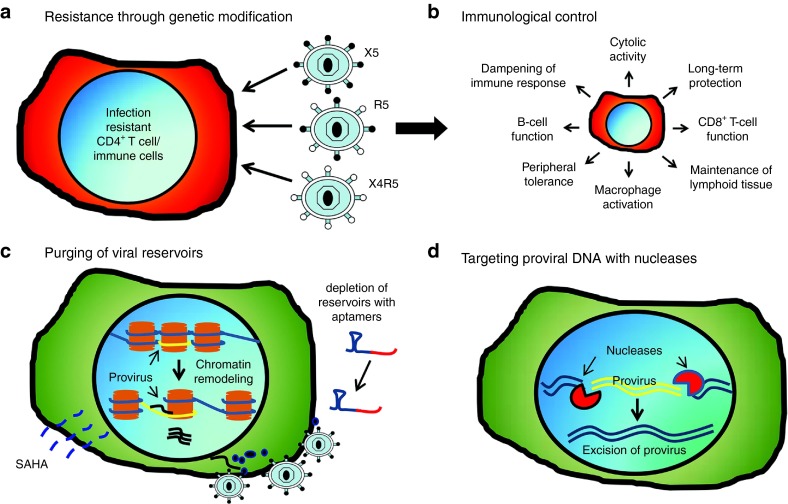
Figure 1.
Achieving immunological control in human immunodeficiency virus (HIV)-1–infected patients. (a) Genetic modification of target cells (hematopoietic stem cells or CD4+ T cells) has been shown to significantly reduce viral infectivity in vitro and in vivo. Disruption of CCR5 prevents infection from R5-tropic strains while expression of the mC46-fusion inhibitor prevents infection of HIV regardless of viral tropism. (b) The development of infection-resistant immune cell populations following infusion of genetically modified hematopoietic stem cells (HSCs) or CD4+ T cells promotes an enhanced immune response against HIV (e.g., antibody response) and HIV-infected cells (e.g., cytotoxic T-cell response). Protected cells maintain functional activity improving both innate and adaptive immune responses against the virus, in addition to reducing the number of potential target cells, which serve to further reduce the latent reservoir. (c) Elimination of viral reservoirs will require the identification of latently infected cells in order to promote targeted deletion of infected cells through immunological responses or through targeted therapies. Reagents including Prostratin or suberoylanilide hydroxamic acid have previously been shown to promote viral reactivation in latently infected cells. Following the induced expression and transport of viral antigens to the plasma membrane of infected cells, targeted therapies such as aptamer-mediated delivery of toxic siRNAs can be utilized to diminish and/or eliminate viral reservoirs. (d) Highly conserved sequences within the viral genome can be targeted with sequence specific nucleases to disrupt or delete conserved regions fundamentally required for viral replication (e.g., transactivation response element).