Summary
Through the years, the burn injury has been described using a variety of labels. These labels have ranged from one word terms to phrases including degrees of injury or more descriptive terms. A search was conducted relying on a common general internet search engine. After multiple searches varying the keywords, the top 100 searches identified the most prevalent terms or phrases, ranging from the common to the more obscure. The search was repeated using the most prevalent terms or phrases identified in the common internet search engine, focusing on either the title or abstract for all papers indexed in PubMed. This process narrowed the attention to the most common terms or phrases used by the academics in their published work. This work therefore focused on measuring the specific terms being used today and their frequency of use in the peer reviewed papers indexed in the PubMed system. It is difficult to focus on the unique aspects of any given profession when there is confusion surrounding a common vocabulary. By identifying and noting in the academic literature the most commonly used labels, a point of reference can be created for future work. Furthermore, having a common and accurate set of labels that are uniformly applied across the profession is critical for academia to include in training and education programs for physicians, nurses, and paramedical staff.
Keywords: burn assessment, burn education, superficial burn, partial thickness burn, full thickness burn
Abstract
Au fil des ans, la brûlure a été décrite en utilisant une variété d'étiquettes. Ces étiquettes ont oscillé entre un seul mot et des phrases, y compris degrés de blessures ou de termes plus descriptifs. Une recherche a été menée en s'appuyant sur un moteur de recherche internet. Après de multiples recherches variant les mots-clés, le top 100 des termes de recherche identifié ou expressions les plus courantes, allant de la commune à la plus obscure. La recherche a été répétée en utilisant des termes ou des expressions les plus fréquentes identifiées dans le moteur de recherche internet, en mettant l'accent soit sur le titre ou le résumé de tous les articles indexés dans PubMed. Ce processus réduit l'attention de termes ou expressions les plus courantes utilisées par les professeurs dans leur travail publié. Par conséquent, ce travail a porté sur la mesure des termes spécifiques qui sont utilisées aujourd'hui et leur fréquence d'utilisation dans les journaux évalués par les pairs indexées dans le système PubMed. Il est difficile de se concentrer sur les aspects spécifiques de chaque profession donnée quand il y a confusion entourant un vocabulaire commun. En identifiant et en notant dans la littérature académique les étiquettes les plus couramment utilisées, un point de référence peut être créé pour les travaux futurs. En outre, un ensemble commun et précis des étiquettes qui sont appliqués uniformément à travers la profession est essentiel pour les universités à inclure dans les programmes de formation et d'éducation pour les médecins, les infirmières et le personnel paramédical.
Introduction
Burn injury remains one of the time sensitive injuries and illnesses which substantially challenge healthcare professionals around the world.1,2 According to the American Burn Association (ABA), there are approximately 450,000 burn injuries each year in the United States (US).3 Given that the US represents approximately 5% of the world population, a conservative extrapolation would suggest that annually, there are 10,000,000 burns worldwide. This approximation is close to the figure reported by the World Health Organization (WHO) in 2004, where “nearly 11 million people worldwide required medical attention for a burn injury,” according to the most recent data available on a 2012 fact sheet from the WHO.4
It is reasonable to presume clinicians have a basic understanding of burn care and how to assess and describe the different severity of burn injuries for pediatric and adult patients. 5-9 However, several years of anecdotal experiences by the authors suggested a lack of consensus when discussing even the most basic elements of burn care; the labels used to stratify the different levels of injury acuity. This inconsistent use of descriptive terms and phrases can also impact public education10 and burn prevention programs11-14 as well as those programs used to target specific burn care providers such as Advanced Burn Life Support (ABLS)15,16 and Emergency Management of Severe Burns (EMSB).17-19
During the past several years of reviewing more than a thousand articles related to burn injury, traumatic injury or disaster medicine, it was apparent that there is an ongoing inconsistent use of terms and phrases to describe the varying types of burn injury. It is difficult to evaluate academic papers or develop educational programs when there are multiple terms and phrases used to identify the same injury.
The aim of this work began with identifying the most prevalent terms or phrases used to label a burn injury in a general search of internet based references. Then using those results to conduct a more focused search of the PubMed database to identify how often those most commonly used terms/phrases were the labels of choice. Although much of what is found through typical search engines lacks the rigors of academic peer reviewed efforts, it was a reasonable source to help bring into focus and narrow the search. Furthermore, it serves as a reminder of the significant inconsistency throughout the general population, even when describing the most basic types of burn injury.
Methods
A preliminary search was conducted by entering the phrase “burn injury” into the Google search engine, which yielded “about 8,600,000” results.20 Each of the 100 highest rated hits was further categorized with the focus on narrowing the search for use in PubMed. Based on the Google search results, there were 11 terms or phrases identified in the 100 highest rated hits. In no particular order, the findings identified included: First (1st) Degree Burn, Second (2nd) Degree Burn, Third (3rd) Degree Burn, Fourth (4th) Degree Burn, Fifth (5th) Degree Burn, Sixth (6th) Degree Burn, Superficial Burn, Partial Thickness Burn, Deep Partial Thickness Burn, Full Thickness Burn and Severe Burn Injury. Each of these 11 terms/phrases were then used with the exact match function in PubMed, searching either the title or the abstract for hits using one or more of these 11 terms/phrases. The start date was the most recent published as of November 1, 2012, and the last article included in the search was published on or after January 1, 2000. All earlier references were not included and those results were not evaluated or recorded for this work.
The search parameters included an exact phrase either located in the title or the abstract and all other fields were not included in the search. After each of the 11 searches was conducted, the findings were evaluated to determine if there were other questions created by the manner in which the search was conducted. After each search, the findings were recorded and the process ended after the 11 searches.
Results
The common internet search engine data produced eleven (11) terms/phrases that were used to describe a burn injury in the context of stratifying the severity of the burn injury. A total of 1110 academic papers in the PubMed search reflected one or more of the 11 terms/phrases identified through the common internet search. All of the 1110 papers identified for inclusion based on the search criteria, focused primarily on one specific burn injury and included one or more of the terms/phrases. Where more than one of the target terms/phrases was identified in the search, the paper was further reviewed to determine if the focus of the work included more than one of the burn injuries identified. There were 9/11 (81.8%) of the terms/phrases identified using the common internet search engine which were also found in the PubMed search. There were 2/11 (18.2%) terms/phrases identified in the common internet search engine that were not identified in the PubMed search. Those not found in the PubMed search included the Fifth (5th) Degree Burn and the Sixth (6th) Degree Burn.
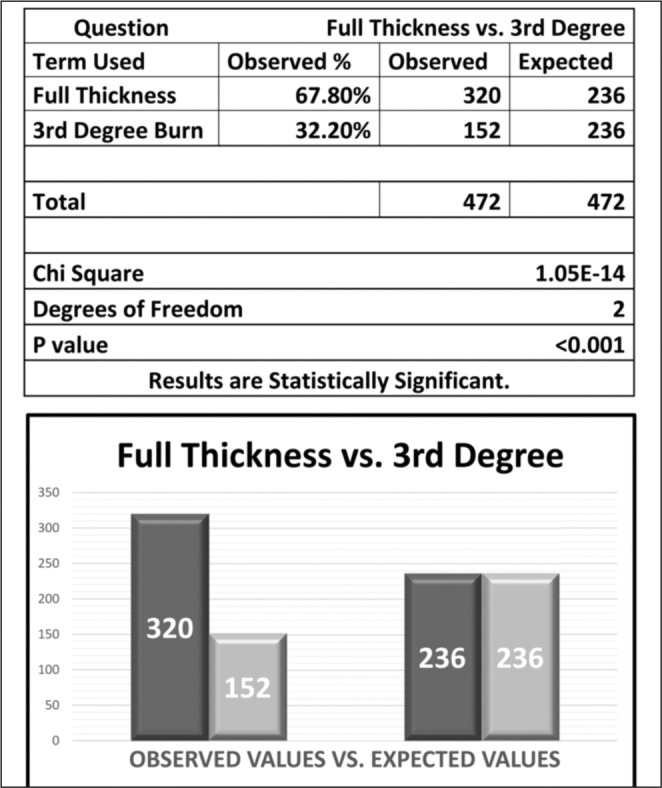
Given that the Superficial Burn and the First (1st) Degree Burn describe basically the same injury, they were compared in use. A total of 55 papers were identified that met inclusion criteria and of which Superficial Burn represented 40/55 (72.7%)21 while First (1st) Degree Burn represented 10/55 (27.3%)22 (Fig. 1). The same comparison was made involving the Partial Thickness Burn and the Second (2nd) Degree Burn. A total of 271 papers were identified that met inclusion criteria of which 180/271 (66.4%)23 were identified as Partial Thickness Burn and 91/271 (33.6%)24 were identified as a Second (2nd) Degree Burn (Fig. 2). The Full Thickness Burn was compared to the Third (3rd) Degree Burn. A total of 472 papers were identified that met inclusion criteria of which 320/472 (67.8%)25 used the term/phrase Full Thickness Burn compared to 152/472 (32.3%)26 using the term/phrase Third (3rd) Degree Burn (Fig. 3). Use of the term Fourth (4th) degree burn injury27 was also found in 7 seven academic papers, where this was described as being a Full Thickness Burn that extended beyond the hypodermis into the muscle tissue or muscle and bone. There were no papers that matched either Fifth (5th)28 or Sixth (6th)29 Degree Burn in the search results. There were, however, 76 academic papers that discussed a Deep Partial Thickness Burn.30 As one would presume, the injury described in the 76 papers generally shared characteristics of the Partial Thickness Burn and the Full Thickness Burn.
Fig. 1. Findings for the use of “Superficial Burn” when compared to “First (1st) Degree Burn” as a description in Peer Reviewed Articles.
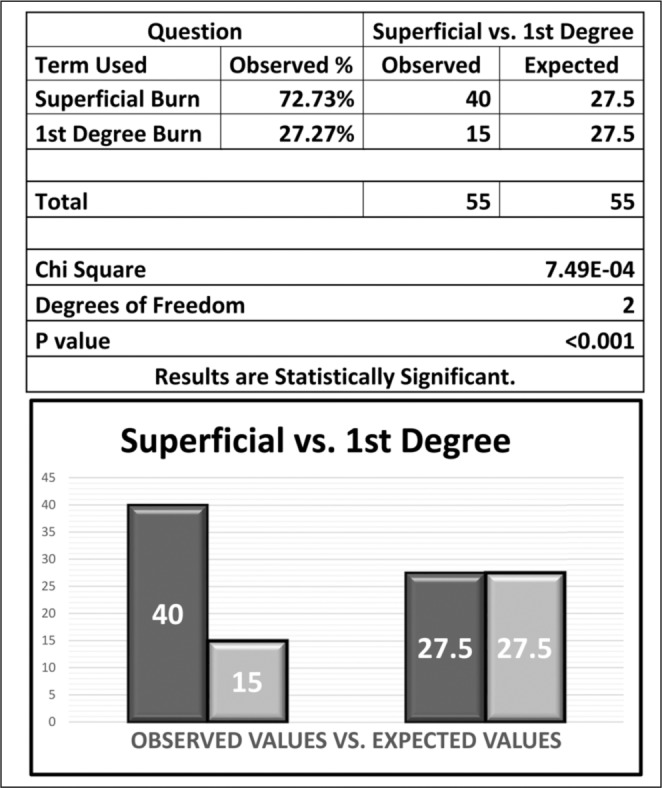
Fig. 2. Findings for the use of “Partial Thickness Burn” when compared to “Second (2nd) Degree Burn” as a description in Peer Reviewed Articles.
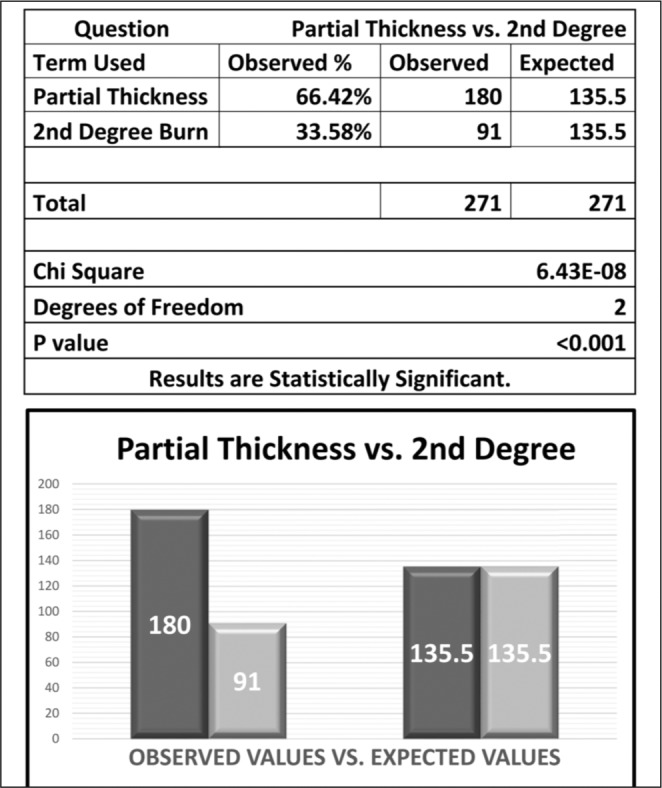
Fig. 3. Findings for the use of “Full Thickness Burn” when compared to “Third (3rd) Degree Burn” as a description in Peer Reviewed Articles.
A common phrase also used was the Severe Burn Injury (SBI).31 The phrase was identified in 229 academic papers published after January 1, 2000. All of the papers reviewed used SBI as a general category to describe the Partial Thickness Burn, Full Thickness Burn and Deep Partial Thickness Burn. There were no incongruent findings. Specifically, at no point did the researchers find that Superficial Burn was used to describe a Second (2nd) Degree Burn or a Third (3rd) Degree Burn. Furthermore, at no point was a Partial Thickness Burn used to describe a First (1st) Degree Burn or a Third (3rd) Degree Burn. Finally, the Full Thickness Burn was not used to describe a First (1st) Degree Burn or a Second (2nd) Degree Burn.
Discussion
Logic suggests, for the sake of consistency in a given profession, it is important to use one common set of terms to describe these critical aspects of a burn injury.7 Also, injury to one or more of the three layers of skin is generally the focal point of the evaluation during the burn injury assessment.32 As such, is further stratification for burn injury that extends beyond the hypodermis into muscle tissue necessary? How about burn injury that involves bone or muscle tissue beyond the three layers of skin?
If the only point of contention was whether to use the term “First (1st) Degree Burn” or “Superficial Burn,” the findings suggest those arguments are settled for a clear majority in the scientific community publishing their work in peer reviewed journals. However, the bigger issue concerns the number of papers that described the Deep Partial Thickness Burn. If the answer remains that there are three layers of skin and thus there are three levels of burn injury, what becomes of this label? Since the initial assessment and care of the Deep Partial Thickness Burn is approximately the same as the Full Thickness Burn and, moreover, is also the same as that for the Fourth (4th) Degree Burn as identified in the common search, it is logical that all should fall under the Full Thickness Burn classification for the initial assessment and treatment.
In the US, there is a trend to associate descending numbers with one being either the best service or serving the most critical conditions, such as Level I Trauma Center33 or a Type I National Incident Management System (NIMS) resource. 34,35 To follow that logic alone would suggest abandoning the historical use of 1st, 2nd and 3rd degree burns is a reasonable evolution since it runs counterintuitive to what is currently in use in the medical and disaster profession. Nevertheless, that may be more applicable to the US and offer less value to the greater international perspective.
Conclusions and recommendations
A review of the literature indicates a clear preference to use descriptive terminology rather than degrees of injury. Generally, this transition from degrees of injury to descriptive terms has been taking place in the literature for the past 12+ years, and today the more favored terms include Superficial, Partial Thickness and Full Thickness as the three main descriptions of burn injury.
Our findings reveal a clear majority of academics who publish their research using mainly descriptive terms to label the different stratifications of burn injury: Superficial Burn, Partial Thickness Burn and Full Thickness Burn in lieu of First (1st), Second (2nd) and Third (3rd) Degree Burns. Given the limited use of a Fourth (4th) Degree Burn and the absence of peer reviewed published works referring to a Fifth (5th) and Sixth (6th) Degree Burn, the clear majority are using descriptive terms to label a burn injury and use of anything beyond a Full Thickness Burn is either rare or non-existent.
The finding for the prevalence of the use of Deep Partial Thickness Burn is somewhat of a paradox. Given there were 76 published papers using this label, it clearly has relevance to those publishing their work. However, a common theme in many of these academic papers included the depth and degree of injury as well as the extent of care needed to manage this patient. Maybe the best place to suggest the use of this label is in the context of assessment and care confined within a Burn Center or where specialized burn care is provided.
It is the conclusion and recommendation of these authors to adopt and encourage colleagues to focus on a common language to describe the initial burn injury assessment. For initial assessment and care that begins in the pre-hospital setting, and continues at the community hospital level, the labels Superficial, Partial Thickness and Full Thickness should be the standard nomenclature. It is further recommended that the Superficial Burn be left in a category of its own, such as a Minor Burn Injury (MBI), as another way to remind clinicians to exclude the impact of the MBI when calculating the TBSA. Those burn injuries that are included in the rule of nines calculation, that is the Partial Thickness and Full Thickness Burn, would thus be classified as a Severe Burn Injury (SBI) (Fig. 4).
Fig. 4. Burn Injury assessment to reflect TBSA inclusion/exclusion criteria. This also includes where Deep Partial Thickness Burn should be assessed and managed. Partial, Deep Partial and Full Thickness burns smaller than 10% TBSA, may be classified as a MBI but should be assessed before reaching that conclusion. Location of Assessment will vary based on resource availability. Burn and Trauma Centers are not routinely available worldwide.
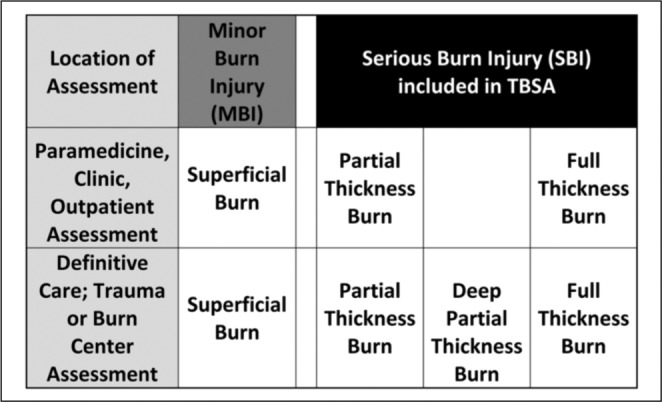
In the context of the diagnostic setting where definitive care is provided, such as a Trauma Center or a Burn Center, the Deep Partial Thickness Burn should be limited to the diagnostic clinician. This too will fall within the SBI classification, since the use of the more descriptive term implies the person performing the assessment has a more common working knowledge of burn injury than the typical clinician who seldom manages serious burn injuries.
Burn care is a global healthcare issue, and it could be concluded from the findings that, as a profession, there is a lack of consensus to even discuss the most fundamental aspects of assessing a burn injury. However, we now have a unique opportunity to coalesce around something simple, and in demonstrating a willingness to tackle the simple, there will be hope for consensus as more difficult problems are confronted that have confounded researchers in burn injury and burn care.
Acknowledgments
Funding. This work is supported in part by the US DHHS/ASPR Hospital Preparedness Program Grant CDC-RFA-TP12-1201 through the North Carolina Office of Emergency Medical Services Contract 00027162.
The authors of this paper would also like to acknowledge the support of their educational programs through FEMA Grant EMW-2011-FP-01131.
References
- 1.Atiyeh BS, Gunn SW, Hayek SN. State of the art in burn treatment. World Journal of Surgery. 2005;29:131–48. doi: 10.1007/s00268-004-1082-2. [DOI] [PubMed] [Google Scholar]
- 2.Resources for Optimal Care of the Injured Patient, Association AB; 2006. [Google Scholar]
- 3.Burn Incidence and Treatment in the United States: 2011 Fact Sheet. Association AB; 2011. [Accessed September 2, 2012]. http://www.ameriburn.org/resources_factsheet.php . [Google Scholar]
- 4.Burns: Fact sheet N°365. Organization WH; 2012. [Accessed December 26, 2012]. http://www.who.int/mediacentre/factsheets/fs365/en/index.html . [Google Scholar]
- 5.Reed JL, Pomerantz WJ. Emergency management of pediatric burns. Pediatric Emergency Care. 2005;21:118–29. doi: 10.1097/01.pec.0000159058.95424.0d. [DOI] [PubMed] [Google Scholar]
- 6.Mlcak R, Cortiella J, Desai MH, Herndon DN. Emergency management of pediatric burn victims. . Pediatric Emergency Care. 1988;14:51–54. doi: 10.1097/00006565-199802000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Ahlers-Schmidt CR, Wetta-Hall R, Berg-Copas G, Jost JC, Jost J. Evaluating program effectiveness: Creating a reliable and valid tool. J Contin Educ Nurs. 2008;39:139–44. doi: 10.3928/00220124-20080301-02. [DOI] [PubMed] [Google Scholar]
- 8.Wetta-Hall R, Jost JC, Jost G, Praheswari Y, Berg-Copas GM. Preparing for burn disasters: Evaluation of a continuing education training course for pre-hospital and hospital professionals in Kansas. J Burn Care Res. 2007:97–104. doi: 10.1097/BCR.0B013E31802Cb815. [DOI] [PubMed] [Google Scholar]
- 9.Notzer N, Eldad A, Donchin Y. Assessment of physician competence in prehospital trauma care. Injury. 1995;26:471–4. doi: 10.1016/0020-1383(95)00075-k. [DOI] [PubMed] [Google Scholar]
- 10.Parmer JE, Corso PS, Ballesteros MF, et al. A cost analysis of a smoke alarm installation and fire safety education program. J Safety Res. 2006;37:367–73. doi: 10.1016/j.jsr.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Atiyeh BS, Costagliola M, Hayek SN. Burn prevention mechanisms and outcomes: pitfalls, failures and successes. Burns: Journal of the International Society for Burn Injuries. 2009;35:181–93. doi: 10.1016/j.burns.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Eldad A, Salmon AY, Breiterman S, Chaouat M, BenBassat H. Flame burn protection: Assessment of a new, air-cooled fireproof garment. Mil Med. 2003;168:595–9. [PubMed] [Google Scholar]
- 13.Grant E, Turney E, Bartlett M, Winbon C, Peterson HD. Evaluation of a burn prevention program in a public school system. J Burn Care Rehabil. 1992;13:703–7. [PubMed] [Google Scholar]
- 14.Peleg K, Goldman S, Sikron F, et al. Burn prevention programs for children: Do they reduce burn-related hospitalizations? Burns: Journal of the International Society for Burn Injuries. 2005;31:347–50. doi: 10.1016/j.burns.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 15.Sasaki J, Takuma K, Oda J, et al. Experiences in organizing advanced burn life support (ABLS) provider courses in Japan. Burns: Journal of the International Society for Burn Injuries. 2010;36:65–9. doi: 10.1016/j.burns.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 16.Wolak E, Klish K, Smith E, Cairns BA. Educational opportunities for experienced staff: Do they make a difference? J Nurses Staff Dev. 2006;22:181–6. doi: 10.1097/00124645-200607000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Stone CA, Pape SA. Evolution of the emergency management of severe burns (EMSB) course in the UK. Burns: Journal of the International Society for Burn Injuries. 1999;25:262–4. doi: 10.1016/s0305-4179(98)00161-2. [DOI] [PubMed] [Google Scholar]
- 18.Lindford AJ, Lamyman MJ, Lim P. Review of the emergency management of severe burns (EMSB) course. Burns: Journal of the International Society for Burn Injuries. 2006;32:391. doi: 10.1016/j.burns.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Rogers AD, Allorto NL, Wallis LA, Rode H. The emergency management of severe burns course in South Africa. South African Journal of Surgery. 2013;51:38. doi: 10.7196/sajs.1309. [DOI] [PubMed] [Google Scholar]
- 20.Google: Google Search Engine Query. 2012. [Accessed November 1, 2012]. https://www.google.com/#hl=en&gs_rn=12&gs_ri=psy-ab&cp=11&gs_id=16&xhr=t&q=burn+injury&es_nrs=true&pf=p&output=search&sclient=psy-ab&oq=burn+injury&gs_l=&pbx=1&bav=on.2,or.r_qf.&bvm=bv.46226182,d.eWU&fp=feb58d80aebd244e&biw=1920&bih=983.
- 21.PubMed Search “Superficial Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=superficial%20burn%5BTitle%2FAbstract%5D .
- 22.PubMed Search “First Degree Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=first%20degree%20burn%5BTitle%2FAbstract%5D .
- 23.PubMed Search "Partial Thickness Burn". 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=partial%20thickness%20burn%5BTitle%2FAbstract%5D .
- 24.PubMed Search “Second Degree Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=second%20degree%20burn%5BTitle%2FAbstract%5D .
- 25.PubMed Search "Full Thickness Burn". 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=full%20thickness%20burn%5BTitle%2FAbstract%5D .
- 26.PubMed Search “Third Degree Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=third%20degree%20burn%5BTitle%2FAbstract%5D .
- 27.PubMed Search “Fourth Degree Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=fourth%20degree%20burn%5BTitle%2FAbstract%5D .
- 28.PubMed Search “Fifth Degree Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=fifth%20degree%20burn%5BTitle%2FAbstract%5D .
- 29.PubMed Search “Sixth Degree Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=sixth%20degree%20burn%5BTitle%2FAbstract%5D .
- 30.PubMed Search “Deep Partial Thickness Burn”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=deep%20partial%20thickness%20burn%5BTitle%2FAbstract%5D .
- 31.PubMed Search “Severe Burn Injury”. 2012. [Accessed Nov 1, 2012]. http://www.ncbi.nlm.nih.gov/pubmed?term=severe%20burn%20injury%5BTitle%2FAbstract%5D .
- 32.Kearns RD, Cairns CB, Holmes JH, Rich PB, Cairns BA. Thermal burn care: A review of best practices. What should prehospital providers do for these patients? EMS World. 2013;42:43–51. [PubMed] [Google Scholar]
- 33.Surgeons ACo: New Verification Site Visit Outcomes. Trauma Programs. 2013. [Accessed May 1, 2013]. http://www.facs.org/trauma/verifivisitoutcomes.html .
- 34.National Incident Management Systemt. 2008. [Accessed Dec 7, 2012]. http://www.fema.gov/pdf/emergency/nims/NIMS_core.pdf .
- 35.Typed Resource Definitions, Emergency Medical Services Resources. [Manual] Federal Emergency Management Agency DoHS; 2009; 21. [Accessed Mar 27 2009]. Available at: http://www.fema.gov/pdf/emergency/nims/508-3_emergency_medica_%20services_%20resources.pdf. 508-3. [Google Scholar]


