Abstract
Background:
Dystocia is one of the important causes of maternal morbidity and mortality in low-income countries. This study was aimed to determine the diagnostic accuracy of maternal anthropometric measurements as predictors for dystocia in nulliparous women.
Materials and Methods:
This prospective cohort study was conducted on 447 nulliparous women who referred to Omolbanin hospital. Several maternal anthropometric measurements such as height, transverse and vertical diameters of Michaelis sacral rhomboid area, foot length, head circumference, vertebral and lower limb length, symphysio-fundal height, and abdominal girth were taken in cervical dilatation ≤ 5 cm. Labor progression was controlled by a researcher blind to these measurements. After delivery, the accuracy of individual and combined measurements in prediction of dystocia was analyzed. Dystocia was defined as cesarean section and vacuum or forceps delivery for abnormal progress of labor (cervical dilatation less than 1 cm/h in the active phase for 2 h, and during the second stage, beyond 2 h or fetal head descend less than 1 cm/h).
Results:
Among the different anthropometric measurements, transverse diameter of the Michaelis sacral rhomboid area ≤9.6 cm, maternal height ≤ 155 cm, height to symphysio-fundal height ratio ≤4.7, lower limb length ≤78 cm, and head circumference to height ratio ≥ 35.05 with accuracy of 81.2%, 68.2%, 65.5%, 63.3%, and 61.5%, respectively, were better predictors. The best predictor was obtained by combination of maternal height ≤155 cm or the transverse diameter of the Michaelis sacral rhomboid area ≤9.6 cm and Johnson's formula estimated fetal weight ≥3255 g, with an accuracy of 90.5%, sensitivity of 70%, and specificity of 93.7%.
Conclusions:
Combination of other anthropometric measurements and estimated fetal weight with maternal height in comparison to maternal height alone leads to a better predictor for dystocia.
Keywords: Anthropometric measurements, cephalopelvic disproportion, dystocia, Iran
INTRODUCTION
Dystocia or abnormal progress of labor is the most common maternal problem and cause of burden in low-income countries.[1,2] It is estimated that 600,000 maternal deaths occur due to pregnancy and delivery disorders each year in the world,[3] of which 95% is reported from developing countries, and in 30% of the cases, the problem is cephalopelvic disproportion.[3,4]
MATERIALS AND METHODS
This is a case–control prospective double-blind study conducted on 447 nulliparous women referring to maternity ward of Omolbanin hospital in Mashhad with term gestational age (38-42 weeks), single tone pregnancy, and vertex presentation during Nov 2008-July 2009. The research project was approved by the ethical consideration committee of Mashhad University of Medical Sciences and an informed consent was taken from all the subjects. Sample size, after a pilot study with confidence level of 99% and optimum error of 1%, was determined by ratio estimation formula. The women with history of pelvis fracture, asymmetric pelvis, foot lameness, clearly pelvic contraction in clinical examination, BMI > 30 kg/m2, 18< age <35 years, severe anxiety and 2500< neonatal weight <4000 g, and CS due to other reasons except dystocia were left out of the study. Maternal anthropometric measurements included head circumference, foot length, vertebral and lower limb length, symphysio-fundal height, abdominal girth, maternal height, transverse and vertical diagonals of Michaelis sacral rhomboid area, and intertrochanteric diameter in labor cervical dilatation ≤5 cm (latent phase until the first stage of active phase), which were taken by a unique researcher. Mothers’ foot length was measured by a wooden ruler, head circumference as the distance between highest occipital peak and mid-forehead line, the length of vertebra as the distance between the first cervical vertebra and the end of sacrum bone, and the length of lower limbs was measured in the right side of the body as the distance between femoral trochanter and heel. Transverse diagonal of the Michaelis sacral rhomboid area (the distance between two notches in superior posterior iliac spines in two transversal ends of sacrum) and vertical diagonal of Michaelis sacral rhomboid area (the distance between the fifth lumbar and the last sacral vertebra) were measured. All measurements were made using a measuring tape, while the mothers were in a standing position [Figure 1]. Mothers’ height was measured in standing position, following the height measurement standards. The intertrochanteric diameter was measured by Breisky pelvimeter in standing position.
Figure 1.
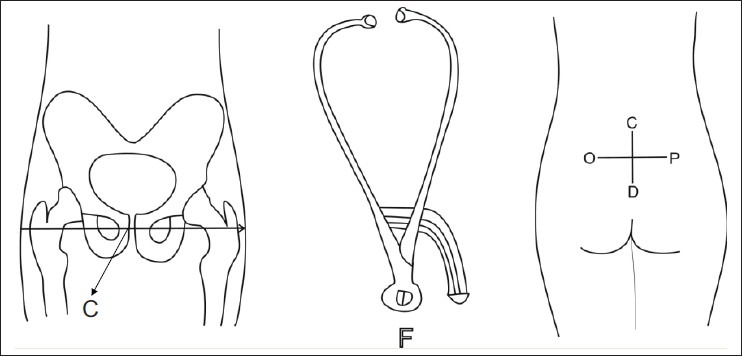
C, intertrochanteric; F, Breisky pelvimeter; OP, transverse diagonal of the Michaelis sacral rhomboid area; CD, vertical diagonal of the Michaelis sacral rhomboid area
Symphysio-fundal height was measured by a measuring tape after being sure of mothers’ bladder voiding and correction of mothers’ uterine deviation by measurement of the distance between superior edge of symphysis and uterine fundus and abdominal girth at the level of the umbilicus while in supine position. Maternal prepregnancy weight or that of the first trimester was collected based on recorded data in maternal prenatal files and BMI was calculated based on that. Data related to labor and delivery were collected through constant control of the patients during labor and delivery. Estimation of fetal weight was conducted by two methods. In Johnson's formula, the height of uterus was measured, and in case of fetal engagement, it was subtracted by 12 and multiplied by 155. In the other method, used in the present study, fetal weight was calculated by multiplication of uterine height by mothers’ abdominal circumference. In order to delete tool error and researcher's bias, all the subjects’ anthropometric measurements were repeated and their mean was considered as the final value. The data associated with these anthropometric measurements were not given to the researcher conducting labor control. Labor control was conducted by observing and recording cervical dilatation and fetal head descend every hour by the same researcher. For labor in the form of CS or vacuum, in addition to the existence of efficient contractions of the uterus, in the active stage of delivery, cervical dilatation <1 cm/h for two straight hours, and in the second stage of delivery, fetal head descend <1 cm/h, and/or when the length of this stage was more than 2 h,[18,19] it was considered as a criterion for dystocia. Number, severity, and length of uterus contractions were calculated by manual touch of uterine head. In the active stage of delivery (cervical dilatation ≥4 cm), existence of three to five contractions in 10 min lasting for ≥40 s, and when touching the fondues of uterus in a mid-severe contraction, if the researcher's hand fingers could not dent the abdominal muscle were considered as efficient uterine contractions. The subjects were divided into two groups of normal delivery and dystocia after delivery. Type of delivery was considered as a golden standard of pelvic capacity, and maternal anthropometric diagnostic value was calculated based on that. It should be noted that in selection of the cut-off points for anthropometric measurements, the obtained numerical value of these measurements was of great importance. With regard to the fact that precise detection of both healthy and diseased individuals is important, to prevent unnecessary referral of healthy individuals and/or not referral of unhealthy individuals, it was tried to consider the cases with the highest accuracy in addition to high level of sensitivity and specificity (>50%) as the cut-off points. So, sensitivity and specificity for percentiles and quarters of various anthropometric measurements in the study population were calculated, and in the second percentile, transverse diagonal of Michaelis sacral rhomboid area ≤9.6 cm was considered as its cut-off point. In the third percentile, maternal height ≤155 cm was considered as its cut-off point. In the fourth percentile, intertrochanteric diameter ≤31 cm; in the fourth percentile, ratio of height to fundal height ≤4.7; in the third percentile, lower limbs’ length ≤78 cm; in the sixth percentile, ratio of head circumference to height ≥35.05; in the first quarter, foot length ≤23 cm; in the second quarter, fetal estimated weight by Johnson's formula ≥3255 g; in the second quarter, fetal weight estimated by multiplication of uterine height by abdominal circumference ≥3255 g; in the sixth percentile, fundal height >33 cm; in the second quarter, mother's BMI >22 kg/m2; in the second quarter, vertebral length ≤58.5 cm; in the sixth percentile, abdominal circumference >98.6 cm; in the second quarter, head circumference >55 cm; in the second quarter, vertical diagonal of Michaelis sacral rhomboid area ≤9.5 cm; in the sixth percentile, lower limb length to height ratio ≤50.6; and in the s econd quarter, vertebral length to height ratio ≤36.8 were considered as the anthropometric measurement cut-off points. The data were analyzed by SPSS version 16. Comparison of mean anthropometric measurements in the two groups of normal delivery and dystocia was conducted by Mann–Whitney and Student's t-test. Various percentiles and quarters of height and pelvic diameters were calculated, and the sensitivity and specificity, positive and negative indicative values, and their accuracy were manually calculated.
RESULTS
In this research, 527 nulliparous women entered the study of whom 80 were excluded due to CS from any other cause except dystocia, such as meconium fetal amniotic fluid (n = 25), fetal distress (n = 16), fetal macrosomia (n = 4), abruption placenta (n = 2), severe vaginal bleeding (n = 3), brow presentation (n = 1), birth weight <2500 g (n = 1), no response of ineffective uterine contraction to oxytocin (n = 3), and severe pelvic contraction (n = 25). Finally, 447 had delivery, of whom 56 subjects (12.5%) had dystocia including 9 subjects (2%) with vacuum delivery and 47 subjects (10.5%) with CS. Total of 391 subjects (87.5%) had normal delivery. Mean mothers’ height (P = 0.002), the transverse diagonal of the Michaelis sacral rhomboid area (P = 0.000), lower limb length (P = 0.016), and height/symphysio-fundal height ratio (P = 0.001) were significantly less in dystocia group. Mean vertebral length was less in dystocia group, but not significant (P = 0.0691). Mean ratio of head circumference to height was significantly higher in dystocia group (P = 0.012), and mean symphysio-fundal height (P = 0.059), estimation of fetal weight through Johnson's method (P = 0.059), estimation of fetal weight by multiplication of symphysio-fundal height by abdominal girth (P = 0.072), and mean abdominal girth (P = 0.310) were higher in dystocia group, but not statistically significant. Mean vertical diagonal of the Michaelis sacral rhomboid area, intertrochanteric diameter, BMI, head circumference, foot length, vertebral length to height ratio, and lower limb length to height ratio were not significantly different in the two groups [Table 1].
Table 1.
Mean of maternal anthropometric measurements in the two groups, normal delivery and dystocia
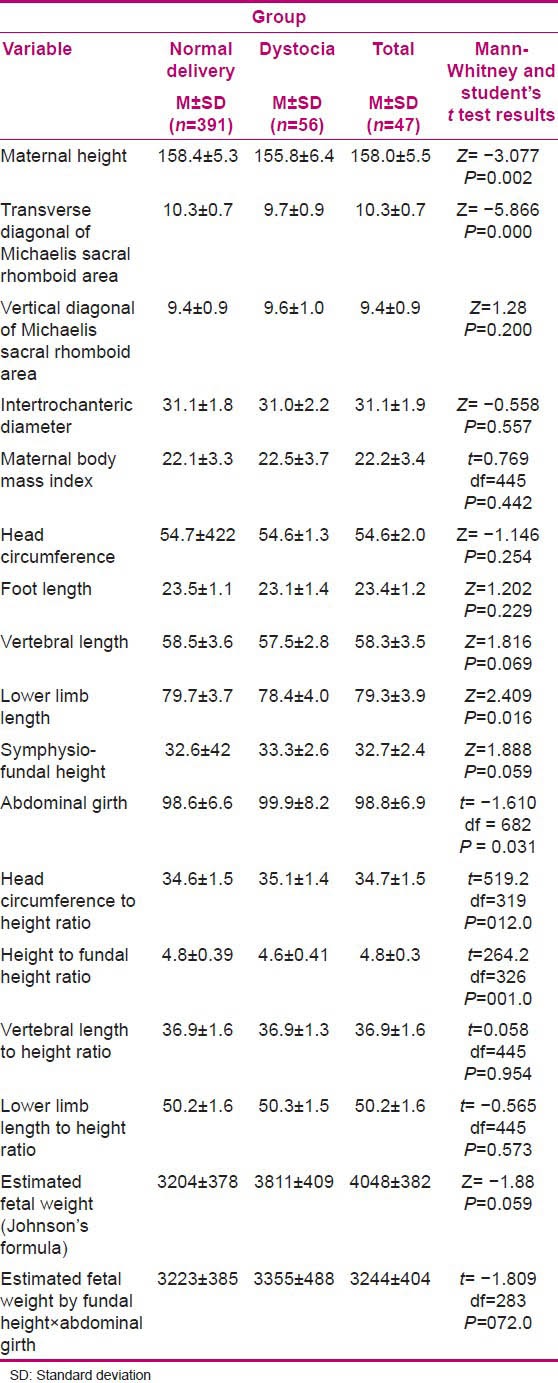
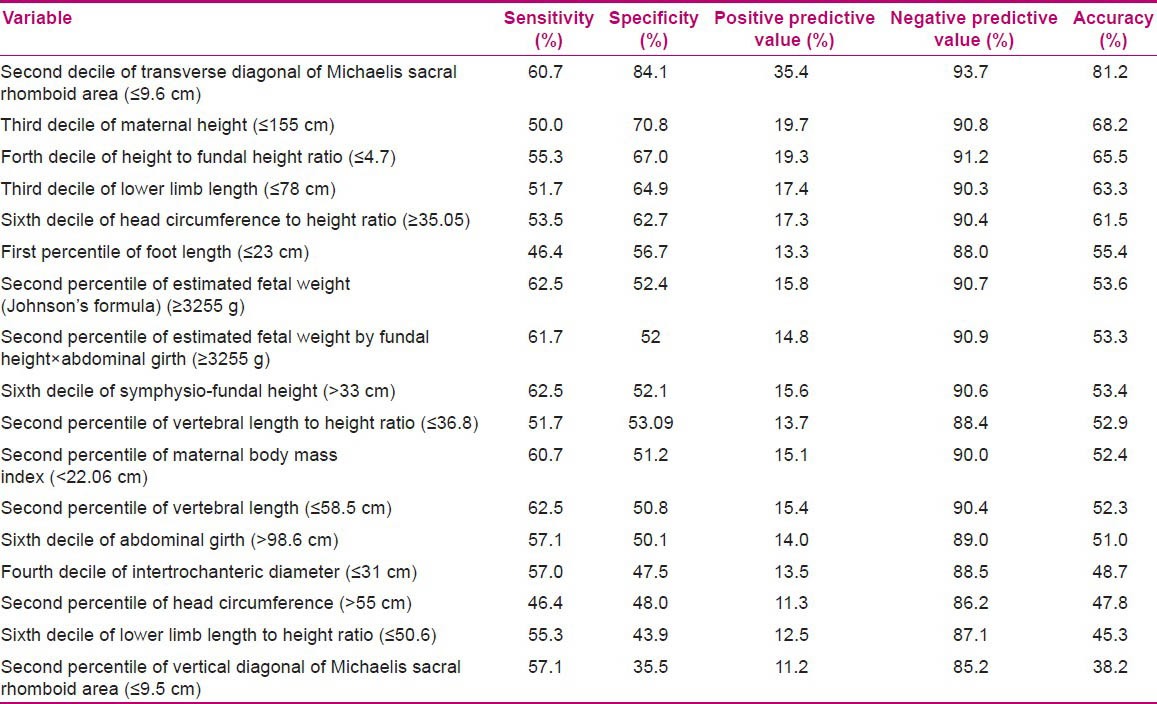
On evaluation of diagnostic values of height and each of the anthropometric measurements alone, the transverse diagonal of the Michaelis sacral rhomboid area with sensitivity of 60.7%, specificity of 84.1%, and accuracy of 81.2% had the highest diagnostic value. After that, mothers’ height with sensitivity of 50%, specificity of 70.8%, and accuracy of 68.2% was in the second rank. Ratio of height to fundal height with accuracy of 63.5%, lower limb length with accuracy of 63.3%, head circumference to height ratio with accuracy of 61.5%, and their respective diagnostic values were almost similar to that of mother's height. Other pelvic measurements presented lower diagnostic values [Table 2].
Table 2.
Diagnostic values of maternal anthropometric measurements for dystocia prediction
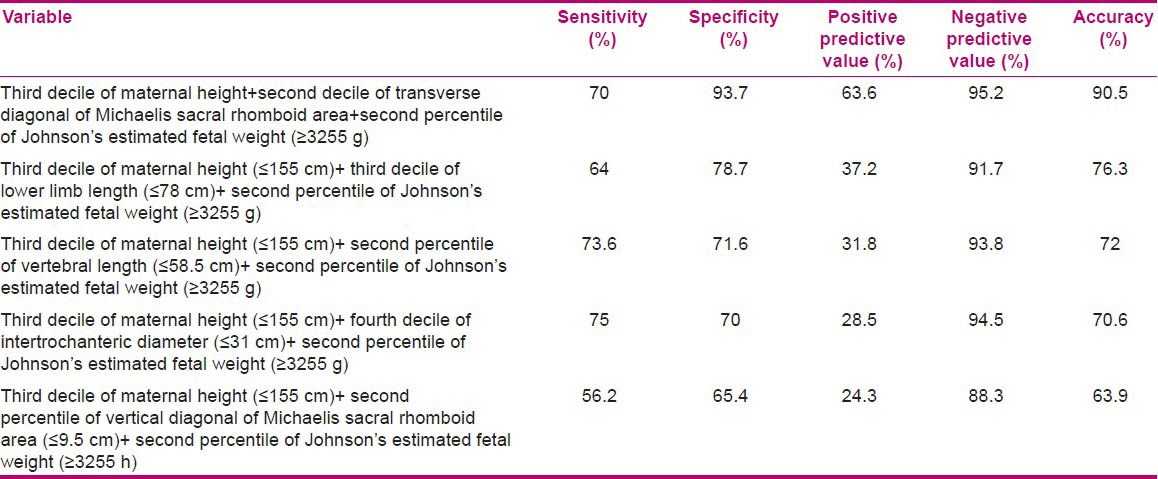
Combination of mothers’ height with most of the maternal anthropometric measurements in comparison with the diagnostic value obtained for height and each of the anthropometric measurements alone led to a better predictor of dystocia, of which combination of the third percentile of mothers’ height ≤155 cm with the second percentile of the transverse diagonal of the Michaelis sacral rhomboid area ≤9.6 cm with a sensitivity of 58.3%, specificity of 89.9%, and accuracy of 86.2% was the best predictor for dystocia. Combination of mothers’ height with uterine height >33 cm with an accuracy of 73.7%, combination of mothers’ height with estimation of fetal weight by Johnson's method with an accuracy of 73.3%, combination of mothers’ height with lower limb length with an accuracy of 71.5%, combination of mothers’ height with abdominal circumference with an accuracy of 71.5%, and combination of mothers’ height with foot length with an accuracy of 69.2%, in comparison with mothers’ height alone, led to a better predictor for dystocia. Combination of height with other anthropometric measurements in comparison with mothers’ height alone did not result in a better predictor [Table 3]. Combination of estimated fetal weight by Johnson's method with pair combination of height and other anthropometric measurements led to a better predictor for dystocia, and the highest diagnostic value obtained in the present study was for combination of the third percentile of mothers’ height with the second percentile of transverse sacral Michaelis diameter and the second quarter of fetal weight estimation through Johnson's formula with a sensitivity of 70%, specificity of 93.7%, and accuracy of 90.5% [Table 4].
Table 3.
Diagnostic values of combining of maternal height with other maternal anthropometric measurements
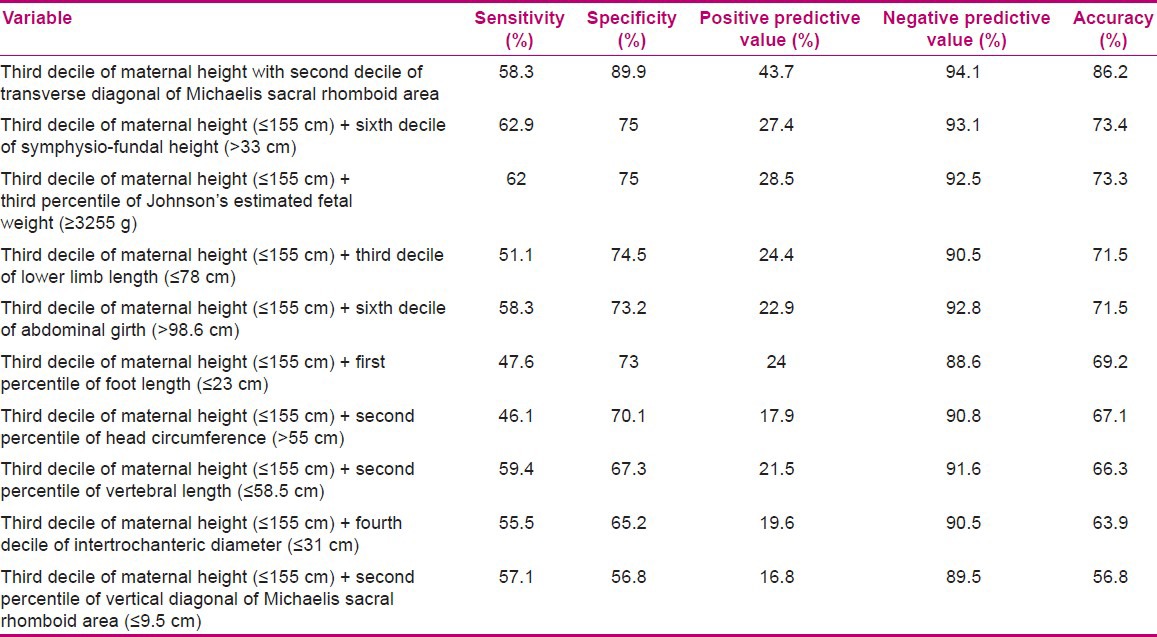
Table 4.
Diagnostic values of combining different deciles and percentiles of maternal height with pelvic diameters and pelvic diameters with each other by the highest validity
DISCUSSION
In the present study, with the goal of achieving better predictors for dystocia, in addition of height, we calculated the other maternal anthropometric measurements: mothers’ head circumference, head circumference to height ratio, lower limb length, lower limb to height ratio, vertebral length, vertebral length to height ratio, transverse and vertical diagonals of Michaelis sacral rhomboid area, intertrochanteric diameter, height to symphysio-fundal height ratio, and abdominal girth.
The accuracy obtained for mothers’ height ≤155 cm was 68.2%, with a sensitivity of 50% and specificity of 70.8%. Among the various maternal anthropometric measurements, the transverse diagonal of the Michaelis sacral rhomboid area ≤9.6 cm with an accuracy of 81.2%, sensitivity of 60.7%, and specificity of 84.1% was the best predictor for dystocia, and had a high accuracy, sensitivity, and specificity compared to mothers’ height. Height to symphysio-fundal height ratio ≤4.7, lower limb length ≤78 cm, maternal head circumference to height ≥35, fetal weight estimation ≥3255 g (Johnson's method), fetal weight estimation ≥3255 g by multiplication of symphysio-fundal height with abdominal girth, symphysio-fundal height >33 cm, mothers’ BMI >22 kg/m2, vertebral length ≤58.5 cm, abdominal girth >98.6 cm, intertrochanteric diameter ≤31 cm, and vertical diagonal of Michaelis sacral rhomboid area ≤9.5 cm had a higher sensitivity in the prediction of dystocia compared to mothers’ height, but their obtained specificity and accuracy were lower than those of mothers’ height. Mothers’ foot length ≤23 cm and head circumference >55 cm had lower sensitivity, specificity, and accuracy compared to mothers’ head. Few studies have compared the diagnostic value of maternal anthropometric measurements with height. In the study of Liselele et al., (2000)[3] the cut-off points of pelvic diameters were selected based on percentile 10 of their society, and their obtained sensitivity, specificity, and positive likelihood ratio for mothers’ height were 21.%, 93.8%, and 3.5, respectively. Transverse diagonal of Michaelis sacral rhomboid area with a sensitivity of 42.9%, specificity of 91.1%, and positive likelihood ratio of 4.8, and intertrochanteric diameter with a sensitivity of 38.1%, specificity of 89.4%, and positive likelihood ratio of 3.6 were better predictors for dystocia compared to mothers’ height.[3] In Rozenholc et al., (2007) report, mothers’ height with a sensitivity of 28.6%, specificity of 98.4%, and positivity likelihood ratio of 18.4 was the best predictor for dystocia and other maternal anthropometric measurements had lower diagnostic value. For transverse diagonal of Michaelis sacral rhomboid area, they found a sensitivity of 45.9%, specificity of 92.7%, and positivity likelihood ratio of 6.3. Although it had a higher sensitivity compared to mothers’ height, its specificity and positive likelihood ratio were lower, and the intertrochanteric diameter with a sensitivity of 26.5%, specificity of 88.9%, and positive likelihood ratio of 2.4 had lower diagnostic value compared to mothers’ height.[15] The calculated sensitivity for mothers’ height and transverse diagonal of Michaelis sacral rhomboid area in our study was more than the sensitivity obtained in the aforementioned studies and is not consistent with them, possibly due to different determined cut-off points in our study, which have been obtained based on the best sensitivity, specificity, and accuracy calculated by various percentiles and quarters. In our study, the diagnostic value of transverse diagonal of Michaelis sacral rhomboid area was higher than the diagnostic value of mothers’ height, which is consistent with the results of Liselele et al.[3]
Benjamin et al., (2011) determined the cut-off point of maternal anthropometric measurements based on Rock's curve, and calculated sensitivity, specificity, and positive predictive value for mothers’ height ≤155.5 cm as 70.4%, 52.1%, and 15.4%, respectively. They reported that mothers’ foot length ≤23 cm with a sensitivity of 77.8, specificity of 58.6%, and positive predictive value of 18.6% had a better prediction value compared to mothers’ height and transverse diagonal of Michaelis sacral rhomboid area ≤10.4 was not a better predictor for dystocia compared to mothers’ height,[20] which is not consistent with the present study. In the study of Rozenholc et al., (2007) and Benjamin et al., (2011) symphysio-fundal height, mothers’ foot length, vertical diagonal of Michaelis sacral rhomboid area ≤10.1, fetal weight estimation by Johnson's formula and abdominal girth had lower specificity compared to mothers’ height.[15,20] In the study of Van Bogaert et al. (1999), the mean lengths of lower limb in the groups of natural delivery and dystocia were 91.3 and 89.3 cm, respectively (P = 0.014), the mean lengths of vertebra in normal delivery and dystocia groups were 75.2 and 73.8 cm, respectively (P = 0.0003), and the mean mothers’ heights in normal delivery and dystocia groups were 157.6 and 154.1 cm, respectively (P = 0.0001).[21] In the study of Barnhard et al., (1997) the mean ratios of height to symphysio-fundal height in normal delivery and dystocia groups were 7 and 3.7, respectively (P = 0.02).[22] In the study of Connolly et al., (2003) the mean mothers’ head circumference values in normal delivery and dystocia groups were not significantly different, but the mean ratios of head circumference to height in normal delivery and dystocia groups were 34 and 35.1, respectively (P = 0.001).[23] Their results are in line with ours. Some researchers have argued that an increase in the ratio of head circumference to height in animals is a risk factor for dystocia. They reasoned that the women with high ratio of head circumference to height possibly have faced a growth disorder in their fetal period, leading to an imbalance in their ratio of head circumference to height, and consequently, this growth disorder may have affected their pelvis size.[23] The ratio of lower limb to height is an important predictor for nutrition and health status of individuals, so women with malnutrition face shortness of vertebra and acute shortness in their lower limb as well as a reduction in the ratio of lower limb to height.[24] Malnutrition in childhood is an important risk factor for bones’ growth and shortness, which can be associated with growth disorder of pelvic bones.[17]
Adolf Michael suggested the importance of Michaelis sacral rhomboid area in the evaluation of pelvic capacity for the first time in 1851.[25] Abnormal size of Michaelis sacral rhomboid area is a predictor for mothers’ shape and abnormal pelvic size,[25,26] and in pelvises with stenosis, its transverse diameter is shorter than its vertical diameter.[26] The distance between femoral great trochanters is associated with transverse pelvic diameter and in a number of studies has been reported to have a better diagnostic value compared to mothers’ height.[3] Fetal size is estimated through different measurement methods such as measurement of symphysio-fundal height, abdominal girth, calculation of fetal weight by Johnson's formula, and multiplication of symphysio-fundal height with abdominal girth. Fetal size alone is not counted as an appropriate criterion for an unsuccessful delivery, as in most of the cases, cephalopelvic disproportion is observed among the fetuses with their weight in a normal range.[19] Therefore, evaluation of the imbalance of fetal size with mothers’ pelvis can be a better criterion to predict dystocia compared to fetal weight alone.[27] These results are in accordance with those of the present study which showed the ratio of height to symphysio-fundal height was a better predictor for dystocia compared to symphysio-fundal height alone. In the present study, combination of mothers’ height with different anthropometric measurements led to better predictors for dystocia compared to mothers’ height alone. Combination of mothers’ height ≤155 cm with transverse diagonal of Michaelis sacral rhomboid area ≤9.6 cm with an accuracy of 86.2%, sensitivity of 58.3%, and specificity of 89.9% yielded the best predictor. After this, combination of cut-off points of mothers’ height with symphysio-fundal height >33 cm, mothers’ height with fetal weight ≥3255 g by Johnson's formula, mothers’ height with lower limb length ≤78 cm, and mothers’ height with abdominal girth >98.6 cm were better predictors concerning sensitivity, specificity, and accuracy, respectively. In Rozenholc et al., (2007) and Liselele et al., (2003) study, combination of mothers’ height with transverse diagonal of Michaelis sacral diameter, intertrochanteric diameter, mothers’ foot length, and symphysio-fundal height resulted in better predictors concerning sensitivity and specificity.[3,15]
Benjamin et al., (2011) suggested combination of mothers’ height with fetal weight estimation by Johnson's formula and measurement of mothers’ foot length as better predictors compared to mothers’ height alone.[20]
In the present study, maternal anthropometric measurements in addition to height and fetal weight estimation by Johnson's formula were combined, and among the triple combinations, the highest accuracy (90.5%) was for combination of mothers’ height, transverse diagonal of Michaelis sacral rhomboid area, and estimated fetal weight by Johnson's formula, with a sensitivity of 70% and specificity of 93.7%, which was better than the combination of height and transverse diagonal of Michaelis sacral rhomboid area concerning specificity and accuracy. Triple combination of fetal estimated weight with height and lower limb length with a sensitivity of 64%, specificity of 78.7%, and accuracy of 76.3%, triple combination of fetal estimated weight with height and vertebral length with a sensitivity of 73.6%, specificity of 71.6%, and accuracy of 72%, and triple combination of fetal estimated weight with height and intertrochanteric diameter with a sensitivity of 75%, specificity of 70%, and accuracy of 70.6% resulted in better predictors concerning sensitivity, specificity, and accuracy, compared to each of the paired combinations.
Our results are consistent with those of Benjamin et al., (2011).[20] In the investigation of diagnostic value of each maternal anthropometric measurement, the accuracy obtained for mothers’ height was 68.3. Except for transverse diagonal of Michaelis sacral rhomboid area, other anthropometric measurements had lower diagnostic values compared to mothers’ height. Combination of mothers’ height with the other anthropometric measurements led to better predictors compared to mothers’ height alone. The best predictor was pair combination of mothers’ transverse diagonal of Michaelis sacral rhomboid area and height with a sensitivity of 58.3%, specificity of 89.9%, and accuracy of 86.2. Combinations of mothers’ height with symphysio-fundal height (accuracy = 73.4%), lower limb length (accuracy = 71.5%), and abdominal girth (accuracy = 71.5%) were the best predictors compared to mothers’ height alone.
In the present study, the best predictors concerning sensitivity, specificity, and accuracy were obtained by triple combination of maternal anthropometric measurements and height with fetal weight estimation by Johnson's method, and the best predictor was related to combination of third percentile of mothers’ height (≤155 cm), the second percentile of transverse diagonal of Michaelis sacral rhomboid area (≤9.6 cm), and fetal estimated weight (≥3255 g) by Johnson's method, which had accuracy of 90.5%, sensitivity of 70%, and specificity of 93.7%.
CONCLUSION
Based on the results of the present study, mothers’ height alone is not an appropriate predictor for dystocia, and its combination with other maternal anthropometric measurements and estimation of fetal weight yields better predictors to predict dystocia.
ACKNOWLEDGMENTS
The present study is a part of MS dissertation approved and sponsored by Mashhad University of Medical Sciences with project number 87325. We greatly appreciate the kind cooperation of Vice-chancellery for research in the university.
Footnotes
Source of Support: This work was supported by Mashhad University of Medical Sciences Vice-presidency for research
Conflict of Interest: Nil.
REFERENCES
- 1.Hofmery G. Obstructed labour: Using better technologies to reduce mortality. Int J Gynaecol Obstet. 2004;1:S62–72. doi: 10.1016/j.ijgo.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Surapanthapisit P, Thitadilok W. Risk factors of caesarean section due to cephalopelvic disproportion. J Med Assoc Thai. 2006;89:S105–11. [PubMed] [Google Scholar]
- 3.Liselele HB, Tshibangu CK, Meuris S. Association between External Pelvimetry and Vertex Delivery Complications in African Women. Acta Obstet Gynecol Scand. 2000;79:673–8. [PubMed] [Google Scholar]
- 4.Gregory KD, Niebyl JR, Johnson TR. Preconception and prenatal care: Part of the continuum. In: Gabbe SG, editor. Gbbe: Obstetrics Normal and Problem Pregnancies. 5th ed. New York: Churchill Livingstone Publishers; 2008. p. 102. [Google Scholar]
- 5.Neilson JP, Lavender T, Quenby S, Wray S. Obstructed labor. Br Med Bull. 2003;67:191–204. doi: 10.1093/bmb/ldg018. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Prolonged obstructed labourc. 2000. [Last accessed on 2007 Nov 21]. Available from: http://www.helid.digicollection.org/es/d/Jwho36e/7.4.6.html .
- 7.Zhu BP, Grigorescu V, Le T, Lin M, Copeland G, Barone M, et al. Labor Dystocia and its Association with Inter pregnancy Interval. Am J Obstet Gynecol. 2006;195:121–8. doi: 10.1016/j.ajog.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 8.Dujardin B, Van Cutsem R, Lambrechts T. The value of maternal height as a risk factor of dystocia: A meta- analysis. Trop Med Int Health. 1996;1:510–21. doi: 10.1046/j.1365-3156.1996.d01-83.x. [DOI] [PubMed] [Google Scholar]
- 9.Kwawukume EY, Ghosh TS, Wilson JB. Maternal height as a predictor of vaginal delivery. Int J Gynecol Obstet. 1993;41:27–30. doi: 10.1016/0020-7292(93)90150-u. [DOI] [PubMed] [Google Scholar]
- 10.Khunpradit S, Patumanond J, Tawinchasri CH. Validation of risk scoring scheme for cesarean delivery due to cephalopelvic disproportion in Lamphum Hospital. J Med Assoc Thai. 2006;89:s163–8. [PubMed] [Google Scholar]
- 11.Mahmood TA, Campbell DM, Wilson AW. Maternal height shoe size, and outcome of labor in white primigravidas: A prospective anthropometric study. Br Med J. 1988;297:20–7. doi: 10.1136/bmj.297.6647.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaretsky MV, Alexander JM, Menintire DD, Hatab MR, Leveno KJ. Magnetic resonance imagining pelvimetry and the prediction of labor dystocia. Obstet Gynecol. 2005;106:919–26. doi: 10.1097/01.AOG.0000182575.81843.e7. [DOI] [PubMed] [Google Scholar]
- 13.Sule ST, Matawal BI. Antenatal clinical pelvimetry in primigravidate and outcome of labour. Ann Afr Med. 2005;4:164–8. [Google Scholar]
- 14.Sonal B, Shalini R, Chandra SK, Neerga G. Ultrasonic obstetric conjugate measurement: A practical pelvimetric tool. J Obstet Gynecol India. 2006;56:212–5. [Google Scholar]
- 15.Rozenholc AT, Ako SN, Leke RJ, Boulvain M. The diagnostic accuracy of external pelvimetry and maternal height to predict dystocia in nulliparous women: A study in cameroon. BJOG. 2007;114:630–5. doi: 10.1111/j.1471-0528.2007.01294.x. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal N, Guleria K, Bansal S. Sacral rhomboid dimension: A new effective screening parameter for cephalopelvic disproportion. Int J Gynaecol Obstet. 2003;210:210. [Google Scholar]
- 17.Konje JC, Ladipo OA. Nutrition and Obstructed Labor. Am J Clin Nutr. 2000;72:s291–7. doi: 10.1093/ajcn/72.1.291S. [DOI] [PubMed] [Google Scholar]
- 18.Dudeley DJ. Complications of labor. In: Scott JR, editor. Danforth's obstetrics and gynecology. 10th ed. Philadelphia: Lippincott Williams and Wilkins Publisher; 2003. pp. 219–29. [Google Scholar]
- 19.Cunningham G, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Sponge CY. Abnormal labour. In: Cunningham G, editor. Williams Obstetrics. 23rd ed. New York: MC Graw Hill publishers; 2010. p. 131. [Google Scholar]
- 20.Benjamin SJ, Daniel AB, Kamath A, Ramkumar V. Anthropometric measurements as predictors of cephalopelvic disproportion: Can the diagnostic accuracy be improved.? Acta Obstet Gynecol Scand. 2011;91:122–7. doi: 10.1111/j.1600-0412.2011.01267.x. [DOI] [PubMed] [Google Scholar]
- 21.Van Bogaert LJ. The Relation Between Height, Foot Length, Pelvic Adequacy and Mode of Delivery. Eur J Obstet Gynecol Reprod Biol. 1999;82:195–9. doi: 10.1016/s0301-2115(98)00232-2. [DOI] [PubMed] [Google Scholar]
- 22.Barenhard YB, Divon MY, Pollack RN. Efficacy of the maternal height to fundal height ratio in predicting arrest of labor disorder. J Matern Fetal Med. 1997;6:103–7. doi: 10.1002/(SICI)1520-6661(199703/04)6:2<103::AID-MFM8>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 23.Connolly G, Naidoo C, Conroy RM, Byrne P, McJenna P. A new predictor of cephalopelvic disproportion? J Obstet Gynaecol. 2003;23:27–9. doi: 10.1080/0144361021000043173. [DOI] [PubMed] [Google Scholar]
- 24.Bogin B, Varela-Silva MI. Leg length, body proportion, and health: A review with a note on beauty. Int J Environ Res Public Healyh. 2010;7:1047–75. doi: 10.3390/ijerph7031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michael J, O’dowd, Philip E. The history of obstetrics and gynaecology: Informa Health Care. c2000. [Last accessed on 2007 May 10]. Available from: http://www.amazon.com/History-Obstetrics-Gynaecology-M-J-ODowd/dp/1850700400 .
- 26.Schunk M, Schulte E. Surface anatomy of the body, landmarks and reference lines. In: Schunk M, editor. Thiems atlas of anatomy: General anatomy and musculoskeletal system. 1st ed. New York: Theime Publisher; 2006. pp. 24–32. [Google Scholar]
- 27.Ferguson JE, 2nd, Newberry YG, Deangelis GA, Finnerty JJ, Agarwal S, Turkheimer E. The fetal-pelvic index has minimal utility in predicting fetal-pelvic disproportion. Am J Obstet Gynecol. 1998;179:1186–92. doi: 10.1016/s0002-9378(98)70129-2. [DOI] [PubMed] [Google Scholar]


