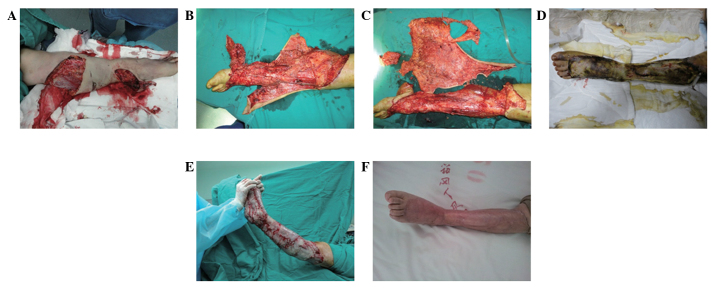
Figure 2.
Case 2: Female, aged 45, admitted to hospital 4 h after a motor vehicle accident. Diagnosis: i) Avulsion of the left lower extremity; ii) fracture of the left tibia; and iii) hemorrhagic shock. (A and B) The skin and subcutaneous soft tissue below the left knee were stripped off and separated from the deep fascia. (C) The wound bed tissue became swollen following debridement. Furthermore, physiological structures and the normal tissues were mixed. Therefore, the success rate of skin grafting was likely to be relatively low. (D) A large sheet of XADM was used to cover the wound and several holes were opened in it for drainage. (E) The wound bed preparation was completed following 10 days of debridement. An autologous skin graft was subsequently performed for wound closure. (F) The follow-up was conducted one year following the surgery. Good recovery of the shape and function of the limb was exhibited. XADM, xenograft (porcine) acellular dermal matrix.