Abstract
High fruit and vegetable consumption is associated with a lower risk of breast cancer. The incidence of breast cancer is continuously increasing in Korea, but only a few studies on nutrition intervention in breast cancer patients has been reported. The aim of this study was to investigate whether an 8-week nutrition intervention based on dietary counseling can promote fruit and vegetable consumption, increase serum antioxidant nutrient levels, and improve quality of life in Korean breast cancer patients. Sixty-one breast cancer patients received either standard care (n = 31) or nutrition counseling (n = 30). The standard care group was given brochures recommending phytochemical rich diet. The intervention group was provided with two nutrition counseling sessions and one cooking class session, thereby encouraged subjects to eat at least 10 or more servings of fruits and vegetables per day. After 8-week intervention, waist circumference in the intervention group was significantly decreased (p < 0.001) even though no difference was reported for body mass index. Energy intake (p = 0.007), fiber (p < 0.001), and antioxidant nutrient (vitamin A, C, E, and β-carotene, p < 0.001, respectively) intakes were significantly increased. Serum antioxidant level was also increased significantly, i.e., vitamin A (p = 0.048); vitamin E (p = 0.004). Total vegetable intake (excluding kimchi intake) in the intervention group was increased from 425 g to 761 g (p < 0.001), fruit consumption was also increased from 232 g to 334 g (p < 0.001), while standard care group did not show any significant change. Our study showed that nutrition counseling and providing cooking tips helped to encourage the patient to consume and maintain more fruit and vegetable intakes.
Keywords: Counseling, Breast neoplasms, Fruits, Vegetables, Antioxidants
Introduction
Although breast cancer is still less prevalent in Korea than in western countries, the incidence of breast cancer, especially in the younger women, is increasing. In 2008, breast cancer was reported as one of the most common forms of cancer being treated in women [1,2]. Possible explanations for these increases are the change to a westernized diet, such as the high consumption of fat and less physical activity, together with early detection [3,4].
High in fruit and vegetable diet has been suggested to be associated with decreased breast cancer [5-7], although not consistently [8-10]. It is generally assumed that the active dietary constituents contributing to these protective effects are antioxidant nutrients such as vitamin A and vitamin E including phytochemicals. Although reasonable evidences proved that they are not enough in the treatment of breast cancer, but those antioxidant compounds, especially consumed as whole food, have been shown to neutralize free radicals, and reduce or even prevent some of the damages caused by free radicals [11,12].
Previous studies reported from the U.S. have demonstrated that intervention programs for breast cancer patients improve breast cancer prognosis and promote positive dietary behaviors [13-15]. The results of Women's Intervention Nutrition Study (WINS), which was an intensive dietary intervention designed to reduce dietary fat intake in postmenopausal women with early stage breast cancer, indicated that those in the intervention group showed reduction of the incidence of breast cancer recurrence and increase of relapse-free survival [13]. The Women's Healthy Eating and Living (WHEL) study also showed that an intensive one-on-one intervention delivered over the telephone had positive effects, in that it led to increased fruit, vegetable and fiber intakes, as well as reduced fat intake [14,15]. Taken together, these studies suggested that intervention program successfully accomplished and maintained a good health status during and after breast cancer treatment.
Some studies have shown that diet quality is associated with quality of life (QOL) [16-18]. It is unclear whether diet influences QOL or reflects it. However, if diet does influence QOL, nutrition intervention programs to improve overall diet quality in breast cancer patients could help to increase QOL.
Dietary intake differs significantly across the countries. Korean, especially, shows relatively high carbohydrate and low dietary fat consumption [19]. It is, therefore, very important to adjust the dietary modification according to their original dietary pattern. Do et al. [20]. showed that the dietary habit and nutrient intakes of postoperative breast cancer patients can be improved by individual nutrition counseling program. In that sense, however, the net effects of nutrition counseling intervention programs (increasing fruit and vegetable intake without much modification of fat intake) for reducing breast cancer recurrence and mortality have not enough investigated in Korea until now.
We hypothesized that breast cancer patients assigned to the dietary intervention group will show greater improvements in fruit and vegetable consumption, which would increase serum antioxidant levels than those of patients assigned to a standard care group. We also hypothesized that the dietary intervention group would show more favorable improvements in QOL than in the control group. In view of this, the aims of this study were: (1) to implement an 8-week intensive nutrition intervention to increase fruit and vegetable intake and (2) to evaluate changes in dietary intake, serum antioxidant level, and QOL after intervention.
Materials and Methods
Subjects and Study design
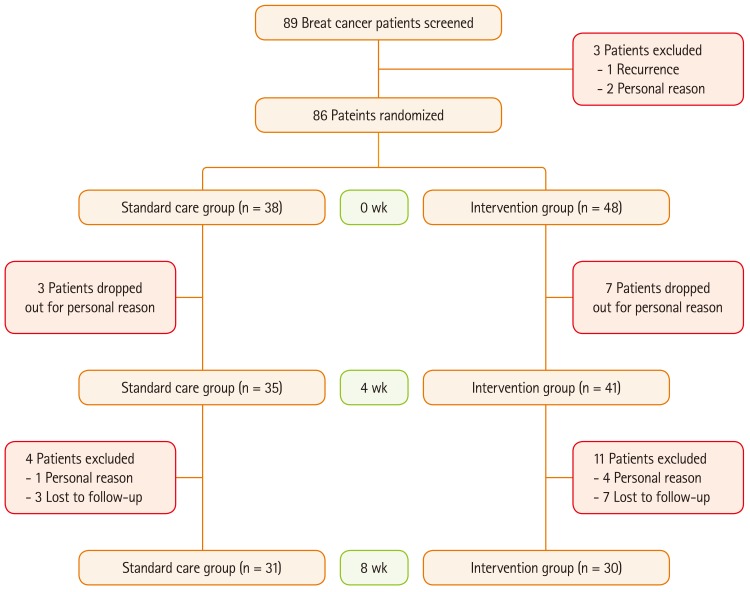
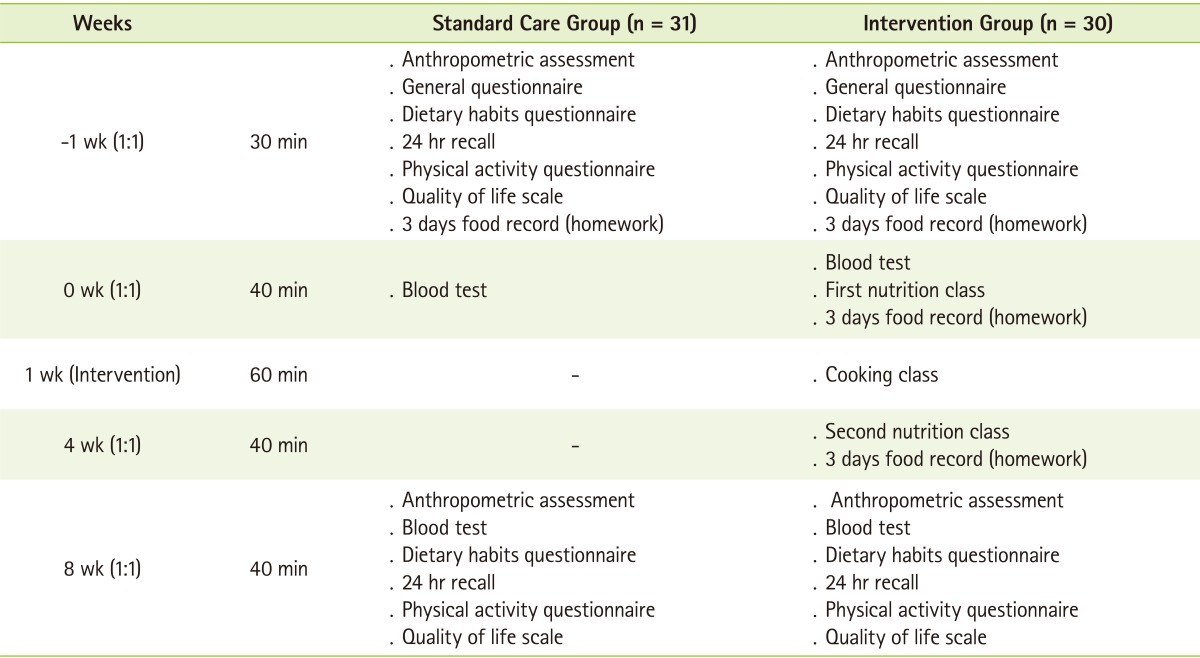
Between February 2009 and October 2009, a randomized dietary intervention study was carried out with breast cancer patients aged 25-65 year who had completed cancer treatment for stage I to III. The research protocol was approved by the Institutional Review Board of the S Hospital (Seoul, Korea), and all subjects provided written informed consent before participation. Subjects were also excluded if they present uncontrolled disease or women with body mass index (BMI) ≥25 kg/m2. Figure 1 shows a flow chart of this study. Breast cancer patients were randomly assigned to the standard care group (n = 38) or the intervention group (n = 48). The standard care group received no treatment but only received a brochure of general dietary guideline, and the intervention group received individualized dietary modification counseling with a professional dietitian (Table 1). Seven subjects in the standard care group and 18 subjects in the intervention group were excluded due to personal reason or lost to follow-up. Overall, 61 breast cancer patients (standard care group: n = 31, intervention group: n = 30) were included in the final analyses. Information regarding the general characteristics of the subjects, including age, medical history, and menopausal status, were collected by self-reported questionnaires.
Figure 1.
Flowchart of the study.
Table 1.
Study protocol
Measurements
Anthropometric measurements of subjects were conducted by a trained staff. Subjects were asked to remove their shoes and heavy outer garments before being weighed. The BMI was calculated as the body weight (kg)/height squared (m2), and waist circumference was measured to the nearest 0.1 cm, at the middle of the space between the lowest rib and the iliac crest, with subjects in standing position and after breathing out gently.
Blood samples (20 mL) were collected from each subject after overnight fasting for more than 8 hour, which were centrifuged for 15 minutes at 3,000 rpm and stored at -80℃ until analyzed. All the biochemical measurements were performed in the laboratory of the S Hospital. Serum antioxidant nutrient (carotene, vitamin A and vitamin E) were measured by using HPLC method [21].
Dietary intake was determined from diet records for 3 consecutive days (2 weekdays, 1 weekend day). The subjects were instructed to record all foods, beverages and supplements consumed, including detailed descriptions of foods, preparation methods and recipes. All the food items eaten, how they were cooked, and the amounts consumed were confirmed by the professional dietitian using food models and measuring tools. Nutrient intake was analyzed with the computer aided nutritional analysis program (CAN-pro 3.0, The Korean Nutrition Society, Seoul, Korea).
QOL was assessed with the Functional Assessment of Cancer Therapy (FACT-B) designed to measure multidimensional health-related quality of life in patients with breast cancer [22]. FACT-B comprises of five subscales: physical well-being (7 items), social well-being (7 items), emotional well-being (6 items), functional well-being (7 items), and concerns specific to patients with breast cancer (10 items). Each item is rated on a 5-point scale with 0 equal to "not at all" and 5 equal to "very much". Higher subscale score indicates higher well-being or satisfaction. All ratings on the FACT-B are completed in terms of the past seven days.
Intervention
The 8-week intervention program consisted of two nutrition counseling sessions of 40 minutes and one cooking class session with a professional dietitian. The counseling sessions focused on individualized dietary counseling to induce the subjects to concentrate on modifying or changing their eating habits. Intervention participants were encouraged to achieve the following advices but attainable goals chosen to promote a dietary pattern that maximizes intake of protective nutrients (antioxidant vitamins and fiber) and phytochemicals. The cooking class session and health-related materials (e.g. pamphlets and brochures) supported this individualized counseling. The cooking class focused on healthy food to promote adherence and understanding of the intervention dietary pattern, and gave patients an opportunity to learn how to prepare recipes to incorporate more fruit and vegetable.
Statistical analyses
Statistical analyses were conducted using the SPSS program (SPSS 15.0 KO for Windows; SPSS Inc., Chicago, USA). All values are expressed as the mean ± standard deviation or number (%).Differences between the two groups were analyzed by an independent Student's t-test or chi-square test. Paired t-tests were used to compare the changes in anthropometrics, dietary intakes, serum antioxidant levels, and quality of life scores between baseline and after intervention values. All reported p values were two-tailed, and the statistical significance was set at p < 0.05.
Results
General characteristics of the subjects
The baseline characteristics of the subjects are presented in Table 2, which shows that neither group differed in any baseline category. The number of subjects who were cooking herself was 27 (87.1%) in the standard care group and 26 (86.7%) in the intervention group. The majority had no family history of breast cancer, and was post-menopausal. Several types of exercise were performed; walking and hiking were the most common type of exercise, whereas stretching and swimming were also reported (data not shown).
Table 2.
Baseline characteristics of the subjects
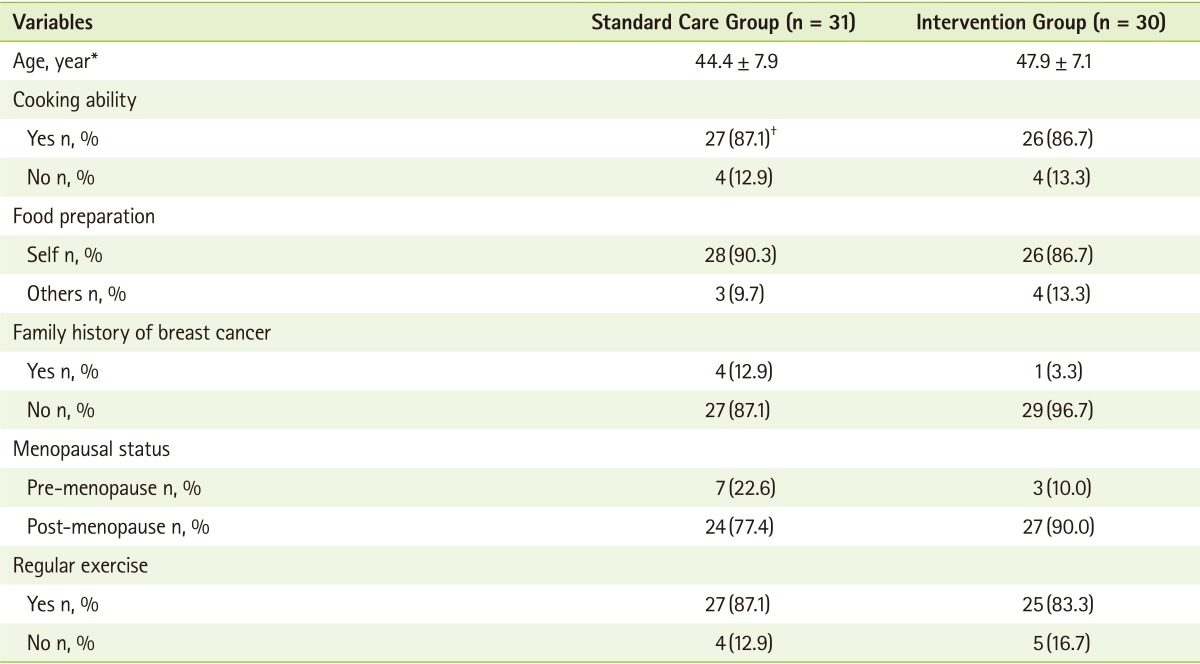
*Values are means ± SD or n, %; †Chi-Square Test shows no statistical significance.
Changes in anthropometrics parameters, dietary intake, serum antioxidant levels
Changes in anthropometrics parameters after the 8-week-nutrition intervention are presented in Table 3. There were no significant differences in the baseline weight, BMI, and waist circumference between the standard care group and the intervention group. After nutrition intervention, waist circumference in the intervention group was significantly decreased (p < 0.001) even though BMI remained unchanged. For the standard care group, in contrast, all of the anthropometric-measurements did not show any significant changes.
Table 3.
Changes in anthropometrics parameters after intervention
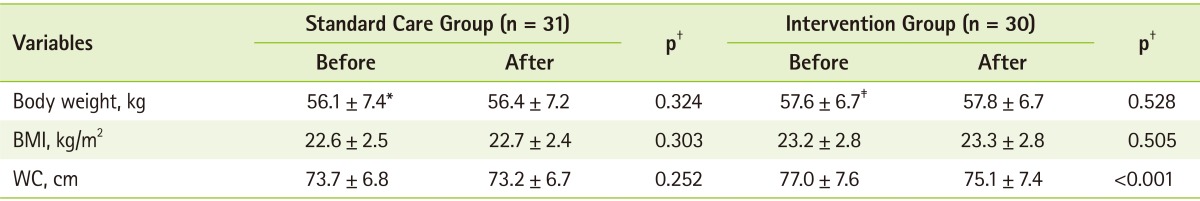
BMI: body mass index, WC: waist circumference.
*Values are means ± SD (all such values); †Measured by paired t-test between baseline and 8 week within each group at p < 0.05; ‡Baseline level between standard care group and intervention group showed no statistical significance after independent t-test.
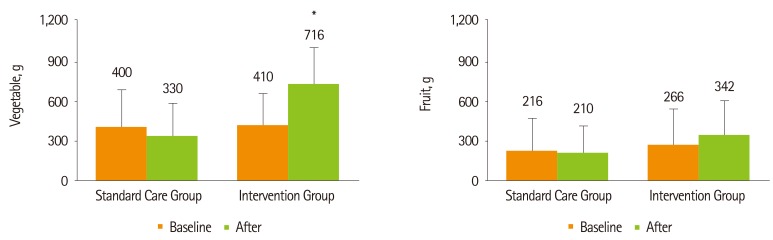
The average daily intakes of nutrients are presented in Table 4. After nutrition intervention, in the intervention group, there was a significant increase in the daily intake of energy (p = 0.009), plant protein (p < 0.001), carbohydrate (p = 0.011), fiber (p < 0.001), vitamin A (p < 0.001), vitamin C (p < 0.001), vitamin E (p < 0.001), folate (p < 0.001), and β-carotene (p < 0.001). Whereas, in the standard care group, there was a significant reduction in the daily intake of fiber (p = 0.027), vitamin A (p < 0.001), and folate (p = 0.029). Daily fruit and vegetable intake are shown in Figure 2. The intervention group increased their consumption of fruit from 266.0 to 341.5 g/d, vegetable consumption was also markedly increased from 410.0 to 716.0 g/d (p < 0.001), whereas standard care group did not show any changes in fruit and vegetable intake.
Table 4.
Changes in nutrient intakes after intervention
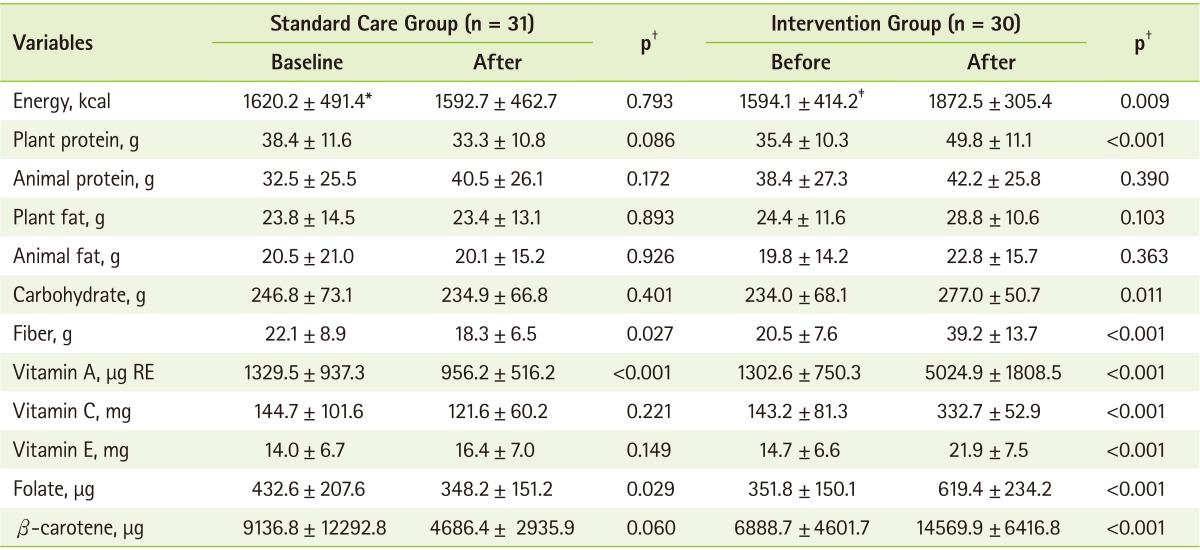
*Values are means ± SD (all such values); †Measured by paired t-test between baseline and 8 week within each group at p < 0.05; ‡Baseline level between standard care group and intervention group showed no statistical significance after independent t-test.
Figure 2.
Daily fruit and vegetable intake between standard care control group and intervention group. The statistical significance measured by paired t-test. *Significant difference between baseline and 8 week (p < 0.001).
Changes in serum antioxidant levels after the 8 week nutrition intervention are presented in Table 5. Serum carotene concentration was significantly decreased in the standard care group (p < 0.001), but not in the intervention group. Serum concentrations of vitamin A (p = 0.048) and vitamin E (p = 0.004) in the intervention group were significantly increased, with no significant change in the standard care group.
Table 5.
Changes in serum antioxidant levels after intensive nutritional counseling
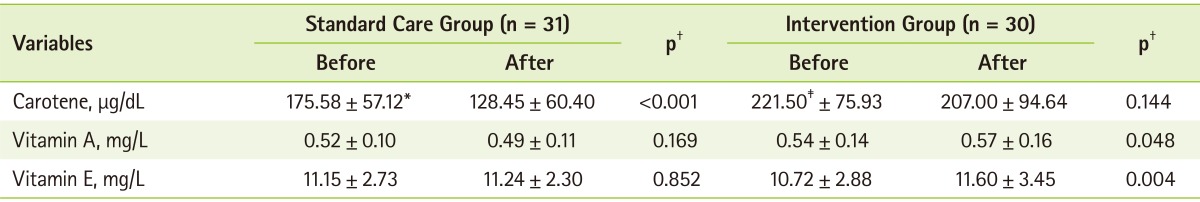
*Values are means ± SD (all such values); †Measured by paired t-test between baseline and 8 week within each group at p < 0.05; ‡Baseline level between standard care group and intervention group showed no statistical significance after independent t-test.
Effect on quality of life
In the standard care group, physical well-being score was significantly increased after nutrition intervention (p = 0.017). However, there were no significant differences in social/family well-being, emotional well-being, and functional well-being, breast cancer subscale after 8 weeks (Table 6).
Table 6.
Effect of intervention on quality of life
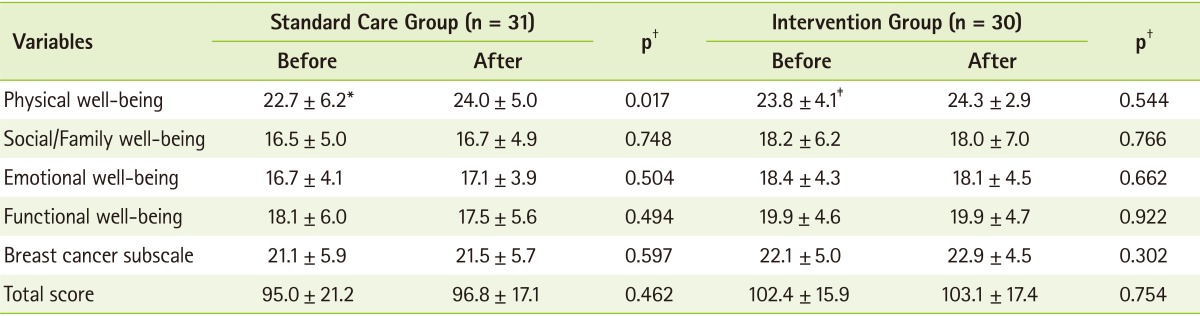
*Values are means ± SD (all such values); †Measured by paired t-test between baseline and 8 week within each group at p < 0.05. The higher score shows the better quality of life; ‡Baseline level between standard care group and intervention group showed no statistical significance after independent t-test.
Discussion
The goal for this particular nutrition intervention was to adopt and maintain an antioxidant rich dietary habit of breast cancer patients. This nutrition intervention program was designed to improve knowledge and skills in selecting phytochemical rich foods and to improve motivation with respect to healthy behavior in the patients. The results of this study showed that the 8-week nutrition intervention program primarily based on dietary counseling, supplemented by cooking classes and health-related materials, can promote a substantial change in the overall dietary pattern, with significant increases in consumptions of phytochemical rich fruit and vegetable.
The health benefits of fruit and vegetable seen in epidemiological studies are the main reasons for the recommended intake of at least 400 g of fruit and vegetable per day, potatoes not included [23]. The world cancer research fund (WCRF) panel of experts also recommended that the consumption of 400 grams/day or more of a variety of vegetables and and fruits, irrespective of other diet and lifestyle patterns, could decrease overall cancer incidence by at least 20% [24]. Accordingly, several clinical trials have intervened specifically on fruit and vegetable consumption. Pierce et al. [25] reported that telephone counseling intervention including cooking classes and monthly newsletters led to significant increase in fruit (18%, 0.6 serving/d) and vegetable (82%, 3.2 serving/d) intake in the intervention group of breast cancer survivors. Smith-Warner et al. [26] also showed that after 1-year diet intervention to increase fruit and vegetable consumption to at least 8 servings per day in an at-risk population, the intervention group had increased their daily fruit and vegetable intake an average of 5.5 servings over 1 year; the standard care group had an average decrease of 0.5 servings per day. In agreement with these intervention trial findings, we found that total fruit and vegetable (excluding kimchi and Korean pickles, etc) consumption in the intervention group was increased by 56.4% (382 g/d, p < 0.001). In detail, there was a 74.6 % (306 g/d, p < 0.001) increase of vegetable and a 28.3% (76 g/d) increase of fruit. The participants achieved these changes via increasing frequency and/or serving size of foods already consuming. In addition, the participants were more successful at increasing vegetable rather than fruit consumption. This may be due to food preferences and convenience because the Korean side dishes that use a wide variety of vegetables are easier to integrate into current eating pattern. These results suggest that it is indeed possible to further increase individual's total fruit and vegetable intake to more than the 1,000 g/d (equivalent to >14 servings), even if the intervention program is only provided for a short-term period.
The change in dietary intake was validated by increases in serum antioxidant nutrient levels which are considered objective biomarkers of fruit and vegetable intake [27,28]. In the intervention group, the average daily intake of vitamin A, vitamin C, vitamin E and β-carotene was significantly increased after the nutrition intervention (p < 0.001, respectively). As expected, serum vitamin A (5.6%, 0.03 mg/L) and vitamin E (8.2%, 0.88 mg/L) levels also were significantly increased after nutrition intervention. Higher dietary intakes and blood concentrations of carotenoids (precursor of vitamin A), including β-carotene, have been shown to reduce breast cancer risk although not entirely consistent [29,30]. According to results by performing a meta-analysis of 11 studies, intake of 7,000 µg per day or more of β-carotene was associated with 18% reduction of breast cancer risk compared with intake of 1,000 µg per day or less [31]. Sato et al. [32] reported that the risk of developing breast cancer in women with high levels of serum β-carotene, lycopene, and total carotene was approximately half of that of women with low levels of these nutrients. Although the intervention did not change the serum carotene level directly, it is hypothesized that the intervention would influence this variable.
Nutrition plays an important role in a cancer patient's overall health and QOL. Accordingly, cancer survivors are often motivated to modify their diets and seek nutritional guidance to reduce cancer recurrence risk. Some studies suggest that nutrition intervention improves QOL of cancer patients [33-36], whereas others report no such benefits [37,38]. In the current study, we could not observe a significant impact on the QOL in the both groups after the intervention. This results show that even though the nutrition intervention participants made significant modifications in their eating behavior, it might be hard to induce improvement on the QOL due to short-term interventions. The physical wellness was significantly increased in the control group, which is hard to explain. It may be possible that because the overall scores in the control group was rather lower than the intervention group, it was easier to be restored to normal level after 8 weeks.
Waist circumference and BMI are predictor biomarkers of breast cancer risk [39,40]. Especially, waist circumference as a measure of visceral adiposity is associated with increased risk of cancer development; is a stronger predictor of cancer risk than BMI [41]. In this study, waist circumference was significantly decreased in the intervention group (p < 0.001) even though BMI remained unchanged. Although not a primary goal of the study, this waist circumference reduction would be considered as desirable outcome for the breast cancer patients.
It should be noted that this study has several limitations. First, the period of the intervention was short. Thus, there is a need to examine if the effects of intervention program would be sustained over the long-term period. Second, fruit and vegetable intake was measured through self-reports rather than direct inspection of food consumption. Self reports can lead to response bias. The participants knew that the goal was to promote their fruit and vegetable consumption, therefore may report it. Indeed, even though the diet screening phase based on fruit and vegetable intake for participant eligibility, total fruit and vegetable intakes were above 500 g at the beginning of the intervention in the both groups. Despite these limitations, our study also has major strength. Cooking class provided an opportunity to taste new foods and a supportive learning environment. The participants could observe the dietitian to show cooking skills, practice these skills, and then demonstrate the skills themselves.
In conclusion, the results of this study showed that the 8-week nutrition intervention can facilitate positive dietary change, and this was reflected in increased fruit and vegetable intake and enhanced serum antioxidant nutrient levels such as vitamin A and vitamin E, but no significant change in QOL.
Footnotes
We declare that we have no conflict of interest.
References
- 1.Ministry of Health & Welfare; National Cancer Center, Korea Central Cancer Registry. Annual report of cancer statistics in Korea in 2010. Goyang: Korea Central Cancer Registry; 2012. [Google Scholar]
- 2.Park SK, Kang D, Kim Y, Yoo KY. Epidemiologic characteristics of the breast cancer in Korea. J Korean Med Assoc. 2009;52:937–945. [Google Scholar]
- 3.Ahn SH Korean Breast Cancer Society. Clinical characteristics of breast cancer patients in Korea in 2000. Arch Surg. 2004;139:27–30. doi: 10.1001/archsurg.139.1.27. [DOI] [PubMed] [Google Scholar]
- 4.Son BH, Kwak BS, Kim JK, Kim HJ, Hong SJ, Lee JS, Hwang UK, Yoon HS, Ahn SH. Changing patterns in the clinical characteristics of Korean patients with breast cancer during the last 15 years. Arch Surg. 2006;141:155–160. doi: 10.1001/archsurg.141.2.155. [DOI] [PubMed] [Google Scholar]
- 5.Bessaoud F, Daurès JP, Gerber M. Dietary factors and breast cancer risk: a case control study among a population in Southern France. Nutr Cancer. 2008;60:177–187. doi: 10.1080/01635580701649651. [DOI] [PubMed] [Google Scholar]
- 6.Edefonti V, Randi G, Decarli A, La Vecchia C, Bosetti C, Franceschi S, Dal Maso L, Ferraroni M. Clustering dietary habits and the risk of breast and ovarian cancers. Ann Oncol. 2009;20:581–590. doi: 10.1093/annonc/mdn594. [DOI] [PubMed] [Google Scholar]
- 7.Zhang CX, Ho SC, Chen YM, Fu JH, Cheng SZ, Lin FY. Greater vegetable and fruit intake is associated with a lower risk of breast cancer among Chinese women. Int J Cancer. 2009;125:181–188. doi: 10.1002/ijc.24358. [DOI] [PubMed] [Google Scholar]
- 8.Smith-Warner SA, Spiegelman D, Yaun SS, Adami HO, Beeson WL, van den Brandt PA, Folsom AR, Fraser GE, Freudenheim JL, Goldbohm RA, Graham S, Miller AB, Potter JD, Rohan TE, Speizer FE, Toniolo P, Willett WC, Wolk A, Zeleniuch-Jacquotte A, Hunter DJ. Intake of fruits and vegetables and risk of breast cancer: a pooled analysis of cohort studies. JAMA. 2001;285:769–776. doi: 10.1001/jama.285.6.769. [DOI] [PubMed] [Google Scholar]
- 9.Wang C, Baumgartner RN, Yang D, Slattery ML, Murtaugh MA, Byers T, Hines LM, Giuliano AR, Baumgartner KB. No evidence of association between breast cancer risk and dietary carotenoids, retinols, vitamin C and tocopherols in Southwestern Hispanic and non-Hispanic White women. Breast Cancer Res Treat. 2009;114:137–145. doi: 10.1007/s10549-008-9979-3. [DOI] [PubMed] [Google Scholar]
- 10.van Gils CH, Peeters PH, Bueno-de-Mesquita HB, Boshuizen HC, Lahmann PH, Clavel-Chapelon F, Thiébaut A, Kesse E, Sieri S, Palli D, Tumino R, Panico S, Vineis P, Gonzalez CA, Ardanaz E, Sánchez MJ, Amiano P, Navarro C, Quirós JR, Key TJ, Allen N, Khaw KT, Bingham SA, Psaltopoulou T, Koliva M, Trichopoulou A, Nagel G, Linseisen J, Boeing H, Berglund G, Wirfält E, Hallmans G, Lenner P, Overvad K, Tjønneland A, Olsen A, Lund E, Engeset D, Alsaker E, Norat T, Kaaks R, Slimani N, Riboli E. Consumption of vegetables and fruits and risk of breast cancer. JAMA. 2005;293:183–193. doi: 10.1001/jama.293.2.183. [DOI] [PubMed] [Google Scholar]
- 11.Liu RH. Potential synergy of phytochemicals in cancer prevention: mechanism of action. J Nutr. 2004;134:3479S–3485S. doi: 10.1093/jn/134.12.3479S. [DOI] [PubMed] [Google Scholar]
- 12.Thomson CA, Stendell-Hollis NR, Rock CL, Cussler EC, Flatt SW, Pierce JP. Plasma and dietary carotenoids are associated with reduced oxidative stress in women previously treated for breast cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:2008–2015. doi: 10.1158/1055-9965.EPI-07-0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winters BL, Mitchell DC, Smiciklas-Wright H, Grosvenor MB, Liu W, Blackburn GL. Dietary patterns in women treated for breast cancer who successfully reduce fat intake: the Women's Intervention Nutrition Study (WINS) J Am Diet Assoc. 2004;104:551–559. doi: 10.1016/j.jada.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 14.Pierce JP, Newman VA, Natarajan L, Flatt SW, Al-Delaimy WK, Caan BJ, Emond JA, Faerber S, Gold EB, Hajek RA, Hollenbach K, Jones LA, Karanja N, Kealey S, Madlensky L, Marshall J, Ritenbaugh C, Rock CL, Stefanick ML, Thomson C, Wasserman L, Parker BA. Telephone counseling helps maintain long-term adherence to a high-vegetable dietary pattern. J Nutr. 2007;137:2291–2296. doi: 10.1093/jn/137.10.2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newman VA, Thomson CA, Rock CL, Flatt SW, Kealey S, Bardwell WA, Caan BJ, Pierce JP Women's Healthy Eating and Living (WHEL) Study Group. Achieving substantial changes in eating behavior among women previously treated for breast cancer--an overview of the intervention. J Am Diet Assoc. 2005;105:382–391. doi: 10.1016/j.jada.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Wayne SJ, Baumgartner K, Baumgartner RN, Bernstein L, Bowen DJ, Ballard-Barbash R. Diet quality is directly associated with quality of life in breast cancer survivors. Breast Cancer Res Treat. 2006;96:227–232. doi: 10.1007/s10549-005-9018-6. [DOI] [PubMed] [Google Scholar]
- 17.Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol. 2005;23:1431–1438. doi: 10.1200/JCO.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 18.Corle DK, Sharbaugh C, Mateski DJ, Coyne T, Paskett ED, Cahill J, Daston C, Lanza E, Schatzkin A PPT Study Group. Polyp Prevention Trial. Self-rated quality of life measures: effect of change to a low-fat, high-fiber, fruit and vegetable enriched diet. Ann Behav Med. 2001;23:198–207. doi: 10.1207/S15324796ABM2303_7. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Health and Welfare, Korea Institute for Health and Social Affairs; Korea Health Industry Development Institute; Korea Centers for Disease Control and Prevention. The Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005. Seoul: Korea Institute for Health and Social Affairs; 2006. [Google Scholar]
- 20.Do MH, Lee SS, Jung PJ, Lee MH. The effect of individual nutrition counseling on diet and nutrition status of postoperative breast cancer patients. Korean J Nutr. 2004;37:557–565. [Google Scholar]
- 21.Bieri JG, Tolliver TJ, Catignani GL. Simultaneous determination of alpha-tocopherol and retinol in plasma or red cells by high pressure liquid chromatography. Am J Clin Nutr. 1979;32:2143–2149. doi: 10.1093/ajcn/32.10.2143. [DOI] [PubMed] [Google Scholar]
- 22.Functional Assessment of Chronic Illness Therapy (US) Functional assessment of cancer therapy-breast cancer version 4-Korean version. Elmhurst (IL): Functional Assessment of Chronic Illness Therapy; 2008. [cited 2013 December]. Availble from: http://www.facit.org/FACITOrg/Questionnaires. [Google Scholar]
- 23.World Health Organization (CH); Food and Agriculture Organization (US) Diet, nutrition and the prevention of chronic diseases. Report of a joint WHO/FAO expert consultation. WHO technical report series No. 916. Geneva: World Health Organization; 2003. [PubMed] [Google Scholar]
- 24.World Cancer Research Fund; American Institute for Cancer Research. Food, nutrition, and the prevention of cancer: a global perspective. Washington DC: American Institute for Cancer Research; 2007. [DOI] [PubMed] [Google Scholar]
- 25.Pierce JP, Newman VA, Flatt SW, Faerber S, Rock CL, Natarajan L, Caan BJ, Gold EB, Hollenbach KA, Wasserman L, Jones L, Ritenbaugh C, Stefanick ML, Thomson CA, Kealey S Women's Healthy Eating and Living (WHEL) Study Group. Telephone counseling intervention increases intakes of micronutrient- and phytochemical-rich vegetables, fruit and fiber in breast cancer survivors. J Nutr. 2004;134:452–458. doi: 10.1093/jn/134.2.452. [DOI] [PubMed] [Google Scholar]
- 26.Smith-Warner SA, Elmer PJ, Tharp TM, Fosdick L, Randall B, Gross M, Wood J, Potter JD. Increasing vegetable and fruit intake: randomized intervention and monitoring in an at-risk population. Cancer Epidemiol Biomarkers Prev. 2000;9:307–317. [PubMed] [Google Scholar]
- 27.Al-Delaimy WK, Ferrari P, Slimani N, Pala V, Johansson I, Nilsson S, Mattisson I, Wirfalt E, Galasso R, Palli D, Vineis P, Tumino R, Dorronsoro M, Pera G, Ocké MC, Bueno-de-Mesquita HB, Overvad K, Chirlaque M, Trichopoulou A, Naska A, Tjønneland A, Olsen A, Lund E, Alsaker EH, Barricarte A, Kesse E, Boutron-Ruault MC, Clavel-Chapelon F, Key TJ, Spencer E, Bingham S, Welch AA, Sanchez-Perez MJ, Nagel G, Linseisen J, Quirós JR, Peeters PH, van Gils CH, Boeing H, van Kappel AL, Steghens JP, Riboli E. Plasma carotenoids as biomarkers of intake of fruits and vegetables: individual-level correlations in the European Prospective Investigation into Cancer and Nutrition (EPIC) Eur J Clin Nutr. 2005;59:1387–1396. doi: 10.1038/sj.ejcn.1602252. [DOI] [PubMed] [Google Scholar]
- 28.McEligot AJ, Rock CL, Flatt SW, Newman V, Faerber S, Pierce JP. Plasma carotenoids are biomarkers of long-term high vegetable intake in women with breast cancer. J Nutr. 1999;129:2258–2263. doi: 10.1093/jn/129.12.2258. [DOI] [PubMed] [Google Scholar]
- 29.Pan SY, Zhou J, Gibbons L, Morrison H, Wen SW Canadian Cancer Registries Epidemiology Research Group [CCRERG] Antioxidants and breast cancer risk- a population-based case-control study in Canada. BMC Cancer. 2011;11:372. doi: 10.1186/1471-2407-11-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duncan AM. The role of nutrition in the prevention of breast cancer. AACN Clin Issues. 2004;15:119–135. doi: 10.1097/00044067-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Gandini S, Merzenich H, Robertson C, Boyle P. Meta-analysis of studies on breast cancer risk and diet: the role of fruit and vegetable consumption and the intake of associated micronutrients. Eur J Cancer. 2000;36:636–646. doi: 10.1016/s0959-8049(00)00022-8. [DOI] [PubMed] [Google Scholar]
- 32.Sato R, Helzlsouer KJ, Alberg AJ, Hoffman SC, Norkus EP, Comstock GW. Prospective study of carotenoids, tocopherols, and retinoid concentrations and the risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2002;11:451–457. [PubMed] [Google Scholar]
- 33.Isenring EA, Capra S, Bauer JD. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer. 2004;91:447–452. doi: 10.1038/sj.bjc.6601962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol. 2005;23:1431–1438. doi: 10.1200/JCO.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 35.Steptoe A, Perkins-Porras L, Hilton S, Rink E, Cappuccio FP. Quality of life and self-rated health in relation to changes in fruit and vegetable intake and in plasma vitamins C and E in a randomised trial of behavioural and nutritional education counselling. Br J Nutr. 2004;92:177–184. doi: 10.1079/BJN20041177. [DOI] [PubMed] [Google Scholar]
- 36.Marín Caro MM, Laviano A, Pichard C. Nutritional intervention and quality of life in adult oncology patients. Clin Nutr. 2007;26:289–301. doi: 10.1016/j.clnu.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 37.Halfdanarson TR, Thordardottir E, West CP, Jatoi A. Does dietary counseling improve quality of life in cancer patients? A systematic review and meta-analysis. J Support Oncol. 2008;6:234–237. [PubMed] [Google Scholar]
- 38.Persson CR, Johansson BB, Sjöden PO, Glimelius BL. A randomized study of nutritional support in patients with colorectal and gastric cancer. Nutr Cancer. 2002;42:48–58. doi: 10.1207/S15327914NC421_7. [DOI] [PubMed] [Google Scholar]
- 39.Hajian-Tilaki KO, Gholizadehpasha AR, Bozorgzadeh S, Hajian-Tilaki E. Body mass index and waist circumference are predictor biomarkers of breast cancer risk in Iranian women. Med Oncol. 2011;28:1296–1301. doi: 10.1007/s12032-010-9629-6. [DOI] [PubMed] [Google Scholar]
- 40.Wang Y, Jacobs EJ, Patel AV, Rodríguez C, McCullough ML, Thun MJ, Calle EE. A prospective study of waist circumference and body mass index in relation to colorectal cancer incidence. Cancer Causes Control. 2008;19:783–792. doi: 10.1007/s10552-008-9141-x. [DOI] [PubMed] [Google Scholar]
- 41.Moore LL, Bradlee ML, Singer MR, Splansky GL, Proctor MH, Ellison RC, Kreger BE. BMI and waist circumference as predictors of lifetime colon cancer risk in Framingham Study adults. Int J Obes Relat Metab Disord. 2004;28:559–567. doi: 10.1038/sj.ijo.0802606. [DOI] [PubMed] [Google Scholar]