summary of the International Mesothelioma Interest Group Congress; 11–14 September 2012, Boston. J Thorac Cardiovasc Surg 2013;145:909–10 [DOI] [PubMed] [Google Scholar]
- 19.Treasure T, Utley M, O'Byrne K. MARS a sense of perspective and an inconvenient truth. J Thorac Oncol 2013;8:e48–9 [DOI] [PubMed] [Google Scholar]
- 20.Bliss JM, Coombes G, Darlison L, et al. The MARS feasibility trial: correspondence. Lancet Oncol 2011;12:1094–5 [Google Scholar]
- 21.Lilford RJ, Thornton JG, Braunholtz D. Clinical trials and rare diseases: a way out of a conundrum. BMJ 1995;311:1621–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rice DC, Stevens CW, Correa AM, et al. Outcomes after extrapleural pneumonectomy and intensity-modulated radiation therapy for malignant pleural mesothelioma. Ann Thorac Surg 2007;84:1685–92 [DOI] [PubMed] [Google Scholar]
- 23.Flores RM, Pass HI, Seshan VE, et al. Extrapleural pneumonectomy versus pleurectomy/decortication in the surgical management of malignant pleural mesothelioma: results in 663 patients. J Thorac Cardiovasc Surg 2008;135:620–6 [DOI] [PubMed] [Google Scholar]
- 24.Tilleman TR, Richards WG, Zellos L, et al. Extrapleural pneumonectomy followed by intracavitary intraoperative hyperthermic cisplatin with pharmacologic cytoprotection for treatment of malignant pleural mesothelioma: a phase II prospective study. J Thorac Cardiovasc Surg 2009;138:405–11 [DOI] [PubMed] [Google Scholar]
- 25.Flores RM, Zakowski M, Venkatraman E, et al. Prognostic factors in the treatment of malignant pleural mesothelioma at a large tertiary referral center. J Thorac Oncol 2007;2:957–65 [DOI] [PubMed] [Google Scholar]
- 26.Lang-Lazdunski L, Bille A, Lal R, et al. Pleurectomy/decortication is superior to extrapleural pneumonectomy in the multimodality management of patients with malignant pleural mesothelioma. J Thorac Oncol 2012;7:737–43 [DOI] [PubMed] [Google Scholar]
- 27.Rena O, Casadio C. Extrapleural pneumonectomy for early stage malignant pleural mesothelioma: A harmful procedure. Lung Cancer 2012;77:151–5 [DOI] [PubMed] [Google Scholar]
- 28.Steele J. Randomised trial of extended pleurectomy and decortication (EPD) with pemetrexed and platinum chemotherapy versus pemetrexed and platinum alone in patients with malignant pleural mesothelioma (‘MARS-2’). Proc IMIG 2012; 12–14 September 2012, Boston 2012:P3.22 http://www.imig2012.org/documents/iMig2012_AbstractBook_vF_Sept10_REV.pdf [Google Scholar]
- 29.NCCN guidelines for patients: malignant pleural mesothelioma: national cancer collaborative network. http://www.nccn.org/patients/patient_guidelines/mpm/files/assets/basic-html/page22.html [Google Scholar]
- 30.Qaseem A, Forland F, Macbeth F, et al. Guidelines International Network: toward international standards for clinical practice guidelines. Ann Intern Med 2012;156:525–31 [DOI] [PubMed] [Google Scholar]
- 31.Treasure T, Utley M. Statistics for the rest of us: ten traps for the unwary in surgical series: a case study in mesothelioma reports. J Thorac Cardiovasc Surg 2007;133:1414–18 [DOI] [PubMed] [Google Scholar]
- 32.Utley M, Fiorentino F, Treasure T. Obtaining an upper estimate of the survival benefit associated with surgery for mesothelioma. Eur J Cardiothorac Surg 2010;38:241–4 [DOI] [PubMed] [Google Scholar]
- 33.Hasani A, Alvarez JM, Wyatt JM, et al. Outcome for patients with malignant pleural mesothelioma referred for trimodality therapy in Western Australia. J Thorac Oncol 2009;4:1010–16 [DOI] [PubMed] [Google Scholar]
- 34.Treasure T, Internullo E, Fiorentino F, et al. A survey of opinions and beliefs concerning surgery for malignant pleural mesothelioma amongst 802 members of the European Association for Cardio-Thoracic Surgery (EACTS), the European Society of Thoracic Surgeons (ESTS) and the Society of Thoracic Surgeons (STS). Interact Cardiovasc Thorac Surg 2011;12:341–6 [DOI] [PubMed] [Google Scholar]
- 35.Rena O, Casadio C. Lack of evidence in malignant pleural mesothelioma surgery. Interact Cardiovasc Thorac Surg 2011;12:347–8 [DOI] [PubMed] [Google Scholar]
- 36.Ploenes T, Osei-Agyemang T, Krohn A, et al. Changes in lung function after surgery for mesothelioma. Asian Cardiovasc Thorac Ann 2013;21:48–55 [DOI] [PubMed] [Google Scholar]
- 37.Russell RCG, Treasure T. Counting the cost of cancer surgery for advanced and metastatic disease. Br J Surg 2012;99:449–50 [DOI] [PubMed] [Google Scholar]
- 38.Treasure T, Morton D. GRIST growing recruitment in interventional and surgical trials. J R Soc Med 2012;105:140–1 [DOI] [PMC free article] [PubMed] [Google Scholar]