Abstract
Purpose
The primary aim of this paper was to evaluate the expression of extracellular matrix metalloproteinase inducer (EMMPRIN) and its relationship with proangiogenic factors and microvessel density (MVD) in ovarian cancer.
Methods
The study group included 58 epithelial ovarian cancers (EOCs), 35 benign ovarian tumors, and 21 normal ovaries. The expression of EMMPRIN, vascular endothelial growth factor (VEGF), and basic fibroblast growth factor (bFGF) was assessed by ELISA of tissue homogenates. Antibodies against CD105, CD31, and CD34 were used to immunohistochemically assess MVD.
Results
We have found significantly higher EMMPRIN expression in EOC than in benign ovarian tumors and normal ovaries. Similarly, the VEGF expression was higher in EOC than in benign ovarian tumors and normal ovaries. By contrast, bFGF expression was lower in EOC than in benign ovarian tumors and ovary samples. EMMPRIN expression in EOC was directly correlated with VEGF expression and CD105-MVD, but inversely correlated with bFGF expression. Grade 2/3 ovarian cancers had increased expression of EMMPRIN and VEGF, increased CD105-MVD, and lowered expression of bFGF compared to grade 1 ovarian cancers. Moreover, EMMPRIN expression was higher in advanced (FIGO III and IV) ovarian cancer.
Conclusions
The upregulation of EMMPRIN and VEGF expression is correlated with increased CD105-MVD and silenced bFGF, which suggests early and/or reactivated angiogenesis in ovarian cancer. Aggressive EOC is characterized by the following: high expression of EMMPRIN and VEGF, high CD105-MVD, and low expression of bFGF.
Keywords: Extracellular matrix metalloproteinase inducer, EMMPRIN, Vascular endothelial growth factor, Basic fibroblast growth factor, Ovarian cancer, Angiogenesis
Introduction
Epithelial ovarian cancer (EOC) is the leading cause of death from gynecological malignancies and the fifth leading cause of cancer-related death among women in the United States (Jemal et al. 2010). The 5-year survival rate is approximately 45.6 % (Howlader et al. 2012). Although complete remission after the primary treatment is achieved in approximately half of patients, the majority will relapse, and the disease then becomes fatal (Gadducci et al. 1998; du Bois et al. 2003). The poor prognosis of ovarian cancer patients has motivated the development of new anticancer therapies. Recently, antiangiogenic treatments have been introduced, and several trials have reported encouraging results in the management of ovarian cancer patients (Burger 2011).
Current antiangiogenic strategies are primarily based on the inhibition of vascular endothelial growth factor (VEGF). Two randomized placebo-controlled trials reported a significant response and prolonged progression-free survival (PFS) after the incorporation of bevacizumab, an anti-VEGF monoclonal antibody, into the primary chemotherapy regimen for ovarian cancer patients (Burger et al. 2011; Perren et al. 2011). However, after the discontinuation of maintenance bevacizumab therapy, the disease was exacerbated, and no improvement in overall survival was observed (Burger et al. 2011; Perren et al. 2011). In the case of recurrent or persistent ovarian cancer, bevacizumab monotherapy produced a 16–21 % response rate, and the median PFS was less than 5 months (Burger et al. 2007; Cannistra et al. 2007). Taken together, these results suggest that anti-VEGF therapy in ovarian cancer is effective but insufficient. Particularly in the primary treatment, the improvement in PFS was modest (Tomao et al. 2013; Collinson et al. 2013). The multipurpose blockade of VEGF and other proangiogenic factors may be more effective than a single anti-VEGF approach (Bergers and Hanahan 2008; Alessi et al. 2009; Burger 2011). Potential strategies include the application of multikinase inhibitors that impede the signaling of several important proangiogenic molecules, such as VEGF, platelet-derived growth factor (PDGF), and fibroblast growth factor (FGF). Such multikinase inhibitors are currently in clinical trials in ovarian cancer patients (Burger 2011).
Extracellular matrix metalloproteinase inducer (EMMPRIN), also known as basigin or cluster of differentiation 147 (CD147), is another candidate for the antiangiogenic treatment of cancer. EMMPRIN is a transmembrane protein member of the immunoglobulin family of receptors (Weidle et al. 2010). As a membrane protein, EMMPRIN has been suggested to act via cell–cell interactions with surrounding cells to stimulate the secretion of matrix metalloproteinases (MMPs) (Biswas et al. 1995). Homotypic EMMPRIN–EMMPRIN interactions are likely responsible for EMMPRIN activity (Sun and Hemler 2001; Seizer et al. 2009). However, it is not known whether direct cell–cell contact is necessary because soluble EMMPRIN and EMMPRIN-enriched tumor microvesicles also have the ability to stimulate the secretion of MMPs (Li et al. 2001; Egawa et al. 2006; Millimaggi et al. 2007).
High expression of EMMPRIN has been observed in various human neoplasms and frequently correlated with cancer aggressiveness (Zucker et al. 2001; Riethdorf et al. 2006). In cancer development, EMMPRIN stimulates the secretion of MMPs, which leads to the destruction of the extracellular matrix to facilitate cancer cell migration, metastasis, and angiogenesis (Gabison et al. 2005; Weidle et al. 2010). Furthermore, EMMPRIN also stimulates VEGF secretion (Tang et al. 2005; Voigt et al. 2009; Bougatef et al. 2009). It was also shown that EMMPRIN may enhance angiogenesis by activating the proliferation, survival, and migration of endothelial cells (ECs) (Chen et al. 2009).
Although several studies have identified EMMPRIN expression in ovarian cancer, little is known about the role of EMMPRIN in the angiogenesis of ovarian cancer. Thus, the main purpose of this study was to investigate the potential association between the expression of EMMPRIN and other proangiogenic factors with microvessel density (MVD) in ovarian cancer samples.
Materials and methods
Participants
The study group included 58 samples of EOC collected from women treated in the Division of Gynecological Surgery, Poznan University of Medical Sciences, Poland, during the years 2007–2012. The control group comprised 35 samples of benign ovarian tumors taken from patients who were operated on in our division. In addition, 21 samples of normal ovaries were obtained from perimenopausal women (median age 51; range 46–55 years), operated on due to non-oncological conditions. The materials obtained during surgery were divided into 2 parts. The first part was fixed in buffered formalin, and the second part was frozen just after collection and stored at −82 °C.
Tumors removed during surgery were examined histopathologically and classified according to WHO criteria. The histological types of the EOCs included in the study were as follows: 22 serous, 8 mucinous, 7 endometrioid, 4 clear cell adenocarcinomas, and 17 undifferentiated carcinomas. The group of benign ovarian tumors included the following: 10 serous and 5 mucinous cystadenomas, 7 endometrioid cysts, 10 adult teratomas, and 3 fibrothecomas. Malignant tumors were classified into three histological grades; 13, 11, and 34 tumors were classified as grades 1, 2, and 3, respectively. The clinical stage of the disease was specified using the criteria of the International Federation of Gynecology and Obstetrics (FIGO). Malignant tumors were classified according to the FIGO stage of the disease as follows: 15 stage I patients, 9 stage II patients, 24 stage III patients, and 10 stage IV patients.
This study received local ethics committee approval, and all patients signed consent forms before participating.
EMMPRIN, VEGF, and bFGF expression
The expression of EMMPRIN, VEGF, and bFGF was assessed by ELISA of tissue homogenates. Homogenates were obtained from freshly frozen tissue samples. The analyzed tissue specimens were homogenized mechanically in a buffer containing 150 mM NaCl (Sigma Aldrich, USA), 5 mM EDTA (Sigma Aldrich, USA), 50 mM Tris–HCl, pH 7.4 (Sigma Aldrich, USA), 1 % Triton X-100 (Sigma Aldrich, USA), and a protease inhibitor cocktail (Sigma Aldrich, USA, catalogue number S8820). The homogenates were centrifuged for 15 min in Eppendorf tubes at 10,000 rpm. The supernatants were used for ELISA to measure the concentration of proangiogenic factors (VEGF, bFGF, and EMMPRIN). We used commercially available ELISA kits obtained from R&D Systems, Minneapolis, Minnesota, USA. The expression of VEGF, bFGF, and EMMPRIN is reported as the tissue protein content (pg/mg total protein). Protein concentrations were assessed according to Lowry’s method. No repeated freeze–thaw cycles were performed before ELISA analysis in any case. Before analysis, we have performed micro-dissection to exclude connective tissue and large vessels from the specimen. The samples were not batched for the analysis, and until statistical analysis, all the members of the team involved in ELISA analysis were blinded against studied groups. The analyses were performed in duplicates for each series, and following coefficients of variation (cv) were calculated for intra-assay variability: VEGF = 13 %; bFGF = 6.98 %, EMMPRIN = 11.00 %.
Immunohistochemistry and MVD assessment
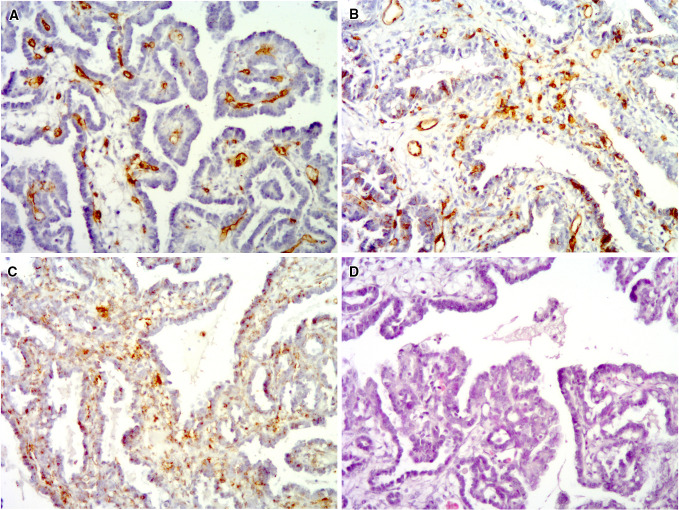
Formalin-fixed tissue samples were used to evaluate MVD. Immunohistochemistry was used for endothelium labeling with antibodies against CD105, CD31, and CD34. A modified protocol proposed by Rubatt et al. (2009) was used for the assessment of MVD. Briefly, one observer screened the whole sample by light microscopy at 40× magnification to identify the three largest microvessel clusters (“hot spots”). Only hot spots located near neoplastic cells were analyzed. Subsequently, microvessels were counted in each of the selected hot spots at 400× magnification. Only microvessels with lumen were considered. Large vessels and vessels with muscular walls were not counted. The median number of microvessels from 3 hot spots was used for the final analysis. MVD assessment was conducted by histopathologist experienced in angiogenesis studies. Representative immunohistochemical staining is presented in Fig. 1.
Fig. 1.
Clear cell ovarian carcinoma showing high MVD for all of the analyzed endothelial markers: CD31 (a), CD34 (b), and CD105 (c). Hematoxylin and eosin staining of the tumor is presented in (d)
Statistical analysis
Statistical analysis was performed with GraphPad InStat 3.06, and following statistical tests were used: Kolmogorov–Smirnov test (K–S test), Kruskal–Wallis test (nonparametric ANOVA) with Dunn’s multiple comparisons test as a post hoc test, unpaired t test, Mann–Whitney test, and Spearman rank correlation. Logistic regression was conducted using MedCalc 11.4.2.0 software.
Results
VEGF, bFGF, and EMMPRIN in EOCs, benign ovarian tumors, and normal ovaries
The median EMMPRIN expression in the EOC group was significantly higher than that in the benign ovarian tumor and normal ovary groups (P = 0.0002). Similarly, the median VEGF expression was higher in the EOC group compared to the benign ovarian tumor and normal ovary groups (P < 0.0001). By contrast, the median bFGF expression was significantly lower in the EOC group compared to the benign ovarian tumor and normal ovary groups (P < 0.0001). These results are summarized in Table 1.
Table 1.
Median concentration of proangiogenic factors within the three analyzed groups
| Ovarian cancer (n = 58) | Benign ovarian tumors (n = 35) | Normal ovaries (n = 21) | P value | |
|---|---|---|---|---|
|
VEGF Median pg/mg protein (range, min–max) |
444.64 (0–3,000.00) | 2.02 (0–634.75) | 4.93 (1.67–79.35) | <0.0001 |
|
EMMPRIN Median ng/mg protein (range, min–max) |
33.41 (8.48–106.50) | 22.94 (13.26–48.38) | 21.06 (10.65–40.75) | 0.0002 |
|
bFGF Median ng/mg protein (range, min–max) |
0.97 (0.17–13.32) | 2.20 (0.67–50.31) | 8.04 (2.56-12.91) | <0.0001 |
Bold values are statistically significant (P < 0.05)
MVD in the studied groups
We observed significantly higher (P = 0.0003) MVD in the ovarian cancer tumors (25 vessels/mm2; range 0–57) than in the benign ovarian tumors (6 vessels/mm2; 0–70) and normal ovaries (6 vessels/mm2; 0–26), as assessed by CD105 staining. There were no differences in MVD as assessed by antibodies against CD31 and CD34 between the three studied groups. The results of the MVD assessment are presented in Table 2.
Table 2.
MVD assessment in the studied group of patients and the healthy individuals
| Ovarian cancer (n = 58) median vessels/mm2 (range, min–max) | Benign ovarian tumors (n = 35) Median vessels/mm2 (range, min–max) | Normal ovaries (n = 21) median vessels/mm2 (range, min–max) | P value | |
|---|---|---|---|---|
| CD105-MVD | 25 (0–57) | 6 (0–70) | 6 (0–26) | 0.0003 |
| CD31-MVD | 76 (19–241) | 70 (6–399) | 60 (31–284) | 0.817 |
| CD34-MVD | 70 (6–190) | 70 (6–386) | 114 (31–354) | 0.077 |
CD105-MVD, CD31-MVD, and CD34-MVD refer to MVD assessed with antibodies against CD105, CD31, and CD34, respectively
Bold value is statistically significant (P < 0.05)
Proangiogenic factors expression in relation to MVD
In the EOC group, EMMPRIN expression positively correlated with MVD assessed by CD105 staining (R Spearman = 0.308, P = 0.031). Similarly, the expression of VEGF correlated positively with CD105-MVD (R Spearman = 0.285, P = 0.049). By contrast, there was no significant relationship between bFGF expression and CD105-MVD (R Spearman = −0.149, P = 0.314). Neither CD31-MVD nor CD34-MVD correlated with the expression of any of the analyzed proangiogenic factors. The correlation results are summarized in Table 3. In the logistic regression model, none of the three analyzed proangiogenic factors was found to be an independent prognostic factor of CD105-MVD higher than the 75th percentile (>38 microvessels/mm2).
Table 3.
Correlation analyses between the expression of proangiogenic factors and MVD in the EOC group
| CD105-MVD (P value) | CD31-MVD (P value) | CD34-MVD (P value) | |
|---|---|---|---|
| VEGF | R Spearman = 0.285 | R Spearman = 0.005 | R Spearman = −0.086 |
| P = 0.049 | P = 0.973 | P = 0.577 | |
| EMMPRIN | R Spearman = 0.308 | R Spearman = 0.193 | R Spearman = 0.151 |
| P = 0.031 | P = 0.183 | P = 0.323 | |
| bFGF | R Spearman = −0.149 | R Spearman = −0.256 | R Spearman = −0.167 |
| P = 0.314 | P = 0.08 | P = 0.278 |
CD105-MVD, CD31-MVD, and CD34-MVD refer to MVD assessed with antibodies against CD105, CD31, and CD34, respectively
Bold values are statistically significant (P < 0.05)
Reciprocal correlations between expression of proangiogenic factors
The analysis of correlations between the expression of proangiogenic factors revealed a significant positive correlation between EMMPRIN and VEGF expression (R Spearman = 0.364, P = 0.006), whereas the expression of EMMPRIN was inversely proportional to bFGF expression (R Spearman = −0.28, P = 0.035). The correlation between the expression of bFGF and VEGF was insignificant (R Spearman = −0.248, P = 0.07).
Proangiogenc factors expression and MVD regarding clinical features of EOC
The median EMMPRIN concentration was significantly higher in advanced ovarian cancer samples (FIGO III and IV) compared to early-stage tumor samples (FIGO I and II) (P = 0.013). Moreover, grade 2/3 ovarian cancers were characterized by the increased expression of EMMPRIN and VEGF, increased CD105-MVD, and the lowered expression of bFGF compared to grade 1 ovarian cancers (P = 0.026, 0.019, 0.017, and 0.018, respectively). Tables 4 and 5 show the expression of proangiogenic factors and the MVD assessment according to FIGO stage and the grade of ovarian cancer, respectively. However, we found no differences in EMMPRIN expression between various histopathological types of ovarian cancer. Similarly, there were no differences in VEGF or bFGF expression or MVD between the different histopathological types of ovarian cancer (Table 6).
Table 4.
Expression of proangiogenic factors and MVD according to the FIGO stage of ovarian cancer
| FIGO I and II (n = 24) | FIGO III and IV (n = 34) | P value | |
|---|---|---|---|
|
VEGF Median pg/mg protein (range, min–max) |
270.35 (0–2,371.3) | 610.35 (10.14–3,000.0) | 0.134 |
|
EMMPRIN Median ng/mg protein (range, min–max) |
26.52 (8.48–90.28) | 37.55 (10.65–106.50) | 0.013 |
|
bFGF Median ng/mg protein (range, min–max) |
0.88 (0.27–13.32) | 1.03 (0.17–8.33) | 0.966 |
|
CD105-MVD Median vessels/mm2 (range, min–max) |
16 (0–57) | 25 (0–51) | 0.203 |
|
CD31-MVD Median vessels/mm2 (range, min–max) |
63 (25–203) | 76 (19–241) | 0.392 |
|
CD34-MVD Median vessels/mm2 (range, min–max) |
57 (6–164) | 82 (32–190) | 0.171 |
CD105-MVD, CD31-MVD, and CD34-MVD refer to MVD assessed with antibodies against CD105, CD31, and CD34, respectively
Bold value is statistically significant (P < 0.05)
Table 5.
Expression of proangiogenic factors and MVD according to the grade of ovarian cancer
| G1 (n = 13) | G2/3 (n = 45) | P value | |
|---|---|---|---|
|
VEGF Median pg/mg protein (range, min–max) |
257.76 (0–1265.8) | 625.35 (10.14–3,000.0) | 0.019 |
|
EMMPRIN Median ng/mg protein (range, min–max) |
25.92 (8.48–44.25) | 35.90 (10.86–106.50) | 0.026 |
|
bFGF Median ng/mg protein (range, min–max) |
2.19 (0.72–13.32) | 0.82 (0.17–8.33) | 0.018 |
|
CD105-MVD Median vessels/mm2 (range, min–max) |
6 (0–44) | 28 (0–57) | 0.017 |
|
CD31-MVD Median vessels/mm2 (range, min–max) |
63 (25–241) | 76 (19–203) | 0.223 |
|
CD34-MVD Median vessels/mm2 (range, min–max) |
54 (6–146) | 76 (32–190) | 0.153 |
CD105-MVD, CD31-MVD, and CD34-MVD refer to MVD assessed with antibodies against CD105, CD31, and CD34, respectively
Bold values are statistically significant (P < 0.05)
Table 6.
Expression of proangiogenic factors and MVD according to the histopathological type of ovarian cancer
| Serous ovarian cancer (n = 22) | Mucinous ovarian cancer (n = 8) | Endometrioid ovarian cancer (n = 7) | Clear cell ovarian cancer (n = 4) | Undifferentiated carcinoma (n = 17) | P value | |
|---|---|---|---|---|---|---|
|
VEGF Median pg/mg protein (range, min–max) |
233.27 (0–3,000.0) | 512.8 (27.25–2,240.4) | 431.97 (166.20–2,298.3) | 1,070.8 (325.57–1,433.1) | 718.95 (10.14–3,000.0) | 0.152 |
|
EMMPRIN Median ng/mg protein (range, min–max) |
26.46 (10.65–88.22) | 25.81 (8.48–106.50) | 31.11 (13.35–60.43) | 34.96 (27.19–69.75) | 34.77 (10.86–90.28) | 0.874 |
|
bFGF Median ng/mg protein (range, min–max) |
1.03 (0.22–9.46) | 1.54 (0.17–3.60) | 0.81 (0.27–13.32) | 2.03 (0.19–5.93) | 0.94 (0.35–4.03) | 0.833 |
|
CD105-MVD Median vessels/mm2 (range, min–max) |
25 (0–38) | 19 (0–51) | 41 (13–51) | 25 (0–44) | 25 (0–57) | 0.573 |
|
CD31-MVD Median vessels/mm2 (range, min–max) |
73 (32–241) | 70 (19–95) | 101 (51–203) | 60 (44–82) | 63 (44–146) | 0.541 |
|
CD34-MVD Median vessels/mm2 (range, min–max) |
57 (6–165) | 57 (44–108) | 92 (57–146) | 57 (38–70) | 57 (6–190) | 0.585 |
CD105-MVD, CD31-MVD, and CD34-MVD refer to MVD assessed with antibodies against CD105, CD31, and CD34, respectively
Discussion
The results of our study indicate that EMMPRIN may contribute to the development of new blood vessels in ovarian cancer. Endoglin (CD105) is a well-established marker of active angiogenesis, as CD105 is expressed exclusively on newly formed vessels (Schliemann and Neri 2007; Dallas et al. 2008). By contrast, CD31 and CD34 are pan-endothelial markers that are found on endothelial cells of both new and mature vessels (Akagi et al. 2002). In the present study, we have shown a direct correlation between the expression of EMMPRIN and VEGF and MVD as assessed by antibodies against CD105. Similarly, we have revealed a direct correlation between the expression of VEGF and EMMPRIN. This result is supported by the previous findings in other neoplasms in which EMMPRIN was shown to stimulate the secretion of VEGF (Tang et al. 2005; Bougatef et al. 2009). However, in a logistic regression model, none of the analyzed proangiogenic factors independently indicated increased CD105-MVD. This may suggest that both molecules are important during the formation of new blood vessels in ovarian cancer.
Although the role of VEGF in ovarian cancer angiogenesis is well-established, there is limited data about the role of EMMPRIN (Yu et al. 2013). Millimaggi et al. (Millimaggi et al. 2007) demonstrated that microvesicles-containing EMMPRIN shed by ovarian cancer cell lines enhanced the proangiogenic activities of human umbilical vein endothelial cells (HUVECs). The stimulation of HUVECs by CD147-positive microvesicles increased invasiveness, the proliferation rate, MMP synthesis, and the formation of capillary-like structures. By contrast, microvesicles of low EMMPRIN concentration had a diminished ability to induce the proangiogenic phenotype of HUVECs (Millimaggi et al. 2007). In another study, Millimaggi et al. (Millimaggi et al. 2009) revealed that EMMPRIN expression in ovarian cancer cell lines is essential for vasculogenic mimicry (VM). VM is an alternative mechanism of angiogenesis in which tumor cells form tubes that act like microvessels. These channels are non-endothelial and are thus not relevant to our study, which was based on MVD evaluation (Millimaggi et al. 2009). VM is frequently associated with cancer aggressiveness (Sood et al. 2002). Indeed, in our study, we observed that EMMPRIN expression is higher in ovarian cancers diagnosed at an advanced stage and in grade 2/3 ovarian cancer when compared to grade 1 cancers. Similarly, Ueda et al. (Ueda et al. 2012) and Davidson et al. (2003) indicated that EMMPRIN expression was correlated with the poor prognosis of ovarian cancer patients. Thus, these results may support the relationship between EMMPRIN, VM, and the aggressiveness of ovarian cancer.
Various preclinical studies have demonstrated the proangiogenic properties of basic fibroblast growth factor. This growth factor can directly stimulate the proliferation and migration of endothelial cells, facilitate tube formation, sensitize ECs to other angiogenic factors, and stimulate the secretion of extracellular matrix remodeling proteases (Presta et al. 2005; Nissen et al. 2007). Giavazzi et al. (2003) suggest that bFGF and VEGF work synergistically to elicit angiogenesis. Interestingly, Alessi et al. (2009) demonstrated that targeting bFGF may overcome anti-VEGF resistance; thus, anti-bFGF therapy is undergoing clinical trials as an antiangiogenic therapy for ovarian cancer (Burger 2011). However, this is somewhat in contrast to our results, because we did not identify relationship between the expression of bFGF and the active angiogenesis. Therefore, we speculate that the timing of proangiogenic factors differs in the course of angiogenesis because VEGF appears earlier than bFGF (Lieu et al. 2011). Thus, increased EMPPRIN and VEGF expressions in malignant tumors associated with the upregulation of CD105 suggest the early phase and/or very active stimulation of angiogenesis in the studied malignant tumors.
Our study is the first to demonstrate an inverse correlation between the expression of EMMPRIN and bFGF in ovarian cancer tissue. Similar findings were obtained by Liu et al. (2011) in a study of head and neck cancer. The authors demonstrated that fibroblast growth factor receptor 2 (FGFR2) gene expression was inversely correlated with EMMPRIN expression. Moreover, Liu et al. (2011) showed that EMMPRIN-silenced tumors had more abundant stroma compared to controls. These results suggest that there could be an antagonistic interaction between EMMPRIN and bFGF. Evidence of the role of cancer-associated fibroblasts (CAFs) in the development and progression of cancer is increasing (Xing et al. 2010), and CAFs also play a substantial role in ovarian cancer (Schauer et al. 2011). Liu et al. (2011) suggest that tumor growth is fibroblast-dependent when EMMPRIN expression is low, while elevated EMMPRIN expression promotes fibroblast-independent tumor growth. Obermair et al. (1998) demonstrated that elevated tumor bFGF expression is correlated with favorable prognosis and that these tumors have greater stromal content. This is in agreement with the results of our study, because we have found higher bFGF expression in low-grade ovarian cancers, which tend to have better prognosis (Malpica et al. 2004). Additionally, we observed lower bFGF expression in ovarian cancer compared to benign ovarian tumors and normal ovaries. By contrast, some recent studies have shown that bFGF expression may be responsible for resistance to paclitaxel; thus, the exact role of bFGF as a prognostic factor in ovarian cancer is unclear (Gan et al. 2006). There appears to be close interactions between EMMPRIN and bFGF in the progression of ovarian cancer. However, exact prognostic significance of EMMRPIN/bFGF expression ratio should be verified according to survival analysis, and this is the main weakness of the presented study. We speculate that both EMMPRIN and bFGF may be key messengers between cancer cells and fibroblasts of the tumor stroma, but these interactions are likely very complex.
To conclude, the overexpression of EMMPRIN and VEGF in ovarian cancer creates a milieu of proangiogenic factors that may play a role in very early and/or reactivated angiogenesis. The upregulation of proangiogenic stimulants correlates with increased CD105-MVD; however, bFGF remains silenced. Additionally, high EMMPRIN/bFGF expression ratio is a new molecular profile of aggressive of EOC.
Acknowledgments
This paper was supported by Grant NR13 0006 06/2009 of The Polish National Centre for Research and Development, Poland, which is gratefully acknowledged.
Conflict of interest
The authors have no potential conflicts of interest to disclose.
References
- Akagi K, Ikeda Y, Sumiyoshi Y et al (2002) Estimation of angiogenesis with anti-CD105 immunostaining in the process of colorectal cancer development. Surgery 131:S109–S113. doi:10.1067/msy.2002.119361 [DOI] [PubMed] [Google Scholar]
- Alessi P, Leali D, Camozzi M et al (2009) Anti-FGF2 approaches as a strategy to compensate resistance to anti-VEGF therapy: long-pentraxin 3 as a novel antiangiogenic FGF2-antagonist. Eur Cytokine Netw 20:225–234. doi:10.1684/ecn.2009.0175 [DOI] [PubMed] [Google Scholar]
- Bergers G, Hanahan D (2008) Modes of resistance to anti-angiogenic therapy. Nat Rev Cancer 8:592–603. doi:10.1038/nrc2442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas C, Zhang Y, DeCastro R et al (1995) The human tumor cell-derived collagenase stimulatory factor (renamed EMMPRIN) is a member of the immunoglobulin superfamily. Cancer Res 55:434–439 [PubMed] [Google Scholar]
- Bougatef F, Quemener C, Kellouche S et al (2009) EMMPRIN promotes angiogenesis through hypoxia-inducible factor-2alpha-mediated regulation of soluble VEGF isoforms and their receptor VEGFR-2. Blood 114:5547–5556. doi:10.1182/blood-2009-04-217380 [DOI] [PubMed] [Google Scholar]
- Burger RA (2011) Overview of anti-angiogenic agents in development for ovarian cancer. Gynecol Oncol 121:230–238. doi:10.1016/j.ygyno.2010.11.035 [DOI] [PubMed] [Google Scholar]
- Burger RA, Sill MW, Monk BJ et al (2007) Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a gynecologic oncology group study. J Clin Oncol Off J Am Soc Clin Oncol 25:5165–5171. doi:10.1200/JCO.2007.11.5345 [DOI] [PubMed] [Google Scholar]
- Burger RA, Brady MF, Bookman MA et al (2011) Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med 365:2473–2483. doi:10.1056/NEJMoa1104390 [DOI] [PubMed] [Google Scholar]
- Cannistra SA, Matulonis UA, Penson RT et al (2007) Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol Off J Am Soc Clin Oncol 25:5180–5186. doi:10.1200/JCO.2007.12.0782 [DOI] [PubMed] [Google Scholar]
- Chen Y, Zhang H, Gou X et al (2009) Upregulation of HAb18G/CD147 in activated human umbilical vein endothelial cells enhances the angiogenesis. Cancer Lett 278:113–121. doi:10.1016/j.canlet.2009.01.004 [DOI] [PubMed] [Google Scholar]
- Collinson F, Hutchinson M, Craven R et al (2013) Predicting response to bevacizumab in ovarian cancer: a panel of potential biomarkers informing treatment selection. Clin Cancer Res. doi:10.1158/1078-0432.CCR-13-0489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallas NA, Samuel S, Xia L et al (2008) Endoglin (CD105): a marker of tumor vasculature and potential target for therapy. Clin cancer Res an Off J Am Assoc Cancer Res 14:1931–1937. doi:10.1158/1078-0432.CCR-07-4478 [DOI] [PubMed] [Google Scholar]
- Davidson B, Goldberg I, Berner A et al (2003) EMMPRIN (extracellular matrix metalloproteinase inducer) is a novel marker of poor outcome in serous ovarian carcinoma. Clin Exp Metastasis 20:161–169. doi:10.1023/A:1022696012668 [DOI] [PubMed] [Google Scholar]
- Du Bois A, Lück H-J, Meier W et al (2003) A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J Natl Cancer Inst 95:1320–1329. doi:10.1093/jnci/djg036 [DOI] [PubMed] [Google Scholar]
- Egawa N, Koshikawa N, Tomari T et al (2006) Membrane type 1 matrix metalloproteinase (MT1-MMP/MMP-14) cleaves and releases a 22-kDa extracellular matrix metalloproteinase inducer (EMMPRIN) fragment from tumor cells. J Biol Chem 281:37576–37585. doi:10.1074/jbc.M606993200 [DOI] [PubMed] [Google Scholar]
- Gabison EE, Hoang-Xuan T, Mauviel A, Menashi S (2005) EMMPRIN/CD147, an MMP modulator in cancer, development and tissue repair. Biochimie 87:361–368. doi:10.1016/j.biochi.2004.09.023 [DOI] [PubMed] [Google Scholar]
- Gadducci A, Sartori E, Maggino T et al (1998) Analysis of failures after negative second-look in patients with advanced ovarian cancer: an Italian multicenter study. Gynecol Oncol 68:150–155. doi:10.1006/gyno.1997.4890 [DOI] [PubMed] [Google Scholar]
- Gan Y, Wientjes MG, Au JL-S (2006) Expression of basic fibroblast growth factor correlates with resistance to paclitaxel in human patient tumors. Pharm Res 23:1324–1331. doi:10.1007/s11095-006-0136-6 [DOI] [PubMed] [Google Scholar]
- Giavazzi R, Sennino B, Coltrini D et al (2003) Distinct role of fibroblast growth factor-2 and vascular endothelial growth factor on tumor growth and angiogenesis. Am J Pathol 162:1913–1926. doi:10.1016/S0002-9440(10)64325-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJCK (2012) SEER Cancer Statistics Review, 1975-2009. Natl, Cancer Inst [Google Scholar]
- Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300. doi:10.3322/caac.20073 [DOI] [PubMed] [Google Scholar]
- Li R, Huang L, Guo H, Toole BP (2001) Basigin (murine EMMPRIN) stimulates matrix metalloproteinase production by fibroblasts. J Cell Physiol 186:371–379. doi:10.1002/1097-4652(2000)9999:999%3c000:AID-JCP1042%3e3.0.CO;2-8 [DOI] [PubMed] [Google Scholar]
- Lieu C, Heymach J, Overman M et al (2011) Beyond VEGF: inhibition of the fibroblast growth factor pathway and antiangiogenesis. Clin cancer Res an Off J Am Assoc Cancer Res 17:6130–6139. doi:10.1158/1078-0432.CCR-11-0659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Hartman YE, Warram JM et al (2011) Fibroblast growth factor receptor mediates fibroblast-dependent growth in EMMPRIN-depleted head and neck cancer tumor cells. Mol cancer Res MCR 9:1008–1017. doi:10.1158/1541-7786.MCR-11-0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malpica A, Deavers MT, Lu K et al (2004) Grading ovarian serous carcinoma using a two-tier system. Am J Surg Pathol 28:496–504. doi:10.1097/00000478-200404000-00009 [DOI] [PubMed] [Google Scholar]
- Millimaggi D, Mari M, D’Ascenzo S et al (2007) Tumor vesicle–associated CD147 modulates the angiogenic capability of endothelial cells. Neoplasia 9:349–357. doi:10.1593/neo.07133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millimaggi D, Mari M, D’ Ascenzo S et al (2009) Vasculogenic mimicry of human ovarian cancer cells: role of CD147. Int J Oncol 35:1423–1428. doi:10.3892/ijo_00000460 [DOI] [PubMed]
- Nissen LJ, Cao R, Hedlund E-M et al (2007) Angiogenic factors FGF2 and PDGF-BB synergistically promote murine tumor neovascularization and metastasis. J Clin Invest 117:2766–2777. doi:10.1172/JCI32479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obermair A, Speiser P, Reisenberger K et al (1998) Influence of intratumoral basic fibroblast growth factor concentration on survival in ovarian cancer patients. Cancer Lett 130:69–76. doi:10.1016/S0304-3835(98)00119-0 [DOI] [PubMed] [Google Scholar]
- Perren TJ, Swart AM, Pfisterer J et al (2011) A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med 365:2484–2496. doi:10.1056/NEJMoa1103799 [DOI] [PubMed] [Google Scholar]
- Presta M, Dell’Era P, Mitola S et al (2005) Fibroblast growth factor/fibroblast growth factor receptor system in angiogenesis. Cytokine Growth Factor Rev 16:159–178. doi:10.1016/j.cytogfr.2005.01.004 [DOI] [PubMed] [Google Scholar]
- Riethdorf S, Reimers N, Assmann V et al (2006) High incidence of EMMPRIN expression in human tumors. Int J Cancer 119:1800–1810. doi:10.1002/ijc.22062 [DOI] [PubMed] [Google Scholar]
- Rubatt JM, Darcy KM, Hutson A et al (2009) Independent prognostic relevance of microvessel density in advanced epithelial ovarian cancer and associations between CD31, CD105, p53 status, and angiogenic marker expression: a gynecologic oncology group study. Gynecol Oncol 112:469–474. doi:10.1016/j.ygyno.2008.11.030 [DOI] [PubMed] [Google Scholar]
- Schauer IG, Sood AK, Mok S, Liu J (2011) Cancer-associated fibroblasts and their putative role in potentiating the initiation and development of epithelial ovarian cancer. Neoplasia 13:393–405. doi:10.1593/neo.101720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schliemann C, Neri D (2007) Antibody-based targeting of the tumor vasculature. Biochim Biophys Acta 1776:175–192. doi:10.1016/j.bbcan.2007.08.002 [DOI] [PubMed] [Google Scholar]
- Seizer P, Borst O, Langer HF et al (2009) EMMPRIN (CD147) is a novel receptor for platelet GPVI and mediates platelet rolling via GPVI-EMMPRIN interaction. Thromb Haemost 101:682–686. doi:10.1160/TH08-06-0368 [DOI] [PubMed] [Google Scholar]
- Sood AK, Fletcher MS, Zahn CM et al (2002) The clinical significance of tumor cell-lined vasculature in ovarian carcinoma: implications for anti-vasculogenic therapy. Cancer Biol Ther 1:661–664 [DOI] [PubMed] [Google Scholar]
- Sun J, Hemler ME (2001) Regulation of MMP-1 and MMP-2 production through CD147/extracellular matrix metalloproteinase inducer interactions. Cancer Res 61:2276–2281 [PubMed] [Google Scholar]
- Tang Y, Nakada MT, Kesavan P et al (2005) Extracellular matrix metalloproteinase inducer stimulates tumor angiogenesis by elevating vascular endothelial cell growth factor and matrix metalloproteinases. Cancer Res 65:3193–3199. doi:10.1158/0008-5472.CAN-04-3605 [DOI] [PubMed] [Google Scholar]
- Tomao F, Papa A, Rossi L et al (2013) Current status of bevacizumab in advanced ovarian cancer. Onco Targets Ther 6:889–899. doi:10.2147/OTT.S46301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda K, Yamada K, Kiyokawa T et al (2012) Pilot study of CD147 protein expression in epithelial ovarian cancer using monoclonal antibody 12C3. J Obstet Gynaecol Res 38:1211–1219. doi:10.1111/j.1447-0756.2012.01853.x [DOI] [PubMed] [Google Scholar]
- Voigt H, Vetter-Kauczok CS, Schrama D et al (2009) CD147 impacts angiogenesis and metastasis formation. Cancer Invest 27:329–333. doi:10.1080/07357900802392675 [DOI] [PubMed] [Google Scholar]
- Weidle UH, Scheuer W, Eggle D et al (2010) Cancer-related issues of CD147. Cancer Genomics Proteomics 7:157–169 [PubMed] [Google Scholar]
- Xing F, Saidou J, Watabe K (2010) Cancer associated fibroblasts (CAFs) in tumor microenvironment. Front Biosci a J virtual Libr 15:166–179. doi:10.2741/3613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Deng L, Li J et al (2013) The prognostic value of vascular endothelial growth factor in ovarian cancer: a systematic review and meta-analysis. Gynecol Oncol 128:391–396. doi:10.1016/j.ygyno.2012.11.002 [DOI] [PubMed] [Google Scholar]
- Zucker S, Hymowitz M, Rollo EE et al (2001) Tumorigenic potential of extracellular matrix metalloproteinase inducer. Am J Pathol 158:1921–1928. doi:10.1016/S0002-9440(10)64660-3 [DOI] [PMC free article] [PubMed] [Google Scholar]