Abstract
Background
The role of ductular reaction (DR) in hepatocellular carcinoma (HCC) remains to be elucidated.
Methods
In this study, we tried to uncover possible effect by correlating peritumoral DR in a necroinflammatory microenvironment with postoperative prognosis in HCC. The expression of peritumoral DR/CK19 by immunohistochemistry, necroinflammation and fibrosis were assessed from 106 patients receiving curative resection for HCC. Prognostic values for these and other clinicopathologic factors were evaluated.
Results
Peritumoral DR significantly correlated with necroinflammation (r = 0.563, p = 3.4E-10), fibrosis (r = 0.435, p = 3.1E-06), AFP level (p = 0.010), HBsAg (p = 4.9E-4), BCLC stage (p = 0.003), TNM stage (p = 0.002), multiple nodules (p = 0.004), absence of tumor capsule (p = 0.027), severe microscopic vascular invasion (p = 0.031) and early recurrence (p = 0.010). Increased DR was significantly associated with decreased RFS/OS (p = 4.8E-04 and p = 2.6E-05, respectively) in univariate analysis and were identified as an independent prognostic factor (HR = 2.380, 95% CI = 1.250-4.534, p = 0.008 for RFS; HR = 4.294, 95% CI = 2.255-8.177, p = 9.3E-6 for OS) in multivariate analysis.
Conclusions
These results suggested that peritumoral DR in a necroinflammatory microenvironment was a poor prognostic factor for HCC after resection.
Keywords: Ductular reaction (DR), Hepatic progenitor cells (HPCs), Necroinflammation, Fibrosis, Hepatocellular carcinoma (HCC), Prognosis
Background
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide [1]. Despite the great advancement in diagnosis and treatment modalities, especially surgical and targeted therapies, it’s outcome remains challenging due to frequent recurrence [2]. It is short of effective specific treatment after postoperative metastasis and recurrence in HCC [3]. Therefore, it is of great importance to seek optimal biomarkers that help predict early recurrence or metastasis.
HCC with progenitor cell features, possibly reflecting a progenitor cell origin, has a very bad prognosis [4]. Hepatic progenitor cells (HPCs) exhibit large nuclear-cytoplasmic ratio and oval-shaped nucleus, known as oval cells in rodents [5]. It is believed that HPCs are the descendants of stem cells. HPCs are scarce in the healthy liver, but upon stimulation, cells resident in the Canals of Hering proliferate across the hepatic lobule infiltrating the liver parenchyma [6]. HPCs can be observed by immunohistochemistry and electron microscope. The neoplastic cells are offspring of HPCs and each can differentiate a little differently, according to the local microenvironment in each part of the tumor if it explains the enormous phenotypic heterogeneity of a neoplasm [4]. In immunohistochemistry the phenotypes of HPCs express as OV6, CK7, CK19, CD133 and EPCAM [7-9]. HPCs are verified to be able to differentiate into both hepatocytes and cholangiocytes when the latter fails to respond after severe injury [10].
HPCs form ductular reaction (DR), emanating from the portal zone and expanding into the parenchyma when they are activated to proliferate/differentiate, hepatocytic differentiation of these cells leads to the formation of intermediate hepatocytes [5]. Three types of DR are classically recognized, type 1, proliferation of pre-existing ducts and ductules; type 2, ductular metaplasia of hepatocytes and type 3, activation/proliferation of HPCs [11]. DR can be marked by immunostained with CK7 and CK19 [12,13]. DR plays an important role in hepatocellular or cholangiocellular proliferation after virus related inflammation and damage. DR may represent a protective mechanism that allows intrahepatic cycling of bile acids to occur in chronic ductopenic biliary diseases [13]. Its immunostaining may help to identify small foci of invasion and to distinguish noninvasive, high-grade dysplastic nodules from both minimally invasive and overtly invasive HCC [12].
Activated and proliferative mechanism of HPCs is not clear, and inflammatory cytokine is considered as a key role in animal experiment [14]. Severity and location of inflammatory infiltration associated with activity and location of HPCs in chronic virus hepatitis [15]. Inflammation has emerged as the seventh hallmark of cancer [16]. Such prolonged self-replication in an inflammatory microenvironment could result in the accumulation of genetic lesions that cause cancer formation [17]. There is substantial evidence that the proinflammatory response at the tumor stroma could be rerouted into a tumor-promoting direction by stimulating angiogenesis and tissue remodeling [18].
However, the role of peritumoral DR in a necroinflammatory microenvironment remains to be elucidated in HCC. At the present study, we investigated DR and necroinflammatory microenvironment of patients with HCC. We also tried to uncover possible effect by correlating DR in a necroinflammatory microenvironment with postoperative prognosis in HCC.
Methods
Patients and specimens
106 patients received curative resection of HCC in Eastern Hepatobiliary Hospital, the Second Military Medical University between 2001 and 2003. The total number of the patients with resected tumors during the same time period was 2180. Patients did not have signs of distant metastasis nor had they received anticancer therapy before surgery. The pathology of each patient was confirmed. Liver function was assigned by Child-Pugh scoring system. The role of the child pugh score was that 2 patients were B and 104 patients were A in this study. The tumor stage was determined according to 2002 AJCC/UICC tumor-node-metastasis (TNM) classification system and the Barcelona-Clinic Liver Cancer (BCLC) staging classification. Follow-up was as described in our previous report [1]. Data was censored at the last follow-up for patients without recurrence or death. Recurrence-free survival time (RFS) and overall survival time (OS) was defined as the interval between the time of surgery to that of recurrence or death, respectively. All human sample collection procedures were approved by China Ethical Review Committee and informed consent was obtained from all participants.
H&E and immunohistochemistry
The paraffin-embedded tissues stained with H&E were scored in a blinded manner according to Ishak scoring system by a single pathologist. The degree of necroinflammatory activity and the stage of fibrosis were scored 0–18 or 0–6 respectively in the non-tumor specimen according to Ishak et al.[19]. Median values were used as a cut-off in subsequent analyses. Immunohistochemistry was carried out according to appropriate protocols [20]. The primary antibody used was mouse monoclonal anti-CK19 (1:100, clone RCK108, Dako), Blank controls were treated identically except that the primary antibodies were omitted.
Evaluation of DR and morphometric determinations
CK19-immunoreactive DR was analyzed at the epithelial-stromal boundaries at the outer edge of tumor. Peritumoral DR was semiquantified as follows: 0 = none, 1 = <10%, 2 = 10% to 25%, 3 = 26% to 50%, and 4 = >50% [12]. Median value was used as a cut-off in subsequent analyses. HPCs and intermediate hepatobiliary cells were considered as CK19-positive cells, previous finding showing that [5].
Tissue samples
The study was approved by the Committee on Ethics, the Eastern Hepatobiliary Surgery Hospital of the Second Military Medical University, informed consent which has been conducted according to the principles expressed in the Declaration of Helsinki was obtained from each patient. All participants provided their written informed consent to participate in this study. HCC tissues were obtained from patients who underwent surgical operations for the tumors at Eastern Hepatobiliary Surgery Hospital.
Statistical analyses
Correlations between immunostaining parameters and clinicopathologic features were analyzed by χ2 tests, the Fisher’s exact test, and Spearman’s rho coefficient test as appropriate. Univariate and multivariate analysis was carried out with the Kaplan-Meier method and the Cox proportional hazards regression model and was compared with the log-rank test. For each analysis, only p <0.05 (two-sided) was considered statistically significant. All statistical analyses were made by use of SPSS 12.0 (SPSS Inc., Chicago, IL, USA).
Results
H&E and immunohistochemical characteristics
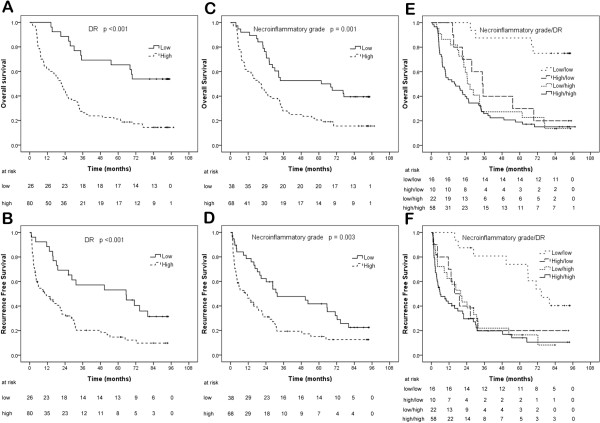
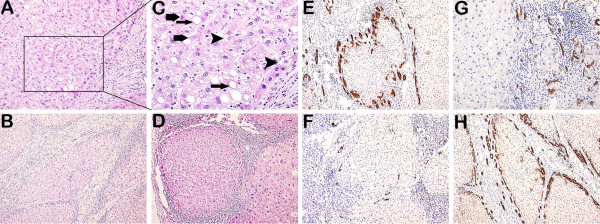
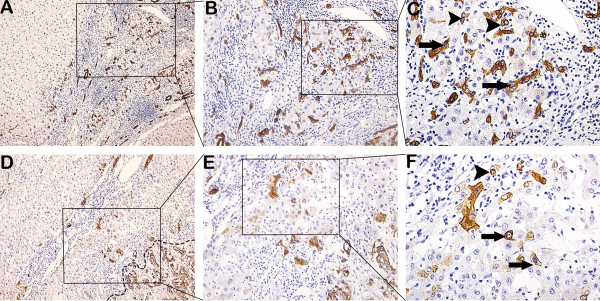
Representative images of necroinflammation and fibrosis/cirrhosis are shown (Figure 1). DR is shown in Figures 1, 2 and 3. As shown in Table 1, DR significantly correlated with necroinflammatory grade (r = 0.563, p = 3.4E-10) and fibrotic stage (r = 0.435, p = 3.1E-06). HPCs, intermediate hepatocytes and correlations with DR are shown in Figures 2 and 3.
Figure 1.
Immunostaining of DR, histopathology of necroinflammation and fibrosis/cirrhosis. (A, C) Ballooning degeneration (arrowheads), steatosis (thin arrows) and focal necrosis (thick arrows) were shown in the peritumoral parenchyma. (B) Cirrhosis and interface hepatitis were shown. (D) Fibrosis/cirrhosis and portal inflammation were shown. (E) Increased DR was around a nodule in the peritumoral tissue. (F) Decreased DR was around a nodule in the peritumoral tissue. (G) DR and necroinflammation were shown. Ballooning degeneration, steatosis and focal necrosis were nearby DR. Inflammatory cells were around DR in the portal tracts. (H) DR and cirrhosis were shown. DR was at the periphery of a cirrhotic nodule. (A and G 200×; C 400×; B, D, E, F and H 100×).
Figure 2.
Immunostaining of DR, histopathology of HPCs and intermediate hepatocytes in fibrotic tissue or peritumoral and tumoral tissues. (A, B, C) DR emanated from the portal zone and expanded into the parenchyma of proliferative nodules, HPCs (arrowheads) and intermediate hepatocytes (arrows) can be seen in the nodules. (D, E, F) DR and CK-19 positive tumor (in dashed line) that had no capsule were shown. HPC (arrowhead) was close to DR, intermediate hepatocytes (arrows) were between DR and neoplastic nodule. (A and D 100×; B and E 200×; C and F 400×).
Figure 3.
Correlations of DR with HPCs and intermediate hepatocytes in the peritumoral and tumoral tissues. (A) DR was at the periphery of the portal tracts. CK-19 positive tumor (in dashed line) had a partial capsule. A lot of intermediate hepatocytes were diffused in the peritumoral parenchyma. (B) At the tumoral borderline, 2 or 5 HPCs (arrowheads) gathered tightly, one intermediate hepatocyte (arrow) was among them. (C) In the peritumoral tissue, several intermediate hepatocytes (arrows) were nearby DR that was at the periphery of the portal tracts, and HPC (arrowhead) was in DR. (D) At the tumoral borderline, HPCs (arrowheads) gathered together, one intermediate hepatocyte (arrow) was closed to them, while intermediate hepatocytes (arrows) were diffused in the tumoral parenchyma. (A 100×; B, C and D 400×).
Table 1.
Necroinflammatory grade, fibrotic stage and correlations with DR
|
Variable |
Median |
25 and 75 percentiles |
Range |
Correlations with DR |
|
|---|---|---|---|---|---|
| r | p | ||||
| DR |
2 |
2-3 |
1-4 |
N.A. |
|
| Necroinflammatory grade |
9 |
7-12 |
4-15 |
0.563 |
3.4E-10 |
| Fibrotic stage | 4 | 3-5 | 1-6 | 0.435 | 3.1E-06 |
Correlations of DR with necroinflammatory grade and fibrotic stage were tested using Spearman’s rho coefficients tests.
Correlations between DR and clinicopathologic features
As shown in Table 2, increased DR correlated with advanced BCLC stage (p = 0.003), TNM stage (p = 0.002), with elevated serum ALT (p = 0.017), ALP (p = 0.007), AFP (p = 0.010) and HBsAg (+) (p = 4.9E-4). Increased DR was also tended to correlate with multiple nodules (p = 0.004), absence of tumor capsule (p = 0.027), severe microscopic vascular invasion (p = 0.031) and early recurrence (p = 0.010).
Table 2.
Correlations of DR with clinicopathologic features
| |
DR (<2 vs ≥2) |
||||
|---|---|---|---|---|---|
| Variable | Low (%) | High (%) | p | ||
| Age (year) (median; 25 and 75 percentiles) |
50; 40-59 |
≤50 |
13 (50.0) |
43 (53.8) |
0.379 |
| >50 |
13 (50.0) |
37 (46.2) |
|||
| Gender |
|
Male |
22 (84.6) |
66 (82.5) |
0.534 |
| Female |
4 (15.4) |
14 (17.5) |
|||
| ALT (U/L) (median; 25 and 75 percentiles) |
44.6; 29.9-72 |
≤40 |
16 (61.5) |
28 (35.0) |
0.017 |
| >40 |
10 (38.5) |
52 (65.0) |
|||
| γ-GT (U/L) (median; 25 and 75 percentiles) |
74.6; 46.4-106.8 |
≤55 |
13 (50.0) |
24 (30.0) |
0.063 |
| >55 |
13 (50.0) |
56 (70.0) |
|||
| ALP (U/L) (median; 25 and 75 percentiles) |
145; 116.5-190 |
≤121 |
13 (50.0) |
18 (22.5) |
0.007 |
| >121 |
13 (50.0) |
62 (77.5) |
|||
| AFP (ng/ml) (median; 25 and 75 percentiles) |
325; 40.9-1000 |
≤20 |
11 (42.3) |
14 (17.5) |
0.010 |
| >20 |
15 (57.7) |
66 (82.5) |
|||
| HBsAg state |
|
Negative |
10 (38.5) |
6 (7.5) |
4.9E-04 |
| Positive |
16 (61.5) |
74 (92.5) |
|||
| Tumor size (cm) (median; 25 and 75 percentiles) |
7; 4.6-11.8 |
≤5 |
7 (26.9) |
28 (35.0) |
0.447 |
| >5 |
19 (73.1) |
52 (65.0) |
|||
| Tumor number |
|
Single |
25 (96.2) |
54 (67.5) |
0.004 |
| Multiple |
1 (3.8) |
26 (32.5) |
|||
| Tumor capsule |
|
Yes |
10 (38.5) |
14 (17.5) |
0.027 |
| None |
16 (61.5) |
66 (82.5) |
|||
| Vascular invasion |
|
No |
18 (69.2) |
52 (65.0) |
0.692 |
| Yes |
8 (30.8) |
28 (35.0) |
|||
| Microscopic vascular invasion (mean ± SD)* |
4.3 ± 3.5 |
≤5 |
7 (87.5) |
10 (35.7) |
0.031 |
| >5 |
1 (12.5) |
18 (64.3) |
|||
| BCLC stage (A/B/C) |
39/12/55 |
A |
16 (61.5) |
23 (28.8) |
0.003 |
| B/C |
10 (38.5) |
57 (71.2) |
|||
| TNM stage (I/II/III) |
35/23/48 |
I |
15 (57.7) |
20 (25.0) |
0.002 |
| II/III |
11 (42.3) |
60 (75.0) |
|||
| Recurrence** |
|
Early |
8 (47.1) |
52 (65.0) |
0.010 |
| Late | 9 (52.9) | 12 (35.0) | |||
Chi-square tests for all the analyses. *Vascular invasion positive cases (36) were enrolled, the degree of microscopic peritumoral vascular invasion was observed. **A total of 81/106 (76.4%) patients suffered from tumor recurrence, of whom 60/81 (74.1%) patients recurred within two years and 21/81 (26.0%) recurred more than two years after surgery.
Prognostic factors
The follow-up was completed on December 25, 2009, with median follow-up time of 93 months (75 to 107 months). The 1-, 3-, 5-, 7-year RFS and OS rates were 54.7%, 24.5%, 19.8%, 8.5% and 71.7%, 36.8%, 32.1%, 20.8% respectively.
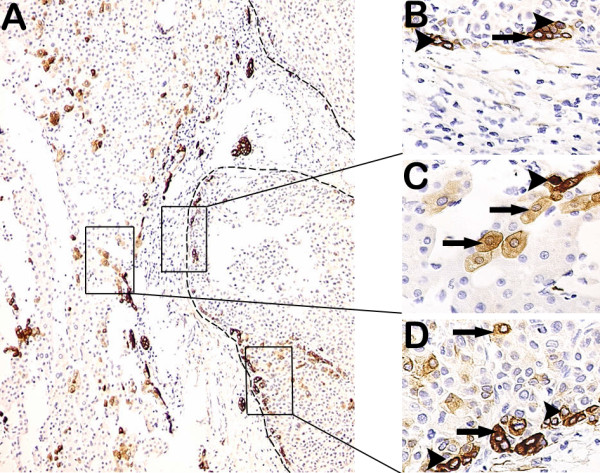
In the univariate analysis, decreased DR (p = 2.6E-05 for OS and p = 4.8E-04 for RFS, Figure 4A and B), decreased necroflammation (p = 0.001 for OS and p = 0.003 for RFS, Figure 4C and D) and decreased DR with lower necroflammation (p = 6.1E-05 for OS and p = 0.001 for RFS, Figure 4E and F) were associated with prolonged RFS and OS. Other clinicopathologic factors significant for RFS/OS are shown in Table 3.
Figure 4.
Kaplan–Meier analysis of DR and necroinflammatory grade from original cohort. Decreased DR (A and B), decreased necroinflammatory grade (C and D) and decreased DR with decreased necroinflammatory grade (E and F) were significantly associated with prolonged RFS (low/low vs high/low, low/high and high/high, p = 0.013, = 0.001 and <0.001; high/low vs low/high, p = 0.858; high/low vs high/high, p = 0.347; low/high vs high/high, p = 0.356) and OS (low/low vs high/low, low/high and high/high, p = 0.002, <0.001 and <0.001; high/low vs low/high, p = 0.472; high/low vs high/high, p = 0.191; low/high vs high/high, p = 0.373). The median was used as cut-off of DR and necroinflammatory grade, respectively.
Table 3.
Univariate and multivariate analyses of prognostic factors
| Variable |
Overall survival |
Recurrence-free survival |
||||
|---|---|---|---|---|---|---|
|
Univariate |
Multivariate |
Univariate |
Multivariate |
|||
| p | HR (95% CI) | p | p | HR (95% CI) | p | |
| Age, year (≤50 vs >50) |
0.719 |
|
N.A. |
0.881 |
|
N.A. |
| Gender (female vs male) |
0.013 |
|
N.A. |
0.003 |
|
N.A |
| ALT, U/L (≤40 vs >40) |
0.264 |
|
N.A. |
0.800 |
|
N.A. |
| γ-GT, U/L (≤55 vs >55) |
0.030 |
|
N.A. |
0.581 |
|
N.A. |
| ALP, U/L (≤121 vs >121) |
0.007 |
|
N.A |
0.077 |
|
N.A |
| Serum albumin, g/L (<35 vs ≥35) |
0.632 |
|
N.A |
0.712 |
|
N.A |
| AFP, ng/ml (≤20 vs >20) |
0.095 |
|
N.A. |
0.169 |
|
N.A. |
| HBsAg (negative vs positive) |
0.207 |
|
N.A. |
0.449 |
|
N.A. |
| Tumor size, cm (≤5 vs >5) |
6.0E-05 |
2.950 (1.694-5.137) |
1.3E-04 |
0.003 |
1.804 (1.057-3.080) |
0.031 |
| Tumor number (single vs multiple) |
0.006 |
|
N.A. |
3.3E-05 |
|
N.A. |
| Tumor capsule (yes vs none) |
0.016 |
|
N.A. |
0.015 |
|
N.A. |
| Microscopical intrahepatic metastasis (no vs yes) |
0.165 |
|
N.A. |
0.021 |
|
N.A. |
| Microscopic vascular invasion (no vs yes) |
0.354 |
|
N.A. |
0.017 |
|
N.A. |
| Portal vein invasion (no vs yes) |
0.004 |
|
N.A. |
0.348 |
|
N.A. |
| BCLC stage (A vs B/C) |
3.3E-08 |
2.738 (1.602-4.679) |
2.3E-04 |
2.2E-07 |
|
N.A. |
| TNM stage (I vs II /III) |
1.8E-07 |
|
N.A. |
3.4E-08 |
3.597 (2.046-6.324) |
8.8E-06 |
| Necroinflammatory grade (<9 vs ≥9) |
0.001 |
|
N.A. |
0.003 |
1.837 (1.087-3.105) |
0.023 |
| Fibrotic stage (≤4 vs >4) |
0.014 |
|
N.A. |
0.103 |
|
N.A. |
| DR (<2 vs ≥2) |
2.6E-05 |
4.294 (2.255-8.177) |
9.3E-06 |
4.8E-04 |
2.380 (1.250-4.534) |
0.008 |
| Liver ischemic time, min (≤25 vs >25) |
0.760 |
|
N.A. |
0.683 |
|
N.A. |
| Blood loss, ml (<800 vs ≥800) |
0.007 |
|
N.A. |
0.063 |
|
N.A. |
| Blood transfusion (yes vs no) | 0.089 | N.A. | 0.071 | N.A. | ||
The median was used as cut-off of necroinflammatory grade, fibrotic stage and DR respectively. Variables with p <0.05 in univariate analysis were adopted for multivariate analysis. Tumor size and DR were included, other covariates including tumor number, tumor capsule and portal vein invasion were then excluded.
Factors demonstrated to be significant in univariate analysis were then used into the Cox proportional hazards regression model for multivariate analysis. Both DR and tumor size were independent prognostic factors for RFS and OS. DR was associated with elevated risks of recurrence (HR = 2.380, 95% CI = 1.250-4.534, p = 0.008) and death (HR = 4.294, 95% CI = 2.255-8.177, p = 9.3E-06). Tumor size was associated with elevated risks of recurrence (HR = 1.804, 95% CI = 1.057-3.080, p = 0.031) and death (HR = 2.950, 95% CI = 1.694-5.137, p = 1.3E-04). Besides, TNM and necroinflammatory grade were demonstrated as independent predictors for RFS; while BCLC stage was independent prognostic factors for OS.
There are two types of recurrence for HCC, one is early recurrence (true metastasis, ≤2 years after surgery) and the other is late recurrence (de novo cancer, >2 years after surgery) [21]. A total of 81/106 (76.4%) patients suffered from tumor recurrence, of whom 60/81 (74.1%) patients recurred within two years and 21/81 (26.0%) recurred more than two years after surgery. As shown in Table 2, patients with high DR were more likely to suffer from early recurrence compared with the low subgroup (8/52 vs 9/12, p = 0.010).
Discussion
To the best of our knowledge, this is the first study to identify peritumoral DR as an independent prognostic factor for HCC after resection. Patients with decreased peritumoral DR had a significantly prolonged OS and RFS compared with the increased subgroup. Therefore, patients with high peritumoral DR require closer follow-up after surgery, and peritumoral DR could also serve as a new biomarker predicting HCC recurrence.
DR occurs in cholestatic diseases, in inflammatory diseases and in conditions with massive loss of parenchyma [22-24]. Hence, three types of DR are classically recognized [11]. We precluded the DR which originated from bile ducts obstructive diseases or cholestatic parenchymal damage in 106 patients with HCC, so the DR we observed could represent an activation of HPCs. Intermediate hepatobiliary cells of several differentiation states are continuously being produced in a dynamic nature of DR [25]. These data are supported by our results (Figures 2 and 3). DR is thought to arise due to a complex interaction between hepatocytes, hepatic progenitor cells, hepatic stellate cells and extracellular matrix as well as inflammatory cells and endothelial cells [13]. The total necroinflammatory score was significantly associated with the expansion of DR (Table 1). The result is in agreement with recent findings [26]. There was a highly significant correlation between the area of DR and fibrotic stage [27]. It may be important in the development of fibrosis [28]. These data are supported by our result showing that DR was significantly correlated with fibrotic stage (Table 1). Insulin resistance and hepatic inflammation might cause liver fibrosis by the expansion of the DR and the occurrence of epithelial-mesenchymal transition (EMT) [27-29]. Our data showed that HPCs were in or closed to DR (Figures 2 and 3). Other authors proposed that DR is an important source of progenitor cells that can repopulate both the bile ductular and hepatocytic lineages in diseased liver [5,30].
HPCs expansion forms DR by provided “field-effects” of a continuing necroinflammatory microenvironment. They were evidenced by their location in close proximity to the DR, and the strong correlation between these two variables [27]. The combination of interferon-γ and tumor necrosis factor alpha, cytokines overexpressed in HCV (Hepatitis C virus) may inhibit primary hepatocyte replication and stimulate HPCs expansion [31-33]. Cellular signalling between HPCs and the surrounding nonparenchymal population is an important determinant of HPCs behaviour [34]. Our subsequent result showed that DR was higher in HBsAg (+) subgroup than in HBsAg (−), which meant that HPCs in DR expanded actively in HBsAg (+) (Table 2). ECM remodelling, such as fibrosis resolution and laminin deposition is likely to be important prerequisite to HPCs activation and expansion [35]. The collected evidence indicates that HPCs, in a suitable environment, could be induced to a direction of portal fibroblastic differentiation through EMT [36]. Chronic carbon tetrachloride (CCl4) administration to mice induces significant hepatic fibrosis and can induce a florid HPCs response in parallel with advanced fibrosis [37]. It was suggested that the HPC response may drive liver fibrogenesis rather than being a secondary event [38].
Inflammation can supply bioactive molecules to the tumor microenvironment, including limiting cancer cell death [39,40]. Necrotic cell death releases proinflammatory signals into the surrounding tissue microenvironment. As a consequence, necrotic cells can recruit inflammatory cells of the immune system [39,41]. Additionally, necrotic cells can release bioactive regulatory factors, such as IL-1a, which can directly stimulate neighboring viable cells to proliferate [39]. Incipient neoplasias and potentially invasive and metastatic tumors may gain an advantage by tolerating some degree of necrotic cell death, doing so in order to recruit tumor-promoting inflammatory cells that bring growth-stimulating factors to the surviving cells within these growths [42].
DR expressing CK perhaps contains ones deriving from malignant degeneration of HPCs. The CK-positive HCC cells play the leading role in directing aggressive behavior of the tumor cell population [43]. The presence of CK19 expression by >5% of cells in HCC is associated with a poor prognosis [8]. The study of CK expression in the liver provides a useful insight into the mechanisms underlying progenitor cell activity and tissue regeneration following liver damage. HPCs express CK7 and CK19 [44]. They potentially derive from malignant degeneration of HPCs. HCC expressing CK19 had a higher incidence of AFP expression [8]. Our data showed that increased CK19-immunoreactive DR correlated with elevated serum AFP (Table 2). The higher recurrence rate of CK19 (+) HCC after transplantation suggests a worse prognosis for HCC expressing CK19 as compared to CK19 (−) HCC [8].
There are two types of recurrence for HCC: one is early recurrence, the other is late recurrence [21]. Discriminating between these two types is necessary in order to determine the appropriate intervention after surgery. True metastasis would benefit from adjuvant chemotherapy, while de novo cancer would be prevented by better control of viral infection and/or cirrhosis [45]. Our data showed that patients with early recurrence had significantly higher DR compared with patients with late recurrence. Patients with recurrence had especially higher DR and high necroinflammation compared with patients without recurrence, indicating the importance of alleviating necroinflammation, protecting hepatic function and strengthening general immunity. DR correlates with the degree of inflammation and fibrosis in the course of many chronic human liver diseases. Inflammation can supply bioactive molecules to the tumor microenvironment that facilitates inductive signals that lead to activation of EMT [39]. Some results indicated the critical association between the metastasis and EMT [46]. Mesenchymal stem cells in inflammation microenvironment accelerate HCC Metastasis by Inducing EMT [47]. DR may undergo the process of EMT in patients with the highest grade of necroinflammation [26]. Maybe the higher peritumoral DR was the prognostic indicator for early recurrence after hepatectomy due to intrahepatic metastasis through EMT.
The lack of liver donation, highly cost of operation and post-operative treatment, caused that few liver transplantation was carried out in our hospital. OS rates after hepatectomy for HCC was low. 5-yr survival after hepatectomy for HCC was 32.1% in this series. Because there were 71 (67%) patients with HCC whose tumor size was more than 5 cm, and the tumor size was independent prognostic factors for RFS and OS in our study. On the other hand, 67 (63.2%) patients had B/C of BCLC stage, 71 (67%) patients had II/III of TNM stage. Our study showed that increased peritumoral DR often correlated with multiple nodules and the absence of a tumor capsule, which are two features of a highly invasive HCC phenotype. Our study also showed that increased peritumoral DR correlated with severe microscopic vascular invasion. The cases with peritumoral multiple portal vein invasions tend to show early recurrence after hepatic resection. That’s the reason why it is common in early recurrence. Therefore, a very close follow-up protocol is required for patients with increased DR because it usually reveals highly aggressive tumor behavior.
Conclusion
In conclusion, we demonstrated for the first time that peritumoral DR in a necroinflammatory microenvironment is a poor prognostic factor for HCC following Resection. A continuing necroinflammatory microenvironment provides “field-effects” for stimulating HPCs expansion to form DR and partly to be diverted to malignant direction. DR expressing CK19 perhaps contains ones deriving from malignant degeneration of HPCs. Maybe the pretumoral DR is the prognostic indicator for early recurrence after hepatectomy due to intrahepatic metastasis through EMT. This provides a rationale for anti-inflammatory, anti-EMT and HPCs targeted therapies in clinical practice. Further experiments are needed to reveal the mechanisms of DR, EMT and inflammatory cells.
Abbreviations
AFP: Alpha fetoprotein; BCLC stage: Barcelona-Clinic Liver Cancer stage; CCl4: Chronic carbon tetrachloride; DR: Ductular reaction; EMT: Epithelial-mesenchymal transition; HCC: Hepatocellular carcinoma; HCV: Hepatitis C virus; HPCs: Hepatic progenitor cells; OS: Overall survival time; RFS: Recurrence-free survival time.
Competing interests
The authors have declared that no competing interests exist.
Authors’ contributions
JiY and LW designed the research; MX, FX, YJ, SZ, LG, and TZ performed the research; MX, GQ and MW analyzed the data; and MX and FX wrote the paper. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Minhui Xu, Email: xmh_8976@163.com.
Feng Xie, Email: hunanxiefeng@yahoo.com.
Guangyang Qian, Email: qiangguangyang@gmail.com.
Yingying Jing, Email: Jingy4172@163.com.
Shanshan Zhang, Email: drzhangss@163.com.
Lu Gao, Email: mouse.520@163.com.
Tao Zheng, Email: jefferyzheng@yeah.net.
Mengchao Wu, Email: qiufujian@sina.com.
Jiamei Yang, Email: jiameiyang@gmail.com.
Lixin Wei, Email: weilixin@yahoo.com.
Acknowledgements
We thank Dr. Jia He for the expert help in statistical analysis.
References
- Zhou WP, Lai EC, Li AJ, Fu SY, Zhou JP, Pan ZY, Lau WY, Wu MC. A prospective, randomized, controlled trial of preoperative transarterial chemoembolization for resec large hepatocellular carcinoma. Ann Surg. 2009;249(2):195–202. doi: 10.1097/SLA.0b013e3181961c16. [DOI] [PubMed] [Google Scholar]
- Llovet JM, Bruix J. Molecular targeted therapies in hepatocellular carcinoma. Hepatology. 2008;48(4):1312–1327. doi: 10.1002/hep.22506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arciero CA, Sigurdson ER. Liver-directed therapies for patients with primary liver cancer and hepatic metastases. Curr Treat Options Oncol. 2006;7(5):399–409. doi: 10.1007/s11864-006-0008-7. [DOI] [PubMed] [Google Scholar]
- Roskams T, Katoonizadeh A, Komuta M. Hepatic progenitor cells: an update. Clin Liver Dis. 2010;14(4):705–718. doi: 10.1016/j.cld.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Roskams TA, Theise ND, Balabaud C, Bhagat G, Bhathal PS, Bioulac-Sage P, Brunt EM, Crawford JM, Crosby HA, Desmet V. et al. Nomenclature of the finer branches of the biliary tree: canals, ductules, and ductular reactions in human livers. Hepatology. 2004;39(6):1739–1745. doi: 10.1002/hep.20130. [DOI] [PubMed] [Google Scholar]
- Knight B, Matthews VB, Olynyk JK, Yeoh GC. Jekyll and Hyde: evolving perspectives on the function and potential of the adult liver progenitor (oval) cell. Bioessays. 2005;27(11):1192–1202. doi: 10.1002/bies.20311. [DOI] [PubMed] [Google Scholar]
- Libbrecht L, Desmet V, Van Damme B, Roskams T. The immunohistochemical phenotype of dysplastic foci in human liver: correlation with putative progenitor cells. J Hepatol. 2000;33(1):76–84. doi: 10.1016/s0168-8278(00)80162-2. [DOI] [PubMed] [Google Scholar]
- Durnez A, Verslype C, Nevens F, Fevery J, Aerts R, Pirenne J, Lesaffre E, Libbrecht L, Desmet V, Roskams T. The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology. 2006;49(2):138–151. doi: 10.1111/j.1365-2559.2006.02468.x. [DOI] [PubMed] [Google Scholar]
- Yang XR, Xu Y, Yu B, Zhou J, Qiu SJ, Shi GM, Zhang BH, Wu WZ, Shi YH, Wu B. et al. High expression levels of putative hepatic stem/progenitor cell biomarkers related to tumour angiogenesis and poor prognosis of hepatocellular carcinoma. Gut. 2010;59(7):953–962. doi: 10.1136/gut.2008.176271. [DOI] [PubMed] [Google Scholar]
- Roskams T. Liver stem cells and their implication in hepatocellular and cholangiocarcinoma. Oncogene. 2006;25(27):3818–3822. doi: 10.1038/sj.onc.1209558. [DOI] [PubMed] [Google Scholar]
- Roskams T, Desmet V. Ductular reaction and its diagnostic significance. Semin Diagn Pathol. 1998;15(4):259–269. [PubMed] [Google Scholar]
- Park YN, Kojiro M, Di Tommaso L, Dhillon AP, Kondo F, Nakano M, Sakamoto M, Theise ND, Roncalli M. Ductular reaction is helpful in defining early stromal invasion, small hepatocellular carcinomas, and dysplastic nodules. Cancer. 2007;109(5):915–923. doi: 10.1002/cncr.22460. [DOI] [PubMed] [Google Scholar]
- Bateman AC, Hubscher SG. Cytokeratin expression as an aid to diagnosis in medical liver biopsies. Histopathology. 2010;56(4):415–425. doi: 10.1111/j.1365-2559.2009.03391.x. [DOI] [PubMed] [Google Scholar]
- Knight B, Matthews VB, Akhurst B, Croager EJ, Klinken E, Abraham LJ, Olynyk JK, Yeoh G. Liver inflammation and cytokine production, but not acute phase protein synthesis, accompany the adult liver progenitor (oval) cell response to chronic liver injury. Immunol Cell Biol. 2005;83(4):364–374. doi: 10.1111/j.1440-1711.2005.01346.x. [DOI] [PubMed] [Google Scholar]
- Freeman A, Hamid S, Morris L, Vowler S, Rushbrook S, Wight DG, Coleman N, Alexander GJ. Improved detection of hepatocyte proliferation using antibody to the pre-replication complex: an association with hepatic fibrosis and viral replication in chronic hepatitis C virus infection. J Viral Hepat. 2003;10(5):345–350. doi: 10.1046/j.1365-2893.2003.00454.x. [DOI] [PubMed] [Google Scholar]
- Mantovani A. Cancer: Inflaming metastasis. Nature. 2009;457(7225):36–37. doi: 10.1038/457036b. [DOI] [PubMed] [Google Scholar]
- Libbrecht L, Desmet V, Van Damme B, Roskams T. Deep intralobular extension of human hepatic ‘progenitor cells’ correlates with parenchymal inflammation in chronic viral hepatitis: can ‘progenitor cells’ migrate? J Pathol. 2000;192(3):373–378. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH700>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Kuang DM, Peng C, Zhao Q, Wu Y, Chen MS, Zheng L. Activated monocytes in peritumoral stroma of hepatocellular carcinoma promote expansion of memory T helper 17 cells. Hepatology. 2010;51(1):154–164. doi: 10.1002/hep.23291. [DOI] [PubMed] [Google Scholar]
- Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F, Denk H, Desmet V, Korb G, MacSween RN. et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22(6):696–699. doi: 10.1016/0168-8278(95)80226-6. [DOI] [PubMed] [Google Scholar]
- Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, von der Maase H. Presence of intratumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J Clin Oncol. 2009;27(28):4709–4717. doi: 10.1200/JCO.2008.18.9498. [DOI] [PubMed] [Google Scholar]
- Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, Sugawara Y, Minagawa M, Takayama T, Kawasaki S. et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38(2):200–207. doi: 10.1016/s0168-8278(02)00360-4. [DOI] [PubMed] [Google Scholar]
- Desmet VJ. Modulation of the liver in cholestasis. J Gastroenterol Hepatol. 1992;7(3):313–323. doi: 10.1111/j.1440-1746.1992.tb00988.x. [DOI] [PubMed] [Google Scholar]
- Liu Z, Sakamoto T, Ezure T, Yokomuro S, Murase N, Michalopoulos G, Demetris AJ. Interleukin-6, hepatocyte growth factor, and their receptors in biliary epithelial cells during a type I ductular reaction in mice: interactions between the periductal inflammatory and stromal cells and the biliary epithelium. Hepatology. 1998;28(5):1260–1268. doi: 10.1002/hep.510280514. [DOI] [PubMed] [Google Scholar]
- Roskams TA, Libbrecht L, Desmet VJ. Progenitor cells in diseased human liver. Semin Liver Dis. 2003;23(4):385–396. doi: 10.1055/s-2004-815564. [DOI] [PubMed] [Google Scholar]
- Zhou H, Rogler LE, Teperman L, Morgan G, Rogler CE. Identification of hepatocytic and bile ductular cell lineages and candidate stem cells in bipolar ductular reactions in cirrhotic human liver. Hepatology. 2007;45(3):716–724. doi: 10.1002/hep.21557. [DOI] [PubMed] [Google Scholar]
- Svegliati-Baroni G, Faraci G, Fabris L, Saccomanno S, Cadamuro M, Pierantonelli I, Trozzi L, Bugianesi E, Guido M, Strazzabosco M. et al. Insulin resistance and necroinflammation drives ductular reaction and epithelial-mesenchymal transition in chronic hepatitis C. Gut. 2011;60(1):108–115. doi: 10.1136/gut.2010.219741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston AD, Powell EE, Walsh MJ, Richardson MM, Demetris AJ, Jonsson JR. Fibrosis correlates with a ductular reaction in hepatitis C: roles of impaired replication, progenitor cells and steatosis. Hepatology. 2005;41(4):809–818. doi: 10.1002/hep.20650. [DOI] [PubMed] [Google Scholar]
- Richardson MM, Jonsson JR, Powell EE, Brunt EM, Neuschwander-Tetri BA, Bhathal PS, Dixon JB, Weltman MD, Tilg H, Moschen AR. et al. Progressive fibrosis in nonalcoholic steatohepatitis: association with altered regeneration and a ductular reaction. Gastroenterology. 2007;133(1):80–90. doi: 10.1053/j.gastro.2007.05.012. [DOI] [PubMed] [Google Scholar]
- Fabris L, Cadamuro M, Guido M, Spirli C, Fiorotto R, Colledan M, Torre G, Alberti D, Sonzogni A, Okolicsanyi L. et al. Analysis of liver repair mechanisms in Alagille syndrome and biliary atresia reveals a role for notch signaling. Am J Pathol. 2007;171(2):641–653. doi: 10.2353/ajpath.2007.070073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J, Hytiroglou P, Wieczorek R, Park YN, Thung SN, Arias B, Theise ND. Immunohistochemical evidence for hepatic progenitor cells in liver diseases. Liver. 2002;22(5):365–373. doi: 10.1034/j.1600-0676.2002.01622.x. [DOI] [PubMed] [Google Scholar]
- Napoli J, Bishop GA, McGuinness PH, Painter DM, McCaughan GW. Progressive liver injury in chronic hepatitis C infection correlates with increased intrahepatic expression of Th1-associated cytokines. Hepatology. 1996;24(4):759–765. doi: 10.1002/hep.510240402. [DOI] [PubMed] [Google Scholar]
- Gochee PA, Jonsson JR, Clouston AD, Pandeya N, Purdie DM, Powell EE. Steatosis in chronic hepatitis C: association with increased messenger RNA expression of collagen I, tumor necrosis factor-alpha and cytochrome P450 2E1. J Gastroenterol Hepatol. 2003;18(4):386–392. doi: 10.1046/j.1440-1746.2003.02984.x. [DOI] [PubMed] [Google Scholar]
- Fausto N. Liver regeneration and repair: hepatocytes, progenitor cells, and stem cells. Hepatology. 2004;39(6):1477–1487. doi: 10.1002/hep.20214. [DOI] [PubMed] [Google Scholar]
- Bird TG, Lorenzini S, Forbes SJ. Activation of stem cells in hepatic diseases. Cell Tissue Res. 2008;331(1):283–300. doi: 10.1007/s00441-007-0542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallis YN, Robson AJ, Fallowfield JA, Thomas HC, Alison MR, Wright NA, Goldin RD, Iredale JP, Forbes SJ. Remodelling of extracellular matrix is a requirement for the hepatic progenitor cell response. Gut. 2011;60(4):525–533. doi: 10.1136/gut.2010.224436. [DOI] [PubMed] [Google Scholar]
- Deng H, Wang HF, Gao YB, Jin XL, Xiao JC. Hepatic progenitor cell represents a transitioning cell population between liver epithelium and stroma. Med Hypotheses. 2011;76(6):809–812. doi: 10.1016/j.mehy.2011.02.024. [DOI] [PubMed] [Google Scholar]
- Pritchard MT, Nagy LE. Hepatic fibrosis is enhanced and accompanied by robust oval cell activation after chronic carbon tetrachloride administration to Egr-1-deficient mice. Am J Pathol. 2010;176(6):2743–2752. doi: 10.2353/ajpath.2010.091186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston AD, Jonsson JR, Powell EE. Hepatic progenitor cell-mediated regeneration and fibrosis: chicken or egg? Hepatology. 2009;49(5):1424–1426. doi: 10.1002/hep.22893. [DOI] [PubMed] [Google Scholar]
- Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White E, Karp C, Strohecker AM, Guo Y, Mathew R. Role of autophagy in suppression of inflammation and cancer. Curr Opin Cell Biol. 2010;22(2):212–217. doi: 10.1016/j.ceb.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Lu XY, Xi T, Lau WY, Dong H, Zhu Z, Shen F, Wu MC, Cong WM. Hepatocellular carcinoma expressing cholangiocyte phenotype is a novel subtype with highly aggressive behavior. Ann Surg Oncol. 2011;18(8):2210–2217. doi: 10.1245/s10434-011-1585-7. [DOI] [PubMed] [Google Scholar]
- Roskams T, De Vos R, Van Eyken P, Myazaki H, Van Damme B, Desmet V. Hepatic OV-6 expression in human liver disease and rat experiments: evidence for hepatic progenitor cells in man. J Hepatol. 1998;29(3):455–463. doi: 10.1016/s0168-8278(98)80065-2. [DOI] [PubMed] [Google Scholar]
- Li YW, Qiu SJ, Fan J, Zhou J, Gao Q, Xiao YS, Xu YF. Intratumoral neutrophils: a poor prognostic factor for hepatocellular carcinoma following Resection. J Hepatol. 2011;54(3):497–505. doi: 10.1016/j.jhep.2010.07.044. [DOI] [PubMed] [Google Scholar]
- Larue L, Bellacosa A. Epithelial-mesenchymal transition in development and cancer: role of phosphatidylinositol 3′ kinase/AKT pathways. Oncogene. 2005;24(50):7443–7454. doi: 10.1038/sj.onc.1209091. [DOI] [PubMed] [Google Scholar]
- Jing Y, Han Z, Liu Y, Sun K, Zhang S, Jiang G, Li R, Gao L, Zhao X, Wu D. et al. Mesenchymal stem cells in inflammation microenvironment accelerates hepatocellular carcinoma metastasis by inducing epithelial-mesenchymal transition. PLoS One. 2012;7(8):e43272. doi: 10.1371/journal.pone.0043272. [DOI] [PMC free article] [PubMed] [Google Scholar]