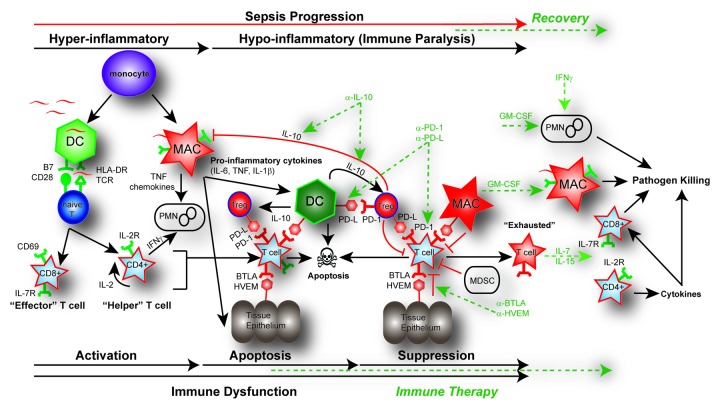
Figure 2. Pathways of immune dysfunction and targets for immune enhancing therapy in sepsis. In the initial pro-inflammatory response of sepsis, both the adaptive and innate immune systems are rapidly activated. This activation of monocytes, dendritic cells (DC), and macrophages (MAC), as well as CD4 helper and CD8 cytotoxic T cells results in the release of pro-inflammatory cytokines (TNF, IL-6, IL-1β) and chemokines. This pro-inflammatory response normally results in cellular activation and clearance of the primary pathogen (~~, pathogen). In the instance of a healthy individual, the immune system maintains homeostasis by employing counter inflammatory mechanisms such as regulatory T cells (Tregs), apoptosis, production of cytokines, expression of inhibitory receptors and myeloid-derived suppressor cells (MDSC) concurrently during inflammation. However, in some septic patients these normal homeostatic counter inflammatory mechanisms remain elevated such as expression of inhibitory receptors including: programmed death receptor -1 (PD-1), programmed death ligand (PD-L), B and T lymphocyte attenuator (BTLA), and herpesvirus entry mediator (HVEM) as well as the production of the immune modulating cytokine IL-10. Immune dysfunction occurs as activated innate and adaptive immune cells undergo rapid apoptosis while in the presence of increased suppressor cell populations like Tregs or MDSC. The primary infection fails to be cleared and may progress into immune suppression. Prolonged immune suppression and persistent antigen may result in T-cell exhaustion indicated by a T cell’s increased expression of PD-1 and decreased expression of the IL-7R as well as a functional impairment that includes failure to proliferate, secrete cytokines, and kill target cells. Potential targets for immune-therapy are indicted in the dotted GREEN line. Potential therapeutic targets include using blocking antibodies such as anti-IL-10 to decrease Treg function; anti-PD-1 and anti-PD-L to reverse the induction of T-cell exhaustion; and anti-HVEM or anti-BTLA to block tissue suppression of immune cells. IL-7 or IL-15 may be effective in blocking apoptosis and reversing cell exhaustion; GM-CSF to stimulate APC function by increasing recruitment and HLA-DR expression; and IFN-γ to increase PMN recruitment and function.

An official website of the United States government
Here's how you know
Official websites use .gov
A
.gov website belongs to an official
government organization in the United States.
Secure .gov websites use HTTPS
A lock (
) or https:// means you've safely
connected to the .gov website. Share sensitive
information only on official, secure websites.