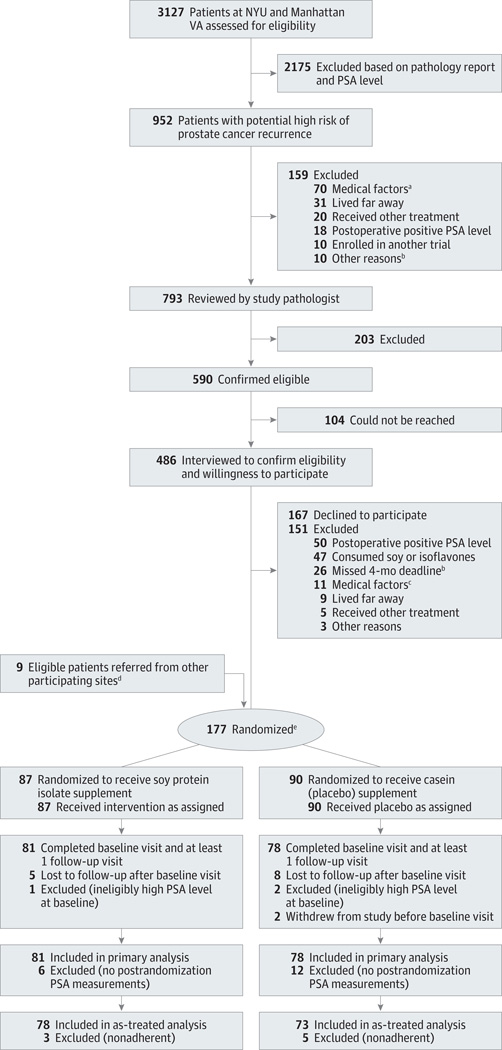
Figure 1. Participant Flow.
NYU indicates New York University; PSA, prostate-specific antigen.
aExclusionary medical factors included recent or current history of anemia, iron deficiency problems or subclinical iron deficiency at baseline, diabetes or insulin resistance requiring use of medication, thyroid disease, significant renal impairment, need for a sodium-restricted diet, substantive tendency to be constipated (grade ≥2 experienced regularly), a medical problem precluding the consumption of soy or casein such as allergies to soy or milk protein, and postoperative PSA of 0.07 ng/mL or higher. Fifty-four patients had diabetes, 8 had thyroid disease, 4 had anemia or low iron status, 2 had other malignancies, 1 had renal disease, and 1 had mental disease.
bThe 4-month postsurgery deadline had passed for these patients before pathology review could occur.
cPreviously undetected exclusionary medical factors included 4 patients who had diabetes, 1 who had thyroid disease, 1 who had anemia, 2 who had protein allergies, 1 who had recurrent constipation, 1 who had a restricted diet, and 1 who had mental disease.
dEight eligible participants were referred to the study by participating clinical sites other than NYU and the Manhattan VA; 1 eligible participant was referred to the study by a urologist in private practice. All 9 participants were confirmed to be at high risk by pathology review.
eThe median time between surgery and randomization was identical in both groups (14 weeks; 95% CI, 13.1–14.1; range, 7 or 8 to 18 weeks).