Abstract
English as a Second Language programs serve large foreign-born populations in the US with elevated risks of tuberculosis (TB), yet little is known about TB perceptions in these settings. Using a community-based participatory research approach, we elicited perceptions about TB among immigrant and refugee learners and staff at a diverse adult education center. Community partners were trained in focus groups moderation. Ten focus groups were conducted with 83 learners and staff. Multi-level, team-based qualitative analysis was conducted to develop themes that informed a model of TB perceptions among participants. Multiple challenges with TB control and prevention were identified. There were a variety of mis-perceptions about transmission of TB, and a lack of knowledge about latent TB. Feelings and perceptions related to TB included secrecy, shame, fear, and isolation. Barriers to TB testing include low awareness, lack of knowledge about latent TB, and the practical considerations of transportation, cost, and work schedule conflicts. Barriers to medication use include suspicion of generic medications and perceived side effects. We posit adult education centers with large immigrant and refugee populations as excellent venues for TB prevention, and propose several recommendations for conducting these programs. Content should dispel the most compelling misperceptions about TB transmission while clarifying the difference between active and latent disease. Learners should be educated about TB in the US and that it is curable. Finally, TB programs that include learners and staff in their design and implementation provide greater opportunity for overcoming previously unrecognized barriers.
Keywords: Tuberculosis, Community-based participatory research, Focus groups, Adult education, Immigrants, Refugees
Introduction
The incidence of tuberculosis (TB) infection in the United States has declined over the past decade, but a disparity has emerged whereby infection rates among foreign-born individuals are on the rise. Over half of active TB cases in the US occur in foreign-born individuals [1], and the majority of these cases are due to reactivation of latent tuberculosis infection (LTBI) [2, 3]. The Centers for Disease Control and Prevention (CDC) recommends testing and treating LTBI among foreign-born individuals from countries with a high incidence of TB who have lived in the US for 5 years or less [4]. In spite of this recommendation, LTBI screening of foreign-born individuals is not commonly practiced [5]. Challenges include low health seeking behaviors for screening for latent infection and active disease, as well as suboptimal treatment compliance [4]. The reasons for these barriers may vary by country of emigration and duration of acculturation.
The Health Beliefs Model has been used as a theoretical framework to address TB health behaviors [5–7], whereby an individual's behaviors are explained by perceived susceptibility, severity, barriers to prevention and treatment, and perceived benefits of the same [6]. Sociocultural perceptions are important mediators of these tenets as they pertain to TB among foreign-born individuals [7]. It is therefore, important to understand perceptions of TB across the broad diversity of those foreign-born populations at highest risk. Previous qualitative reports have brought to light critical perceptions and misperceptions of TB among Mexican and Vietnamese immigrants to the US [8–13], which have been used to inform TB control measures. Information from emigrants of other countries is less well known.
Community-based participatory research (CBPR) is a means to collaboratively investigate health topics within a community, whereby community members and academics partner in an equitable relationship [14–16]. CBPR has been particularly successful in identifying and acting to reduce health disparities, as it empowers communities and promotes understanding of culturally pertinent issues [17, 18]. Furthermore, the CDC recommends forging these types of partnerships to eliminate TB in the US [19].
English as a Second Language (ESL) programs seem a logical setting for acquiring a better understanding of perceptions related to TB among new immigrants and refugees to the US In fact, school-based programs have proven to be highly effective locations for TB control among children [20–25], including one ESL program for school age students [26]. Furthermore, while we are aware of no published reports of TB programming at adult education centers, adult ESL programs have been successful venues for educational programming around the topics of hepatitis B [27], cancer screening and prevention [28], and cardiovascular health [29].
Since education at adult education centers is delivered to heterogenous groups of recent immigrants and refugees, it is important to understand collective experiences and perceptions of this group so that TB programming may be most effectively delivered. Therefore, a CBPR approach was engaged to elicit perceived susceptibility and severity of TB, perceived barriers, and perceived benefits of TB prevention among this group of learners and staff.
Methods
Setting
As a constituent of the Rochester Public School District, Hawthorne Education Center (HEC) provides education with an emphasis on literacy to Rochester adults. HEC has evolved into a community center, providing instruction for cultural adjustment, citizenship, and even driver's license training. The Hawthorne Health Service at HEC emerged as a collaborative free clinic and health literacy campaign for adult learners and their families. The clinic is staffed by volunteer physicians and a public health nurse who see patients with health concerns 4 days per week and organize a variety of public health activities through the year, e.g., immunizations, health education, health literacy classes, etc.
The Hawthorne community includes approximately 2,500 learners, 60 staff members, and 250 volunteers each year. Adult learners come predominantly from Sub-Saharan Africa (38%), Latin America (21%), Southeast Asia (17%), and Southeast Minnesota (20%); they speak 70 different languages at home. An estimated 85% live at or below the federal poverty level. Less than half (40%) have completed high school; 12% have never before attended school.
A significant proportion of Hawthorne learners have some of the highest risk characteristics for TB and LTBI in this country, including recent emigration from regions of the world where TB is endemic. The HEC community has experienced several cases of active TB among its students in recent years. Furthermore, 20% of 261 learners and staff who participated in a 2009 pilot TB screening project were found to have LTBI. This disparity contributed to a desire among HEC learners and staff to address the problem among this community of recent immigrants and refugees.
Partnership
In 2006, HEC leadership approached Mayo Clinic faculty who were engaged as volunteers at HEC to work together to address the problem of TB among its learners. Both community and academic partners agreed to adopt a CBPR approach to broadly address health concerns at HEC, and to focus the initial effort on TB. Operating norms were established, monthly meetings were conducted, and a health needs survey was performed. This partnership has grown to include five additional community based organizations, two additional academic centers, and many volunteers to form the Rochester Healthy Community Partnership (RHCP) with a mission of promoting health and well-being among the Rochester population through CBPR, education, and civic engagement to achieve health equity. While RHCP was conducting several health projects, community research capacity and external funding was built around the TB project with the goal of applying the CBPR infrastructure to future health topics. Project partners engaged HEC learners and staff to ensure community involvement in every aspect of the project design and analysis. Once obtained, funding was divided equally between HEC and the academic partner.
Building a Community-Based Qualitative Research Infrastructure
After approval by the Mayo Clinic institutional review board and the Rochester Public School's Office of the Superintendent, a work group was assembled from community and academic partners to address TB at HEC through a CBPR approach.
In early discussions, it became evident that a community-based qualitative research infrastructure was needed to dive deeper into the factors that influence health behaviors related to TB prevention and control, especially among the refugee and immigrant student population. Furthermore, the partnership recognized that it would be important to systematically obtain input from the HEC community through focus groups. A variety of options for conducting focus groups were discussed, but ultimately it was agreed that the infrastructure for focus groups work should come directly from the community. Therefore, a team of community-academic members was assembled to learn focus groups techniques and to build a qualitative research infrastructure for the partnership.
Through established relationships within the CBPR partnership, 28 HEC learners, community members, and academic partners were recruited for qualitative research skills training. Recruitment occurred through direct solicitation of community members. Skills training included a 4 h workshop on the principles of CBPR followed by a 20 h interactive workshop on moderation of focus groups taught by a national focus groups expert (see Acknowledgments).
Research Questions
In early partnership discussions, it became clear that before TB programming could be implemented at the school, learners and staff would have to be systematically interviewed to understand their perceptions about TB. First, the partnership recognized that HEC represents a distinct “community” of individuals bound together by characteristics of low English language literacy and recent immigration from regions of the world where TB is endemic. Since TB education would eventually be targeted to this “community”, it was felt that information gathered from this group as a whole is more valuable than information from subset cultural communities. Next, the Health Beliefs Model was adopted as a literature-based theoretical framework from which to collect information and design programming. The following research questions were then formulated by the RHCP TB work group: (1) What are the perceptions and misperceptions about TB among learners and staff at an adult education center?; (2) How do relationships and social structures influence these perceptions of TB?; (3) What are the perceived barriers and benefits to health seeking behavior for TB? The partnership work group then determined that focus groups with students and staff would be the most optimal means of obtaining this information.
Sampling
In this study, we defined the community as students and staff of HEC. The purpose of the study was introduced to the learners in their classrooms. The learners were then recruited via sign-up sheets in the classrooms and through direct communication with their teachers. Word of mouth likely resulted in a “snowball” sampling within each of the major ethnic groups in the school. Since more learners volunteered for focus groups participation than capacity allowed, the HEC program manager finalized the list of participants to roughly reflect the demographic of the entire student body. HEC staff was invited to participate as focus groups participants as well. The invitation was extended to the entire HEC staff, including teachers, administrative assistants, janitorial staff, etc.
Focus Groups Techniques
Structured focus groups questions were designed by the TB work group and focus groups moderators with edits by adult education specialists familiar with the culture and literacy levels at HEC. Questions were designed to elicit learners' perceptions of TB and perceived barriers to testing and treatment as defined by the Health Beliefs Model. Between October 2008 and January 2009, focus groups facilitators performed ten focus groups with 83 HEC learners and staff. Focus groups were conducted at HEC in a casual setting. Culturally acceptable food was provided to participants. Six focus groups with a total of 54 participants were conducted with learners, and four focus groups with 29 participants were conducted with staff. Focus groups were conducted in English (7), Somali (2), and Spanish (1). One of the focus groups conducted in the Somali language was facilitated by Somali-speaking trained moderators, whereas the other Somali focus groups and the Spanish-language focus group were conducted with real-time translation provided by professional medical interpreters. Following each session, facilitators debriefed with each other to reflect on key moments in the session. Focus groups sessions were digitally recorded, translated to English, and transcribed. Translations were conducted by a single native-language speaking focus group moderator, and translation integrity was verified by at least one other native-language speaking partner.
Thematic Analysis
Each focus groups team created a report with key quotes and themes for each of the questions. An analysis sub-committee of the TB work group was assembled; the board consisted of community and academic partners directly involved in the focus groups planning and moderation, as well as academics with expertise in qualitative analysis. Three members of this committee (M.L.W., S.B., C.S.) used NVIVO-8 software to independently prepare initial coding of all ten focus group transcripts. These individuals held multiple meetings over a period of 2 months, where discrepancies in coding were examined, discussed and debated until consensus was reached between these analysts. The consensus coding structure was used to generate a model of focus groups results conveyed by a series of themes. Themes were organized in the context of the Health Beliefs Model of perceived susceptibility, severity, barriers, and benefits of TB and its treatment and prevention. These themes were then presented to the broader analysis sub-committee through three cycles of meetings and revisions. The consensus model of focus groups results were then presented to the team of focus groups facilitators and to the project work group. Final revisions were made based on feedback from this meeting. The focus groups results were disseminated to HEC students and staff at a World TB Day event in March 2009, which was attended by over 500 learners. Data from HEC learners and staff were analyzed separately and combined.
Results
Sample Characteristics
Demographics of the study sample are displayed in Table 1. The broad diversity of adult learners reflects the demographic of the HEC student body. Likewise, the diverse HEC staff were representative of several occupations, including teachers, administrative assistants, interpreters, volunteers, and janitors. Many of the staff were born in some of the same regions of the world as the dominant student demographics.
Table 1.
Focus groups participants region of birth
| Region of birth | Focus groups with HEC learners (6) | Focus groups with HEC staff (4) | Totals |
|---|---|---|---|
| Africaa | 22 | 6 | 28 |
| Asiab | 11 | 4 | 15 |
| Eastern Europec | 12 | 0 | 12 |
| Latin Americad | 9 | 0 | 9 |
| United States | 0 | 19 | 19 |
| Totals | 54 | 29 | 83 |
Somalia and Sudan
Vietnam, Cambodia, Laos, China, Pakistan
Ukraine, Russia, Turkey
Mexico, Columbia, Puerto Rico
Model of Focus Groups Results
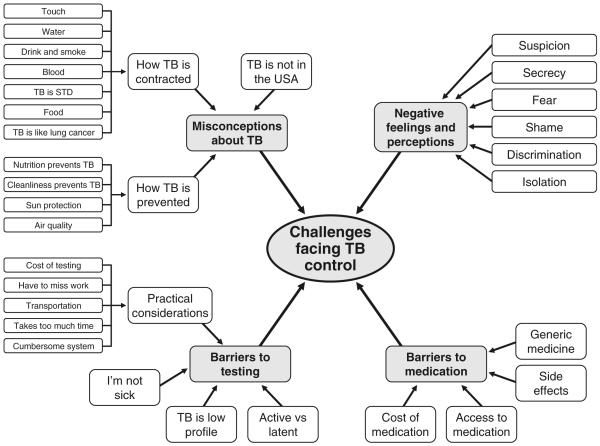
The factors contributing to challenges facing TB control at an adult education center are reflected in Fig. 1. Results to support each theme are conveyed below.
Fig. 1.
Model of challenges facing TB control at an adult education center
Challenges Facing TB control
Misconceptions About TB
One striking observation was the quantity of unsolicited misconceptions about TB. The focus groups moderators did not ask about perceptions of transmission or prevention, but inaccurate statements were proposed 27 times.
One frequently stated misperception was that TB is not present in the United States. One participant stated “I think of (TB as a problem) a long time ago, but not a problem in America anymore.” Another participant from Somalia said “…I don't think Somalis here (in America) have it—maybe people in Africa.”
Focus groups participants often opined about transmission of TB. Theories included transmission by touch, contaminated food or water, blood, sexual contact, and through smoking and drinking alcohol. Furthermore, the most prevalent theories of prevention among participants were through cleanliness, good nutrition, and air pollution control.
Feelings and Perceptions
A number of feelings and perceptions about TB were expressed by adult learners and staff. These feelings are articulated through summaries and quotes highlighted below.
Fear
Fear of the disease and associated repercussions were the most commonly stated feelings regarding TB. This theme was stated in all ten focus groups. Participants expressed three predominant fears about TB. Namely, they feared dying from an incurable disease, spreading the disease to others, and the social isolation that comes from having TB. These fears were often manifestations of experiences with TB in their native countries, where people with TB frequently died or they were taken from their families. In turn, fear is a motivator for many of the subsequent themes identified throughout the focus groups. Representative quotes are as follows:
“It's a killer disease”
“TB is fearful thing. The possibility of going away from the family which take place in other countries. We need to put aside on these fears…So, I think there is fear factor level for several fronts; not just cost but the stigma or the shame or the unknown.”
“I think we need more community education about TB…to remove some of the fear factors.”
Secrecy and Shame
The idea that TB is to be kept secret was brought up in all ten focus groups. Focus groups participants suggested that a diagnosis of TB should be kept secret so that people do not think less of them. Secrecy is thought to be a means to avoid the social isolation that may result from others knowing the diagnosis. Finally, the label of TB seems to carry a level of shame that is disproportionate to other diseases. Representative quotes are as follows:
“In Somalis it (TB) is kept a secret or hidden from others.”
“You have to understand—in our culture (Somali), TB is a very sensitive issue, and a lot of people do not like to talk about it. They do not want to tell people that they have it or they might have had it at one point in their life. They like to be quiet about it. You guys need to understand that first of all.”
“…People don't like TB. They're not willing to come forth and share their ideas about TB because it's a very sensitive issue. It's hard for you guys to understand because it's something that Somali's don't really like to discuss.”
“It (TB) was not talked about. If you get it (then you are) quiet about it because of the fear that he (would be) told leave his family and if there was treatment available it was long track of taking the medication. They rather expose the disease … then go away from the family. You have understood the life expectancy is half in Cambodia than it (is) here. So, it's different perspective but those are things that came with culture that we don't think about.”
”…I also think in some cultures there's taboos about talking about things like whatever word they use for Tuberculosis, what a wasting kind of disease or cancer or something like that.”
Isolation
A feeling that TB is associated with social isolation was a theme that emerged from five of the ten focus groups. There was a significant concern that a diagnosis of TB would uniquely wrench people away from their social ties, both within and outside their family. This perception of isolation was cited as a barrier to seeking care. Furthermore, tensions arose in several focus groups between a tendency to socially isolate those with TB and a perceived religious obligation to embrace those who would be otherwise isolated. Representative quotes are as follows:
“Usually, persons with symptoms of tuberculosis may avoid seeking health care, or use simple cough medicine and sometimes deny their illness to others, because of fear of isolation within the community.”
“It's hard for him (person with TB) because when he tells somebody he has TB, they're going to keep their distance right away. That's what they're going to do. That's one of the reasons he's not comfortable discussing it with anybody.”
“First of all, we are Muslims and our belief is that you're not supposed to run away or isolate someone in need. That's what people should understand. If somebody has TB, it's not like you're better than they. So running away or putting them down or ignoring them is what's making this whole issue worse. It's not helpful. So we have to just realize that just isolating someone is not going to cure anything.”
God's Punishment
Several members of the focus group of Somali women expressed beliefs that TB is considered a punishment for past ill deeds. This view is summarized as follows: “(TB is a) curse or punishment by God for dishonest conducts.”
Barriers to Testing
As recent immigrants or refugees to the US, many focus groups participants meet criteria for LTBI testing. Furthermore, most cases of active TB among foreign-born individuals in the US are secondary to re-activation of LTBI, rather than primary infection. Therefore, questions regarding barriers to testing largely centered around LTBI screening. The following themes emerged from these discussions:
TB is `Low Profile'—Lack of Awareness About TB
Several focus groups brought up the theme that TB is low profile as one reason those who should be tested for TB are not tested. That is, people are not generally aware that TB is a problem or that they should be tested. One participant who meets criteria for TB skin testing conveyed their perception in this way: “…When they do offer free testing or when they do tell us about where you can go to get tested, I think a lot of people are just like `oh, I'm not doing that, I don't know what that is, or TB is not an issue.' Or in my own case, I didn't have it done and I just didn't feel it was important. I don't know why I didn't do it to tell you the truth.”
`I'm Not Sick'—Lack of Knowledge About Latent TB
The barrier to testing identified most often in all of the focus groups stemmed from a lack of knowledge about LTBI. Many focus groups participants did not understand that it is possible to be infected with (latent) TB without having symptoms. When this distinction was demonstrated in the focus groups, participants uniformly cited this lack of knowledge as a primary non-motivator for testing: why would I get tested if I'm not sick? Representative quotes are as follows:
“…if they're talking about something where it's preventive, you know they're not sick, then you know, there's little motivation to do it (TB screening)…”
The problem in our community … is that they don't know the difference between the sleeping one and the active one. The active one almost everyone gets treated for because it's so obvious that your symptoms are just there. But the sleeping one is difficult and people sometimes don't know, and they don't get treated.
Practical Considerations
Several practical considerations were raised in the focus groups regarding ease of testing. These included difficulties with transportation to testing center, testing centers only being open during work hours, testing takes too much time, and cost of testing.
Barriers to Treatment
Barriers to medication compliance for TB were discussed in all of the focus groups. While cost and access to medications came up, most participants were aware of the fact that these medications would be provided free of charge. Therefore, access and costs were not large concerns. The two most common barriers to medication compliance were perceived side effects and suspicion over generic medications. There was no dominant side effect profile that arose as a theme.
Generic medications were discussed at length in one focus group. There was general agreement in that group that the medication(s) used to treat TB were generic, and therefore, not effective. This was summed up by one Somali participant: “(treat with) Not generic medicine, good medicine…Generic's no good medicine.”
Establishing Trust When Talking About TB
All ten focus groups had participants who were willing to share personal experiences on TB. These stories included personal experience with TB testing and treatment for both latent infection and active disease.
Participants indicated that the fact that so many people were willing to speak openly about TB reflects a change in attitude about TB. It was frequently stated that this topic would have been far more taboo in their native countries. Many participants were encouraged and surprised by this openness in the groups. Two representative quotes are as follows:
“At the beginning of this meeting (focus group), we were all hesitant. Nobody wanted to talk about TB or say anything. But when people understand the purpose behind this meeting, they will open up. I was able to tell that I had TB at one point in my life, and I got treated for it. She (pointing to another focus group participant) was able to tell us that she got treated.”
“It's not as difficult to tell someone or influence someone to get tested. Back home it was difficult because when you tell somebody they may have TB they get offended right away. But in this country that's not the case, I mean you have to put your health first and get treatment…So, it's not as difficult as it was back home.”
Differences Between HEC Learners and Staff
Separate analysis of HEC learner and staff responses revealed generally consistent themes between the two groups. Notable exceptions include `practical considerations' regarding barriers to TB testing. Specifically, HEC staff members were far more concerned than the learners about the learners' ability to find transportation to testing centers or pay for the test. On the other hand, themes generated in the `negative feelings and perceptions' (about TB) category were disproportionately represented by the HEC learners.
Discussion
This community-based, participatory study is the first to reveal several important insights into perceptions about TB at an adult ESL education center. Because learners in these programs consist of recent immigrants and refugees from regions of the world where TB is endemic, adult education centers may be particularly effective venues for TB prevention programs in the US. TB remains an area of concern, and misperceptions about TB and negative feelings and emotions about the disease persist among immigrants and refugees to our community. The findings support several practical recommendations for establishment of TB control programs at education centers that serve large foreign-born populations (Table 2).
Table 2.
Recommendations for educational approaches to TB education at an adult education center
| Involve the adult learners in design and implementation of education programs |
| Address the heterogeneity of TB perceptions by providing multiple approaches to TB education |
| Link TB education to community resources for testing and treatment |
| Engage educational content according to perceived susceptibility, severity, barriers and benefits (Table 3) |
Our results conform to the premises of the Health Beliefs Model, and suggest that TB programs may effectively target these domains. Regarding perceived susceptibility, our results suggest that misperceptions about TB transmission should be addressed. The perception that TB is incurable should prompt a call to action for education that TB is treatable and usually curable. Barriers to prevention and treatment should be addressed by recognizing and reflecting feelings and perceptions about TB while educating the population about latent TB and raising awareness that TB exists in the US. Finally, the lack of perceived benefits of prevention and treatment should be addressed through education about latent TB and the implications eradication on personal and community health (Table 3).
Table 3.
The health beliefs model: focus groups results and practice implications for TB programs at an adult education center
| Health beliefs model domains | Focus group results (TB perceptions) | Practice implications (Cues to Action) |
|---|---|---|
| Perceived susceptibility | Misperceptions about TB transmission | Re-enforce modes of transmission |
| Perceived severity | TB is incurable | Reassure that TB is curable |
| Perceived barriers to prevention and treatment | Feelings of fear, secrecy, shame, isolation, discrimination, punishment | Recognize and reflect perceptions and feelings about TB |
| Lack of knowledge about latent TB | Educate about latent TB | |
| Lack of awareness | Raise awareness that TB does exist in the US | |
| Perceived benefits of prevention and treatment | Very little perceived benefit, largely due to lack of knowledge about latent TB and its relationship to illness | Educate about latent TB and implications of eradication for personal and community health |
Focus groups participants asked many unsolicited questions about TB during the session, and they freely stated that attitudes about TB were changing such that the topic could be more openly discussed now than in their home countries or even a few years ago in the United States. Furthermore, many participants were perfectly willing to convey their own stories with TB. While not directly implied from this study, this may indicate that adult learners at these education centers may be ready to learn more about TB. This readiness to learn is a central tenet of successful adult education interventions [30].
The openness of focus groups participants and their willingness to learn may, in part, reflect the participatory process through which the focus groups were planned and conducted. Many of the focus group moderators were community leaders trained in this qualitative technique. The involvement of the HEC students and staff in every phase of the project, and the fact that the focus groups were conducted in the trusted setting of the adult education center may have been additional facilitators of candid discussion. Empowerment of community through CBPR has yielded successful health education and promotion programs across a variety of disciplines [31], and it has been used to address TB control among Aboriginal communities in Canada [32]. This suggests that TB education programs that involve the targeted community in their planning and execution may be particularly successful.
We found that secrecy, shame, fear and isolation were the most prevalent perceptions surrounding TB. A previous study of attitudes towards TB demonstrated increased feelings of stigma among foreign-born individuals compared with the general population [33]. Our findings of specific negative perceptions may help clarify the components of this stigma. Descriptions of TB stigma among East Asian immigrants seemed to be fueled by misperceptions of transmission and disease severity [8, 9]. Likewise, among Mexican immigrants to the US, the stigma and negative perceptions of TB are prevalent, but these negative feelings are attenuated by exposure to TB education [11–13]. This indicates that education programs aimed at the negative perceptions we identified may help to curb stigma associated with this disease.
Our study demonstrated several misconceptions about TB among the mostly foreign-born participants. Consistent with previous studies, we found misperceptions about mechanisms of transmission and severity of TB infection [8]. However, the most prominent misconception among all of the focus groups was a lack of distinction between active disease and LTBI. Downstream effects of this misunderstanding include heightened fear of a diagnosis of LTBI and ambivalence toward TB testing in the absence of symptoms. In fact, the focus groups participants stated that the ambivalence to testing was fed, in part, by a lack of knowledge about this distinction. Therefore, education highlighting the common misperceptions about transmission and severity, but especially the distinction between active disease and latent infection are important for any program attempting to deliver TB information in this setting. This education is particularly important among foreign-born individuals, where most cases of active TB are secondary to reactivation of LTBI [2, 3].
Our study has limitations. First, the application of these descriptive data from a convenience sample of learners at an adult education center may limit applicability of our results in other settings. However, the sample is representative of the student body at this adult education center, and may be representative of other adult education programs across the country that serve immigrant and refugee populations. Second, our sample is derived from a broad diversity of cultures, native languages, and ethnic groups. However, previous research has consistently shown heterogeneous perceptions of TB within individual ethnic groups [8, 12, 13, 34], indicating that heterogeneity of TB perceptions is the norm both within and between groups. This reinforces the fact that multiple types of TB educational interventions are necessary to reach a target population. Third, for those focus groups conducted in English, this was not the native language of most of the participants. This may compromise the interpretation of some responses. Finally, while the analysis team cross-referenced themes with partners from diverse cultural and linguistic backgrounds, interpretation of focus groups results are still based on the analysts' understanding of cultural norms, which may distort the meaning of certain comments.
Conclusions
This community-based participatory research project sheds light on perceptions of TB among a multicultural, mostly immigrant and refugee population while positing adult education centers, particularly those with prominent ESL programming, as promising venues for TB prevention. The findings support several practical recommendations for establishment of TB programs at adult education centers that serve large foreign-born populations. Content should dispel the most compelling misperceptions about TB, reinforce the difference between active TB and latent infection, emphasize that TB does exist in the US, and reassure learners that TB is curable. Furthermore, the approach to TB education at adult education centers should involve the adult learners in the design and implementation of programs while addressing the heterogeneity of TB perceptions by providing multiple approaches to TB education. Finally, education should be directly linked to information about community resources for testing and treatment.
Acknowledgments
The authors would like to thank the HEC learners and staff and community volunteers who participated in this project. The authors also acknowledge with gratitude the role of Richard Krueger, PhD, for his role in training the focus groups facilitators, as well as Kevin Kenny, PhD and Amina Arte for their role in data analysis. Finally, we thank the community focus group moderators for their time and expertise. This project is supported by the National Institutes of Health (NIH) through a Partners in Research grant, R03 AI082703, and by Grant Number 1 UL1 RR024150* from the National Center for Research Resources (NCRR), a component of the NIH, and the NIH Roadmap for Medical Research.
Contributor Information
Mark L. Wieland, Primary Care Internal Medicine, Mayo Clinic College of Medicine, 200 First Street SW, Rochester, MN 55904, USA
Jennifer A. Weis, Research Services: Center for Translational Sciences Activities (CTSA), Mayo Clinic College of Medicine, Rochester, MN, USA
Barbara P. Yawn, Olmsted Medical Center, Rochester, MN, USA
Susan M. Sullivan, Winona State University, Rochester, MN, USA
Kendra L. Millington, Mayo Clinic College of Medicine, Rochester, MN, USA
Christina M. Smith, Behavioral Health Research, Mayo Clinic College of Medicine, Rochester, MN, USA
Susan Bertram, Olmsted Medical Center, Rochester, MN, USA.
Julie A. Nigon, Hawthorne Education Center, Rochester, MN, USA
Irene G. Sia, Infectious Diseases, Mayo Clinic College of Medicine, Rochester, MN, USA
References
- 1.Trends in tuberculosis-United States. MMWR Morb Mortal Wkly Rep 2008. 2007;57(11):281–5. [PubMed] [Google Scholar]
- 2.Cain KP, et al. Tuberculosis among foreign-born persons in the United States: achieving tuberculosis elimination. Am J Respir Crit Care Med. 2007;175(1):75–9. doi: 10.1164/rccm.200608-1178OC. [DOI] [PubMed] [Google Scholar]
- 3.Geng E, et al. Changes in the transmission of tuberculosis in New York City from 1990 to 1999. N Engl J Med. 2002;346(19):1453–8. doi: 10.1056/NEJMoa012972. [DOI] [PubMed] [Google Scholar]
- 4.Taylor Z, Nolan CM, Blumberg HM. Controlling tuberculosis in the United States. Recommendations from the American thoracic society, CDC, and the infectious diseases society of America. MMWR Recomm Rep. 2005;54(RR-12):1–81. [PubMed] [Google Scholar]
- 5.Institute of Medicine . Ending neglect: the elimination of tuberculosis in the United States. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- 6.Rosenstock I. Why people use health services. Millbank Mem Fund Q. 1966;44:94–124. [PubMed] [Google Scholar]
- 7.Rubel AJ, Garro LC. Social and cultural factors in the successful control of tuberculosis. Public Health Rep. 1992;107(6):626–36. [PMC free article] [PubMed] [Google Scholar]
- 8.Joseph HA, et al. TB perspectives among a sample of Mexicans in the United States: results from an ethnographic study. J Immigr Minor Health. 2008;10(2):177–85. doi: 10.1007/s10903-007-9067-5. [DOI] [PubMed] [Google Scholar]
- 9.Carey JW, et al. Tuberculosis beliefs among recent Vietnamese refugees in New York State. Public Health Rep. 1997;112(1):66–72. [PMC free article] [PubMed] [Google Scholar]
- 10.Ito KL. Health culture and the clinical encounter: Vietnamese refugees' responses to preventive drug treatment of inactive tuberculosis. Med Anthropol Q. 1999;13(3):338–64. doi: 10.1525/maq.1999.13.3.338. [DOI] [PubMed] [Google Scholar]
- 11.McEwen MM. Mexican immigrants' explanatory model of latent tuberculosis infection. J Transcult Nurs. 2005;16(4):347–55. doi: 10.1177/1043659605278943. [DOI] [PubMed] [Google Scholar]
- 12.Poss JE. The meanings of tuberculosis for Mexican migrant farmworkers in the United States. Soc Sci Med. 1998;47(2):195–202. doi: 10.1016/s0277-9536(98)00062-8. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Reimann DI, et al. Acculturation and health beliefs of Mexican Americans regarding tuberculosis prevention. J Immigr Health. 2004;6(2):51–62. doi: 10.1023/B:JOIH.0000019165.09266.71. [DOI] [PubMed] [Google Scholar]
- 14.Horowitz CR, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009;119(19):2633–42. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shalowitz MU, et al. Community-based participatory research: a review of the literature with strategies for community engagement. J Dev Behav Pediatr. 2009;30(4):350–61. doi: 10.1097/DBP.0b013e3181b0ef14. [DOI] [PubMed] [Google Scholar]
- 16.Israel BA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 17.Wells K, Jones L. “Research” in community-partnered, participatory research. Jama. 2009;302(3):320–1. doi: 10.1001/jama.2009.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention 2007. Forging partnerships to eliminate tuberculosis: a guide and toolkit. cited; Available from: http://www.cdc.gov/tb/publications/guidestoolkits/for ge/default.htm.
- 20.Chang S, Wheeler LS, Farrell KP. Public health impact of targeted tuberculosis screening in public schools. Am J Public Health. 2002;92(12):1942–5. doi: 10.2105/ajph.92.12.1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohle-Boetani JC, et al. School-based screening for tuberculous infection. A cost-benefit analysis. Jama. 1995;274(8):613–9. [PubMed] [Google Scholar]
- 22.Brassard P, et al. Evaluation of a school-based tuberculosis-screening program and associate investigation targeting recently immigrated children in a low-burden country. Pediatrics. 2006;117(2):e148–56. doi: 10.1542/peds.2005-1534. [DOI] [PubMed] [Google Scholar]
- 23.Barry MA, et al. Tuberculosis infection in urban adolescents: results of a school-based testing program. Am J Public Health. 1990;80(4):439–41. doi: 10.2105/ajph.80.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pong AL, et al. Tuberculosis screening at 2 San Diego high schools with high-risk populations. Arch Pediatr Adolesc Med. 1998;152(7):646–50. doi: 10.1001/archpedi.152.7.646. [DOI] [PubMed] [Google Scholar]
- 25.Sipan C, et al. Screening latino adolescents for latent tuberculosis infection (LTBI) Public Health Rep. 2003;118(5):425–33. doi: 10.1016/S0033-3549(04)50274-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Denison AV, Pierce JR., Jr. Enrollment in english-as-a-second-language class as a predictor of tuberculosis infection in school-children. Public Health Rep. 1996;111(5):428–30. [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor VM, et al. Evaluation of a hepatitis B educational ESL curriculum for Chinese immigrants. Can J Public Health. 2009;100(6):463–6. doi: 10.1007/BF03404345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennett IM, et al. Combining cancer control information with adult literacy education: opportunities to reach adults with limited literacy skills. Cancer Control. 2003;10(5 Suppl):81–3. doi: 10.1177/107327480301005s11. [DOI] [PubMed] [Google Scholar]
- 29.Elder JP, et al. Results of language for health: cardiovascular disease nutrition education for latino English-as-a-second-language students. Health Educ Behav. 2000;27(1):50–63. doi: 10.1177/109019810002700106. [DOI] [PubMed] [Google Scholar]
- 30.Knowles M. The modern practice of adult education: andragogy versus pedagogy. Prentice Hall; Cambridge: 1970. [Google Scholar]
- 31.Viswanathan M, et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess (Summ) 2004;(99):1–8. [PMC free article] [PubMed] [Google Scholar]
- 32.Gibson N, et al. Socio-cultural factors influencing prevention and treatment of tuberculosis in immigrant and aboriginal communities in Canada. Soc Sci Med. 2005;61(5):931–42. doi: 10.1016/j.socscimed.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 33.Marks SM, Deluca N, Walton W. Knowledge, attitudes and risk perceptions about tuberculosis: US national health interview survey. Int J Tuberc Lung Dis. 2008;12(11):1261–7. [PMC free article] [PubMed] [Google Scholar]
- 34.Ailinger RL, et al. Latino immigrants' knowledge of tuberculosis. Public Health Nurs. 2004;21(6):519–23. doi: 10.1111/j.0737-1209.2004.21603.x. [DOI] [PubMed] [Google Scholar]