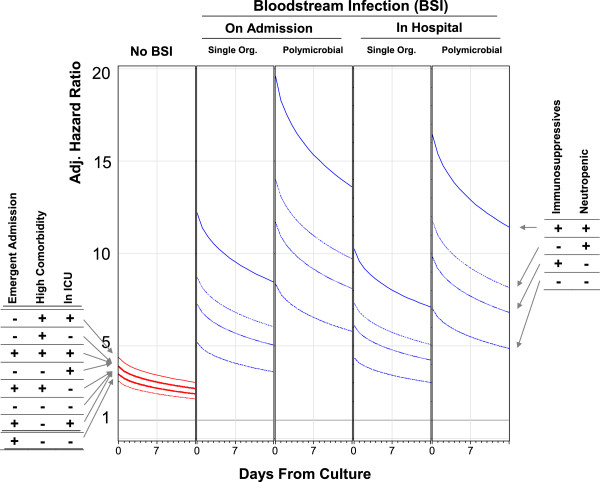
Figure 3.
Adjusted influence of negative blood cultures/bloodstream infection on hospital mortality by significant effect modifiers. These plots present the adjusted hazard ratio (vertical axes) for the association of negative blood cultures (“No BSI”) and bloodstream infection with death in hospital in the first 2 weeks following blood culture testing (horizontal axes). Adjusted hazard ratios for negative blood cultures are presented for all combinations of admission urgency (elective vs. emergent), patient comorbidity status (low comorbidity [Elixhauser score of 1] vs. high comorbidity [Elixhauser score of 12]), and intensive care unit (ICU) status. Adjusted hazard ratios for bloodstream infection (calculated for patients with low comorbidity, low comorbidity, and not in the ICU) are presented for all combinations of immunosuppressant exposure and neutropenia. All hazard ratios adjust for: patient age; patient sex; admission service (i.e. medical or surgical) and diagnosis; severity of acute illness as measured by the Laboratory-based Acute Physiology Score (LAPS); chronic comorbidities as measured by the Elixhauser score [20]; treatment in the intensive care unit; performance of significant operative procedures [23]; awaiting long-term care status; [19] and exposure to immunosuppressant medications. All adjusted hazard ratios use as a comparator a person an electively admitted person with low comorbidity not in the ICU who has no blood culture measured.