Abstract
Introduction
ITP is an autoimmune blood disorder in which platelet destruction is mediated by anti-platelet antibodies. The mechanisms of anti-platelet antibodies development are still a little known. The rate of some bacterial or viral agents in cause of ITP is well known. Recently, some study proposed that H pylori infection may be associated with ITP and H pylori eradication can improves platelet counts in infected ITP patients.
Materials and Method
A baseline platelet count <50×103 µL for 4 weeks prior to study entry were required. These patients were tested for H. pylori infection by urea breath. All positive H pylori patients received triple therapy for 7 or 14 days to eradicate H pylori infection. These patients followed for six months.
Results
Of 92 patients with ITP, H pylori infection was found in 59.7% (55/92). After excluding patients with confounding factors, 41 patients were remained. After H pylori eradication, CR wasn't obtained in any patients. Partial response were obtained only in 3 (7.3%) of the 41 patients and no response in 38 (92.6%) patients. There is a significant difference between the platelet counts of PR and NR groups (P < 0.001).
Conclusion
The results of this study and our previously study showed H pylori eradication therapy has beneficial effect for patients with mild thrombocytopenia but the chance of obtaining a response by H pylori treatment is lower in patients with severe thrombocytopenia.
Keywords: Idiopathic thrombocytopenic purpura, Helicobacter pylori, Platelet counts
INTRODUCTION
Idiopathic thrombocytopenic purpura (ITP) is an autoimmune blood disorder characterized by the production of antibodies against platelets antigens and therefore platelet destruction. The major cause of this disorder Is IgG antibodies bind to the platelet surface glycoprotein such as GPIIb-IIIa, GPIb-IX and etc.1 Still, all causes factors for developing ITP aren't known. However, the association between this disorder with hepatitis C, Cytomegalovirus, HIV, sepsis and other viruses are known to common childhood was confirmed and this issue showed association between ITP and infection agents.2–4 In the late 1990s, Initial case reports described increased platelet counts in patients with ITP following after Helicobacter pylori (H pylori) eradication. Since then, several studies have investigated that whether H pylori eradication can improves platelet counts in infected ITP patients.5
H pylori is a gram-negative microaerophilic bacterium that colonizes in over half the human population. Interestingly, the prevalence of H pylori in ITP patients from 22 to 90.6 percent is changing in different parts of the world.6–11 Since, the role of H pylori in developing ITP isn't well known. There are several hypotheses as to why H pylori, that predominately inhabits the gastric mucosa, may be associated with developing ITP that improve or resolve after H pylori eradication.12, 13 One hypothesis proposes that an H pylori surface antigen, such as the anti cytotoxin associated gene A protein (CagA), evokes a host systemic immune response that produces auto-antibodies cross reactive with host platelets. This hypothesis may explain the observed variability in treatment effect by country since CagA-positive strains of H pylori are more prevalent in some countries. Other proposed mechanisms are modulation of host immunity following colonization by H pylori to favor the emergence of autoreactive B-1 cells and the enhancement of phagocytic capacity of monocytes together with low levels of the inhibitory Fcγ receptor IIB following H pylori infection.15–18 Further, another hypothesis explain eradication therapy may result in the improvement of thrombocytopenia by mechanisms independent of H pylori including the immune modulating effects of the treatment itself or the removal of other commensal bacteria.19 However, in reject of this hypothesis there are some data showing that a beneficial effect of the H pylori eradication without infection was not observed.20–21
Our previously study22 showed revealed eradication therapy of H pylori infection can improve platelet counts in ITP patients with mild thrombocytopenia and it seems this eradication cannot have a major role in the treatment in a little group of severe ITP patients of our study. In this study we investigated the effects of H pylori eradication on platelet counts in a larger group of severe ITP patients in a teaching hospital in Kermanshah, west of Iran.
MATERIALS AND METHODS
Patients
The medical records of 92 (50 male and 42 female) adult with severe chronic ITP that refer to us between June 2008 and November 2012 were retrospectively examined for the presence of gastric H pylori infection. The diagnosis of ITP was confirmed by a hematologist according to standard criteria.21 A baseline platelet count <50×103 µL for 4 weeks prior to study entry were required. Cases of thrombocytopenia caused by drugs, pseudo thrombocytopenia, family history consistent with inherited thrombocytopenia, human immunodeficiency virus infection, hepatitis, and autoimmune disorders were excluded. Patients were excluded if they had been treated for H pylori within 2 years of recruitment or if they had been treated with an antibiotic or proton pump inhibitor within the previous 4 weeks.13 According to declaration of Helsinki; we took consent from all patients before H pylori eradication for remedy of their ITP disorders.
Diagnosis and Treatment
All 92 Patients were screened for H pylori infection using H pylori urea breath test (UBT) and serum H pylori antibody. H pylori infection was treated with standard eradication therapy: amoxicillin 1000 mg twice daily, clarithromcin 500 mg twice daily, and a proton pump inhibitor 40 mg twice daily for 2 weeks. Platelet counts were obtained at baseline and then every 2 weeks until month 6.
Response Criteria
Complete response (CR) was defined as a platelet count >150×103 µL at month 6. Partial response (PR) was defined by a platelet increase of >30×103 µL at month 6. Relapse was defined as any platelet count below either of these values after month 6. No response (NR) was defined as any platelet count below either of these values after month 6.
Statistical Analysis
Differences of platelet count are expressed as the mean (SD) as appropriate. A Mann-Whitney-u test was used for analysis of platelet differences in 3 groups (CR, PR and NR). A P-value of less than 0.05 was considered statistically significant. All statistical analysis was performed by using SPSS software version 21.0.
RESULTS
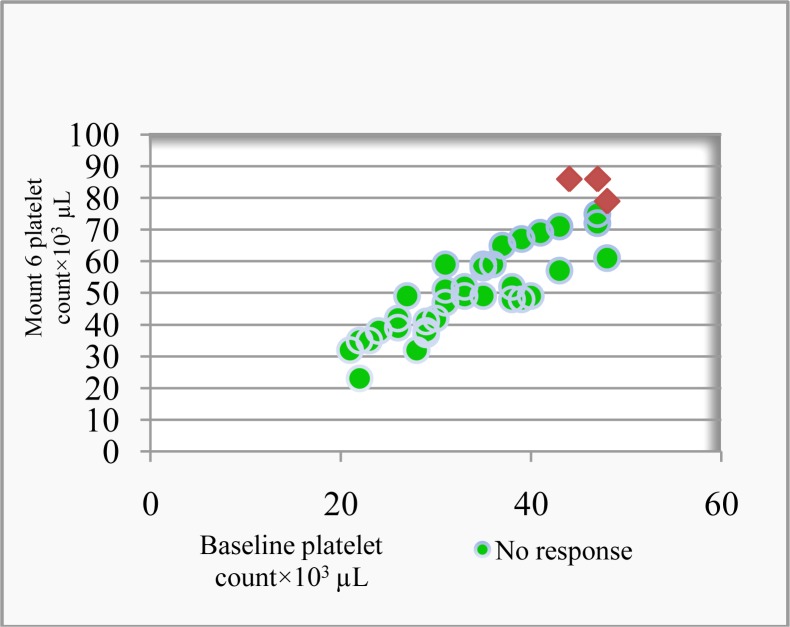
Of 92 patients with ITP, H pylori infection was found in 59.7% (55/92) of patients. Five patients with autoimmune disorders, two patients with HBV infection and one patient with HCV infection were excluded. Thus 47 patients were considered whom 41 (21 males, 20 females) achieved H pylori eradication (87.2%). Median disease duration before H pylori eradication was 2.2 month (1- 4.5 months). There is no significant different between platelet response and disease duration (P > 0.08). We fallowed up patients 6 mount. Outcomes after H pylori eradication of the patients with ITP are indicated in Table 1. After H pylori eradication, CR wasn't obtained in any patients. Partial response were obtained only in 3 (7.3%) of the 41 patients and no response in 38 (92.6%) patients (Figure 1). There is a significant difference between the platelet counts of PR and NR groups (P < 0.001).
Table 1.
Clinical and Platelet Response Characteristics by Patient
| Patient | Baseline platelet count×103 µL | Mount 6 platelet count×103 µL | Response status | ||
|---|---|---|---|---|---|
| No | Sex | Age | |||
| 1 | F | 27 | 26 | 39 | NR |
| 2 | M | 19 | 38 | 52 | NR |
| 3 | F | 54 | 47 | 72 | NR |
| 4 | M | 37 | 31 | 51 | NR |
| 5 | M | 63 | 35 | 59 | NR |
| 6 | M | 29 | 41 | 69 | NR |
| 7 | F | 61 | 29 | 37 | NR |
| 8 | F | 35 | 21 | 32 | NR |
| 9 | F | 39 | 23 | 35 | NR |
| 10 | F | 22 | 44 | 86 | PR |
| 11 | M | 46 | 43 | 71 | NR |
| 12 | M | 31 | 36 | 59 | NR |
| 13 | M | 44 | 37 | 65 | NR |
| 14 | F | 28 | 48 | 79 | PR |
| 15 | M | 51 | 33 | 49 | NR |
| 16 | F | 39 | 28 | 32 | NR |
| 17 | F | 48 | 24 | 38 | NR |
| 18 | M | 33 | 35 | 58 | NR |
| 19 | M | 67 | 22 | 35 | NR |
| 20 | F | 31 | 47 | 86 | PR |
| 21 | F | 25 | 26 | 42 | NR |
| 22 | F | 20 | 31 | 47 | NR |
| 23 | F | 38 | 38 | 52 | NR |
| 24 | M | 48 | 29 | 41 | NR |
| 25 | M | 58 | 27 | 49 | NR |
| 26 | F | 30 | 31 | 59 | NR |
| 27 | M | 48 | 47 | 75 | NR |
| 28 | F | 59 | 41 | 69 | NR |
| 29 | M | 49 | 36 | 59 | NR |
| 30 | M | 21 | 39 | 67 | NR |
| 31 | M | 54 | 43 | 57 | NR |
| 32 | M | 43 | 29 | 38 | NR |
| 33 | M | 37 | 22 | 23 | NR |
| 34 | M | 33 | 35 | 49 | NR |
| 35 | F | 33 | 38 | 48 | NR |
| 36 | F | 27 | 30 | 42 | NR |
| 37 | F | 65 | 33 | 52 | NR |
| 38 | M | 71 | 40 | 49 | NR |
| 39 | M | 19 | 48 | 61 | NR |
| 40 | F | 38 | 29 | 37 | NR |
| 41 | F | 67 | 39 | 48 | NR |
Figure 1.
Platelet count response status after 6 months vs baseline platelet ( ×103 µm)
DISCUSSION
ITP is an autoimmune blood disorder in which platelet destruction is mediated by anti-platelet antibodies. The mechanisms of anti-platelet antibodies development are still a little known. The rate of some bacterial or viral agents in cause of ITP is well known. It has been demonstrated that the mimicry of human antigens by infection agents represents the mechanism underlying this phenomenon.7–9 Many studies have shown an association between H pylori infection and ITP, and substantial evidence has indicated that achieving H pylori eradication can lead to a significant improvement in platelet counts in these H pylori -positive ITP patients. Gasbarrini et al., First reported that 61% of 18 ITP cases with H pylori were eradicated, showed significant increases in mean platelet count after 2 and 4 months with disappearance of anti-platelet antibody. 5 In recent years, many studies have demonstrated improvement of platelet counts in ITP patients after treatment of H pylori infection.13–18
Several studies have treated both H pylori positive and H pylori negative patients with H pylori eradication therapy with no responses in the H pylori negative group.6, 14, 24, 25 Further, Arnold et al., concluded that treatment of thrombocytopenia in adults with ITP using H pylori eradication therapy should be reserved for patients with active H pylori infection.21 A beneficial effect of the treatment for H pylori-negative patients was not observed. So, we excluded H pylori-negative patients from our study. Also, we excluded patients with confounding factors to avoid bias in our results.
In present study, the prevalence of H pylori infection in severe ITP patients was 59.7%. In our pervious study,22 the prevalence of H pylori infection in ITP patients was 69.3%. This difference indicate that the prevalence of H pylori infection in severe ITP patients is lower than mild ITP patients and it suggest this hypothesis H pylori infection in severe ITP patients is less important as the major cause of this disorder. Nevertheless, this prevalence is high and this rate almost similar to prevalence of H pylori infection in the general population in Iran.26 These results also were comparable to those of previous studies which were done in Asian countries such as Japan and South Korea but this rate is in contrast studies were conducted in Western countries.27 In general, the prevalence of H pylori infection varies according to geographic location and in Asian countries such as Iran is too high.
In this study all patients with H pylori infection was treated with triple therapy regime and eradication rate was 87.2%. This finding is in agreement to other studies which they have showed successful eradication greater than 70% using triple therapy.28, 29
The platelet recovery rate after H pylori eradication therapy appears to be as heterogeneous between studies as the response rates. In most studies, a shorter ITP duration is correlated with better chance of response.12, 29 In present study, median disease duration before H pylori eradication was 2.2 month and there is no significant different between platelet response and disease duration.
There are conflicting reports about the predictive value of baseline platelet count.24, 28 In our previous study,22 we had 65.6% of patients that have response to eradication and all responders had platelet count ≥50×103 µL. Also, we observed poor response to treatment in ITP patients with severe thrombocytopenia. So, we concluded H pylori eradication can improve platelet counts in ITP patients with mild thrombocytopenia but not in sever ITP patients. But, because of a few number of severe ITP patients (11/26 patients) we couldn't conclude exactly.
In our present study, we saw poor response to treatment in patients with severe thrombocytopenia, again. In this study all of patients had baseline platelet count <50×103 µL. Of 41 patients that achieved H pylori eradication just 3 (7.3%) patients had partial response and other patients had no response. Also, there were no patients with complete response. These results suggest that probably, patients with severe thrombocytopenia (<50×103 µL) appear to have fewer chances of response, although this issue has not been systematically addressed in most published reports. In confirm, an Italian/UK study Indicated that 33% (17 of 52) patients had platelet responses, but only 1 response was observed among patients with severe thrombocytopenia.30
In conclusion, the results of this study and our previously study showed H pylori eradication therapy has beneficial effect for patients with mild thrombocytopenia but the chance of obtaining a response by H pylori treatment is lower in patients with severe thrombocytopenia. Further studies are required to clarify causative factors involved in platelet recovery, monitor the duration of response, and understand the mechanism underlying the response to eradication therapy.
ACKNOWLEDGEMENT
This work was performed in partial fulfillment of the requirements for G.P. (General Physician) of Samira Gholami, in Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran.
REFERENCES
- 1.Fan H, Zhu HL, Li SX, Lu XC, Zhai B, Guo B, Yao SQ, Liu Y. Efficacy of amifostine in treating patients with idiopathic thrombocytopenia purpura. Cell Biochem Biophys. 2011;59(1):7–12. doi: 10.1007/s12013-010-9100-5. [DOI] [PubMed] [Google Scholar]
- 2.McCrae K. Helicobacter pylori and ITP: many questions, few answers. Blood Journal. 2004;103(3):752–3. [Google Scholar]
- 3.Arif SH, Ahmad I, Ali SM, Khan HM. Thrombocytopenia and Bacterial Sepsis in Neonates. Indian J Hematol Blood Transfus. doi: 10.1007/s12288-011-0118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nascimento FG, Tanaka PY. Thrombocytopenia in HIV-Infected Patients. Indian J Hematol Blood Transfus. doi: 10.1007/s12288-011-0124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gasbarrini A, Franceschi F, Tartaglione R, Landolfi R, Pola P, Gasbarrini G. Regression of autoimmune thrombocytopenia after eradication of Helicobacter pylori. Lancet. 1998;352:878. doi: 10.1016/S0140-6736(05)60004-9. [DOI] [PubMed] [Google Scholar]
- 6.Jackson SC, Beck P, Buret AG, O'Connor PM, Meddings J, Pineo G, Poon MC. Long term platelet responses to Helicobacter pylori eradication in Canadian patients with immune thrombocytopenic purpura. Int J Hematol. 2008;88(2):212–8. doi: 10.1007/s12185-008-0138-8. [DOI] [PubMed] [Google Scholar]
- 7.Russo A, Eboli M, Pizzetti P, et al. Determinants of Helicobacter pylori seroprevalence among Italian blood donors. Eur J Gastroenterol Hepatol. 1999;11:867–73. doi: 10.1097/00042737-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Graham DY, Kimura K, Shimoyama T, Takemoto T. Helicobacter pylori infection in Japan: current status and future options. Eur J Gastroenterol Hepatol. 1994;(6 Suppl 1):S1–4. [PubMed] [Google Scholar]
- 9.Graham DY, Malaty HM, Evans DG, Evans DJ, Jr, Klein PD, Adam E. Epidemiology of Helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology. 1991;100:1495–501. doi: 10.1016/0016-5085(91)90644-z. [DOI] [PubMed] [Google Scholar]
- 10.Michel M, Khellaf M, Desforges L, et al. Autoimmune thrombocytopenic Purpura and Helicobacter pylori infection. Arch Intern Med. 2002;162:1033–6. doi: 10.1001/archinte.162.9.1033. [DOI] [PubMed] [Google Scholar]
- 11.Yim JY, Kim N, Choi SH, et al. Seroprevalence of Helicobacter pylori in South Korea. Helicobacter. 2007;12:333–40. doi: 10.1111/j.1523-5378.2007.00504.x. [DOI] [PubMed] [Google Scholar]
- 12.Stasi R, Provan D. Helicobacter pylori and Chronic ITP. Hematology Am Soc Hematol Educ Program. 2008:206–11. doi: 10.1182/asheducation-2008.1.206. [DOI] [PubMed] [Google Scholar]
- 13.Tag HS, Lee HS, Jung SH, Kim BK, Kim SB, Lee A, Lee JS, Shin SH, Kim YS. Effects of Helicobacter pylori eradication in patients with immune thrombocytopenic purpura. Korean J Hematol. 2010;45(2):127–32. doi: 10.5045/kjh.2010.45.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takahashi T, Yujiri T, Shinohara K, Inoue Y, Sato Y, Fujii Y, et al. Molecular mimicry by Helicobacter pylori CagA protein may be involved in the pathogenesis of H pylori-associated chronic idiopathic thrombocytopenic purpura. Br J Haematol. 2004;124:91–6. doi: 10.1046/j.1365-2141.2003.04735.x. [DOI] [PubMed] [Google Scholar]
- 15.Franceschi F, Christodoulides N, Kroll MH, Genta RM. Helicobacter pylori and idiopathic thrombocytopenic purpura. Ann Intern Med. 2004;140:766–7. doi: 10.7326/0003-4819-140-9-200405040-00028. [DOI] [PubMed] [Google Scholar]
- 16.Perez-Perez GI, Bhat N, Gaensbauer J, Fraser A, Taylor DN, Kuipers EJ, et al. Country-specific constancy by age in cagA+ proportion of Helicobacter pylori infections. Int J Cancer. 1997;72:453–6. doi: 10.1002/(sici)1097-0215(19970729)72:3<453::aid-ijc13>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 17.Yamanishi S, Iizumi T, Watanabe E, Shimizu M, Kamiya S, Nagata K, et al. Implications for induction of autoimmunity via activation of B-1 cells by Helicobacter pylori urease. Infect Immun. 2006;74:248–56. doi: 10.1128/IAI.74.1.248-256.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asahi A, Nishimoto T, Okazaki Y, Suzuki H, Masaoka T, Kawakami Y, et al. Helicobacter pylori eradication shifts monocyte Fcgamma receptor balance toward inhibitory FcgammaRIIB in immune thrombocytopenic purpura patients. J Clin Invest. 2008;118:2939–49. doi: 10.1172/JCI34496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ianaro A, Ialenti A, Maffia P, Sautebin L, Rombola L, Carnuccio R, et al. Anti-inflammatory activity of macrolide antibiotics. J Pharmacol Exp Ther. 2000;292:156–63. [PubMed] [Google Scholar]
- 20.Arnold DM, Bernotas A, Nazi I, Stasi R, Kuwana M, Liu Y, Kelton JG, Crowther MA. Platelet count response to H pylori treatment in patients with immune thrombocytopenic purpura with and without H pylori infection: a systematic review. Haematologica. 2009 Jun;94(6):850–6. doi: 10.3324/haematol.2008.005348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arnold DM, Stasi R. Does Helicobacter pylori eradication therapy result in a platelet count improvement in adults with immune thrombocytopenic purpura regardless of H pylori infection? ASH evidence-based review 2008. Hematology Am Soc Hematol Educ Program. 2008:31–2. doi: 10.1182/asheducation-2008.1.31. [DOI] [PubMed] [Google Scholar]
- 22.Payandeh M, Sohrabi N, Zare ME, Kansestani AN, Hashemian AH. Platelet Count Response to Helicobacter pylori Eradication in Iranian Patients with Idiopathic Thrombocytopenic Purpura. Mediterr J Hematol Infect Dis. 2012;4(1):2012056. doi: 10.4084/MJHID.2012.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morimoto N, Takeuchi H, Takahashi T, Ueta T, Tanizawa Y, Kumon Y, et al. Helicobacter pylori associated chronic idiopathic thrombocytopenic purpura and low molecular weight H. pylori proteins. Scand J Infect Dis. 2007;39:409–16. doi: 10.1080/00365540601105723. [DOI] [PubMed] [Google Scholar]
- 24.Suvajdzić N, Stanković B, Artiko V, et al. Helicobacter pylori eradication can induce platelet recovery in chronic idiopathic thrombocytopenic purpura. Platelets. 2006;17:227–30. doi: 10.1080/09537100500462487. [DOI] [PubMed] [Google Scholar]
- 25.Ohguchi H, Kameoka J, Harigae H, et al. Can the Helicobacter pylori eradication regimen induce platelet recovery in H pylori negative patients with idiopathic thrombocytopenic purpura. Am J Hematol. 2005;78:164–5. doi: 10.1002/ajh.20266. [DOI] [PubMed] [Google Scholar]
- 26.Abadi AT, Taghvaei T, Mobarez AM, Carpenter BM, Merrell DS. Frequency of antibiotic resistance in Helicobacter pylori strains isolated from the northern population of Iran. J Microbiol. 2011;49(6):987–93. doi: 10.1007/s12275-011-1170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham DY, Malaty HM, Evans DG, Evans DJ, Jr, Klein PD, Adam E. Epidemiology of Helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology. 1991;100:1495–501. doi: 10.1016/0016-5085(91)90644-z. [DOI] [PubMed] [Google Scholar]
- 28.Inaba T, Mizuno M, Take S, Suwaki K, Honda T, Kawai K, Fujita M, Tamura T, Yokota K, Oguma K, Okada H, Shiratori Y. Eradication of Helicobacter pylori increases platelet count in patients with idiopathic thrombocytopenic purpura in Japan. Eur J Clin Invest. 2005;35:214–219. doi: 10.1111/j.1365-2362.2005.01471.x. [DOI] [PubMed] [Google Scholar]
- 29.Fujimura K, Kuwana M, Kurata Y, Imamura M, Harada H, Sakamaki H, Teramura M, Koda K, Nomura S, Sugihara S, Shimomura T, Fujimoto TT, Oyashiki K, Ikeda Y. Is eradication therapy useful as the first line of treatment in Helicobacter pylori positive idiopathic thrombocytopenic purpura? Analysis of 207 eradicated chronic ITP cases in Japan. Int J Hematol. 2005;81:162–168. doi: 10.1532/ijh97.04146. [DOI] [PubMed] [Google Scholar]
- 30.Stasi R, Rossi Z, Stipa E, Amadori S, Newland AC, Provan D. Helicobacter pylori eradication in the management of patients with idiopathic thrombocytopenic purpura. Am J Med. 2005;118:414–9. doi: 10.1016/j.amjmed.2004.09.014. [DOI] [PubMed] [Google Scholar]