Abstract
Purpose
To evaluate the personal and professional characteristics associated with career satisfaction and burnout among US oncologists.
Methods
Between October 2012 and March 2013, the American Society of Clinical Oncology conducted a survey of US oncologists evaluating burnout and career satisfaction. The survey sample included equal numbers of men and women and represented all career stages.
Results
Of 2,998 oncologists contacted, 1,490 (49.7%) returned surveys (median age of respondents, 52 years; 49.6% women). Among the 1,117 oncologists (37.3% of overall sample) who completed full-length surveys, 377 (33.8%) were in academic practice (AP) and 482 (43.2%) in private practice (PP), with the remainder in other settings. Oncologists worked an average of 57.6 hours per week (AP, 58.6 hours per week; PP, 62.9 hours per week) and saw a mean of 52 outpatients per week. Overall, 484 oncologists (44.7%) were burned out on the emotional exhaustion and/or depersonalization domain of Maslach Burnout Inventory (AP, 45.9%; PP, 50.5%; P = .18). Hours per week devoted to direct patient care was the dominant professional predictor of burnout for both PP and AP oncologists on univariable and multivariable analyses. Although a majority of oncologists were satisfied with their career (82.5%) and specialty (80.4%) choices, both measures of career satisfaction were lower for those in PP relative to AP (all P < .006).
Conclusion
Overall career satisfaction is high among US oncologists, albeit lower for those in PP relative to AP. Burnout rates among oncologists seem similar to those described in recent studies of US physicians in general. Those oncologists who devote the greatest amount of their professional time to patient care seem to be at greatest risk for burnout.
INTRODUCTION
Although rewarding, caring for patients with cancer is demanding and stressful.1 Oncologists work long hours, supervise the administration of highly toxic therapy, and are continually exposed to death and suffering.1–3 These characteristics place oncologists at risk for burnout, a syndrome characterized by emotional exhaustion, treating people as if they are objects (ie, depersonalization), and loss of meaning or purpose in work.1,4 In addition to potentially profound personal consequences (eg, anxiety, depression, alcohol/substance use, suicide),5–8 burnout among physicians seems to have important professional consequences, including adverse effects on quality of care and professionalism.9–13 Studies also suggest that physicians experiencing burnout are more likely to reduce their work hours and/or pursue early retirement,14 with potential manpower implications for the physician workforce. Although isolated studies have explored burnout in national samples of US oncologists (most recently in 2003),15,16 little is known about personal and professional characteristics associated with burnout and professional satisfaction.1,17,18
METHODS
Participants
A sample of 3,000 oncologists was assembled from the 8,998 US oncologists in the American Society of Clinical Oncology (ASCO; Alexandria, VA) membership file. To ensure adequate representation of oncologists at different career stages and of both sexes, oncologists in the membership file were classified by sex and categorized into three groups according to years in practice (< 10, 10 to 19, and > 20 years). Oncologists were then selected at random to construct a sample evenly distributed by career stage (n = 1,000 from each of career stage category) and sex (1,500 men; 1,500 women).
The 3,000 individuals in the sample were sent an e-mail stating the purpose of the study (eg, to better understand factors contributing to career satisfaction among US oncologists) and providing a link to an electronic survey in October 2012. Three reminder requests were sent over the ensuing 3 weeks. Two individuals sent surveys were deceased, yielding a final sample of 2,998. Individuals not responding to the electronic survey were mailed an identical paper version of the survey in November 2012. Those not responding by January 2013 were sent a brief postcard survey. As an incentive to participate, oncologists who completed the full-length survey received a free ASCO educational product. Participation was voluntary, and all data were deidentified before analysis. ASCO commissioned the study with human subject oversight provided by the Institutional Review Board of the Mayo Clinic (Scottsdale, AZ).
Study Measures
Full-length survey.
The full-length survey included 60 questions exploring a variety of personal and professional characteristics and using standardized instruments to measure burnout and career satisfaction. The full survey is available by request.
Burnout was measured using the Maslach Burnout Inventory (MBI), a 22-item questionnaire considered the gold-standard tool for measuring burnout.4,19–21 The MBI has three subscales to evaluate each domain of burnout: emotional exhaustion, depersonalization, and low personal accomplishment. In the standard scoring for health care workers, physicians with scores ≥ 27 on the emotional exhaustion subscale, ≥ 10 on the depersonalization subscale, or < 33 on the personal accomplishment subscale are considered to have a high degree of burnout in that dimension.4 In keeping with previous studies22–24 and convention,25 we considered physicians with high scores on the depersonalization and/or emotional exhaustion subscales as having at least one manifestation of professional burnout.4 Career satisfaction was assessed using two questions from previous physician surveys regarding career and specialty choice.17,23,26–29
Postcard survey.
To gain insight into participation bias, oncologists not completing the full-length survey were sent a six-question postcard survey that collected information on age, sex, years in practice, and career satisfaction, along with a validated two-item measure of burnout shown to be an accurate proxy measure of burnout.30–32
Statistical Analysis
All full-length and postcard surveys received by March 15, 2013, were included in the analysis. Standard descriptive statistics were used to characterize responding oncologists. Associations between variables were evaluated using the Kruskal-Wallis (continuous variables) or χ2 test (categorical variables) as appropriate. All tests were two sided with type I error rates of 0.05. With the 1,117 responses to the full-length survey, the percentage estimates are accurate to 2.9% with 95% confidence. Comparisons between men and women oncologists were tested using Wilcoxon-Mann-Whitney and Fisher's exact tests. Comparisons with 554 men and 545 women have 80% power to detect an average difference of 17% times the standard deviation, a relatively small effect size.33,34 Multivariable analysis to identify demographic and professional characteristics associated with the dependent outcomes was performed using logistic regression (Appendix, online only). All analyses used SAS software (version 9; SAS Institute, Cary, NC).
RESULTS
Personal and Professional Characteristics
Of 2,998 oncologists who received an invitation to participate, 1,490 (49.7%) responded. Of these, 1,117 oncologists (75.0%) completed the full-length survey (613 electronic; 504 paper version), and 373 (25.0%) completed postcard surveys. Participants were representative of the overall sample with respect to sex; however, early-career oncologists (in practice < 10 years) were somewhat less likely to respond than later-career oncologists (in practice ≥ 20 years). Comparison of full-length survey responders with those completing only the postcard survey (a standard approach for evaluating response bias) did not identify any statistically significant differences with respect to age, sex, years in practice, or satisfaction with specialty choice (Appendix Table A1, online only). Validated single-item measures34,35 of the emotional exhaustion or depersonalization domains of burnout30,31 also failed to identify significant differences. Subsequent analysis focused on participants completing full-length surveys.
The median age of participants was 52 years, with approximately 40% of participants younger than age 50 years (Table 1). Participants were evenly divided by sex. A majority of oncologists (86.2%) were currently married. Independent of relationship status, 86.0% of oncologists reported having children, and nearly half of these oncologists (527; 47.2.%) had a child age ≤ 18 years (ie, school age).
Table 1.
Personal Characteristics for Oncologists in AP Versus PP
| Characteristic | All (N = 1,117) |
AP (n = 377) |
PP* (n = 482) |
P† | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Age, years | |||||||
| Median | 52 | 50 | 52 | .0037 | |||
| Missing | 32 | 10 | 12 | .0380 | |||
| < 40 | 63 | 5.8 | 29 | 7.9 | 24 | 5.1 | |
| 40-49 | 369 | 34.0 | 150 | 40.9 | 161 | 34.3 | |
| 50-59 | 343 | 31.6 | 113 | 30.8 | 165 | 35.1 | |
| ≥ 60 | 310 | 28.6 | 75 | 20.4 | 120 | 25.5 | |
| Sex | < .001 | ||||||
| Missing | 18 | 5 | 3 | ||||
| Male | 554 | 50.4 | 158 | 42.5 | 260 | 54.3 | |
| Female | 545 | 49.6 | 214 | 57.5 | 219 | 45.7 | |
| Children | < .001 | ||||||
| Missing | 17 | 4 | 3 | ||||
| Yes | 946 | 86.0 | 299 | 80.2 | 431 | 90.0 | |
| No | 154 | 14.0 | 74 | 19.8 | 48 | 10.0 | |
| Youngest child age, years | .0532 | ||||||
| Missing | 173 | 79 | 51 | ||||
| < 5 | 119 | 12.6 | 55 | 18.5 | 47 | 10.9 | |
| 5-12 | 249 | 26.4 | 85 | 28.5 | 121 | 28.1 | |
| 13-18 | 159 | 16.8 | 51 | 17.1 | 83 | 19.3 | |
| 19-22 | 106 | 11.2 | 34 | 11.4 | 53 | 12.3 | |
| > 22 | 311 | 32.9 | 73 | 24.5 | 127 | 29.5 | |
| Relationship status | .1721 | ||||||
| Missing | 16 | 3 | 3 | ||||
| Single | 98 | 8.9 | 40 | 10.7 | 32 | 6.7 | |
| Married | 949 | 86.2 | 317 | 84.8 | 427 | 89.1 | |
| Partnered | 34 | 3.1 | 12 | 3.2 | 12 | 2.5 | |
| Widowed/widower | 20 | 1.8 | 5 | 1.3 | 8 | 1.7 | |
| Ever gone through divorce | .1962 | ||||||
| Missing | 20 | 6 | 5 | ||||
| Yes | 193 | 17.6 | 60 | 16.2 | 79 | 16.6 | |
| No | 896 | 81.7 | 310 | 83.6 | 391 | 82.0 | |
| Currently going through one | 8 | 0.7 | 1 | 0.3 | 7 | 1.5 | |
| Current student loan debt | .0742 | ||||||
| Missing | 19 | 2 | 6 | ||||
| No debt | 985 | 89.7 | 324 | 86.4 | 432 | 90.8 | |
| Debt < $25,000 | 26 | 2.4 | 13 | 3.5 | 9 | 1.9 | |
| $25,000-$49,999 | 13 | 1.2 | 9 | 2.4 | 2 | 0.4 | |
| $50,000-$74,999 | 28 | 2.6 | 14 | 3.7 | 11 | 2.3 | |
| $75,000-$99,999 | 16 | 1.5 | 6 | 1.6 | 8 | 1.7 | |
| $100,000-$125,000 | 10 | 0.9 | 2 | 0.5 | 6 | 1.3 | |
| > $125,000 | 20 | 1.8 | 7 | 1.9 | 8 | 1.7 | |
Abbreviations: AP, academic practice; PP, private practice.
Including single-specialty group, multispecialty group, and health maintenance organization.
AP to PP.
With respect to practice setting (Table 2), most oncologists were in private practice (PP; 43.2%) or academic practice (AP; 33.8%), with smaller proportions working at a veterans' hospital, in active military practice, or in other settings. Of the 482 oncologists in PP, 335 (69.5%) were in a single-specialty practice, 124 (25.7.%) a multispecialty practice, and 23 (4.8%) a health maintenance organization (HMO).
Table 2.
Practice Characteristics for AA Versus PP
| Characteristics | All (N = 1,117) |
AP (n = 377) |
PP* (n = 482) |
P† | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Years in practice‡ | |||||||
| Mean | 21.7 | 19.4 | 21.0 | .0262 | |||
| Median | 20.0 | 18.0 | 20.0 | ||||
| < 10 | 148 | 14.5 | 64 | 18.7 | 62 | 13.9 | .0599 |
| 10-19 | 337 | 33.1 | 126 | 36.8 | 152 | 34.0 | |
| ≥ 20 | 533 | 52.4 | 152 | 44.4 | 233 | 52.1 | |
| Practice setting | |||||||
| Academic medical center | 377 | 34.0 | 377 | — | |||
| PP single-specialty group | 335 | 30.2 | — | 335 | 69.5 | ||
| PP multispecialty group | 124 | 11.2 | — | 124 | 25.7 | ||
| PP health maintenance organization | 23 | 2.1 | — | 23 | 4.8 | ||
| Veterans hospital | 20 | 1.8 | — | — | |||
| Active military practice | 2 | 0.2 | — | — | |||
| Industry | 59 | 5.3 | — | — | |||
| Not in practice or retired | 31 | 2.8 | — | — | |||
| Other | 138 | 12.4 | — | — | |||
| Time devoted to patient care, % | < .001 | ||||||
| Missing | 10 | 1 | 2 | ||||
| None | 82 | 7.5 | 3 | .8 | 1 | 0.2 | |
| 1-25 | 94 | 8.6 | 43 | 11.4 | 8 | 1.7 | |
| 26-50 | 121 | 11.0 | 99 | 26.3 | 7 | 1.5 | |
| 51-75 | 199 | 18.0 | 140 | 37.2 | 39 | 8.1 | |
| 76-100 | 611 | 55.2 | 91 | 24.2 | 425 | 88.5 | |
| Focus on specific type cancer | < .001 | ||||||
| Missing | 45 | 11 | 16 | ||||
| Yes | 418 | 39.0 | 295 | 80.6 | 81 | 17.4 | |
| No | 654 | 61.0 | 71 | 19.4 | 385 | 82.6 | |
| Time supervising physicians in training, % | < .001 | ||||||
| Missing | 78 | 25 | 25 | ||||
| 0 | 385 | 37.1 | 9 | 2.6 | 241 | 52.7 | |
| < 5 | 232 | 22.3 | 48 | 13.6 | 141 | 30.9 | |
| 5-10 | 183 | 17.6 | 103 | 29.3 | 56 | 12.3 | |
| 11-20 | 130 | 12.5 | 106 | 30.1 | 12 | 2.6 | |
| > 20 | 109 | 10.5 | 86 | 24.4 | 7 | 1.5 | |
| Hours and call schedule | |||||||
| Median nights on call/week | 1 | 1 | 2 | < .001 | |||
| Hours seeing patients at work/week | < .001 | ||||||
| Mean | 34.0 | 29.2 | 43.4 | ||||
| SD | 17.2 | 14.1 | 11.9 | ||||
| Hours on administrative tasks at work/week | < .001 | ||||||
| Mean | 11.5 | 14.6 | 8.9 | ||||
| SD | 10.5 | 11.0 | 6.9 | ||||
| Hours spent at home on work tasks/week | < .001 | ||||||
| Mean | 8.5 | 10.8 | 7.2 | ||||
| SD | 8.7 | 8.5 | 7.2 | ||||
| Hours at home to keep abreast of developments/week | .4064 | ||||||
| Mean | 4.6 | 4.6 | 4.3 | ||||
| SD | 4.0 | 3.8 | 3.3 | ||||
| Mean total hours/week§ | < .001 | ||||||
| Median | 57.6 | 58.6 | 62.9 | ||||
| SD | 20.8 | 17.7 | 16.2 | ||||
| Outpatient practice | |||||||
| Outpatients in clinic/week | < .001 | ||||||
| Mean | 51.7 | 37.4 | 74.2 | ||||
| SD | 34.6 | 21.0 | 31.0 | ||||
| Minutes allocated/new outpatient | .0011 | ||||||
| Mean | 49.1 | 53.9 | 51.5 | ||||
| SD | 20.3 | 17.0 | 14.8 | ||||
| Minutes allocated/return outpatient | < .001 | ||||||
| Mean | 18.2 | 20.7 | 17.8 | ||||
| SD | 8.2 | 6.8 | 6.1 | ||||
| Hospital practice | |||||||
| Hospital rounding | < .001 | ||||||
| Missing | 45 | 5 | 18 | ||||
| Round own patients when hospitalized | 162 | 15.1 | 20 | 5.4 | 118 | 25.4 | |
| Share rounding with partners in blocks | 171 | 16.0 | 58 | 15.6 | 92 | 19.8 | |
| Share rounding with partners on weekends | 307 | 28.6 | 35 | 9.4 | 218 | 47.0 | |
| Attend oncology teaching service | 249 | 23.2 | 224 | 6.2 | 7 | 1.5 | |
| Do not round in hospital | 183 | 17.1 | 35 | 9.4 | 29 | 6.3 | |
| No. of inpatients on average hospital day | < .001 | ||||||
| Mean | 7.0 | 11.9 | 5.1 | ||||
| SD | 7.3 | 8.1 | 5.3 | ||||
| No. of weekends rounding in hospital/year | < .001 | ||||||
| Mean | 9.8 | 7.2 | 13.0 | ||||
| SD | 9.8 | 5.5 | 10.9 | ||||
| Compensation method | < .001 | ||||||
| Missing | 102 | 25 | 26 | ||||
| Salary no incentive | 336 | 33.1 | 134 | 38.1 | 95 | 20.8 | |
| Salary with bonus | 466 | 45.9 | 207 | 58.8 | 182 | 39.9 | |
| Pure incentive | 213 | 21.0 | 11 | 3.1 | 179 | 39.3 | |
Abbreviations: AP, academic practice; PP, private practice; SD, standard deviation.
Including single-specialty group, multispecialty group, and health maintenance organization.
Comparison of AP to PP.
Since completion of fellowship training.
Sum of above four categories.
Oncologists spent 57.6 hours per week devoted to professional activities, including an average of 34.0 hours per week on direct patient care, 11.5 hours per week on administrative tasks at work, and 8.5 hours per week performing work tasks at home (completing paperwork, preparing talks, writing grants/manuscripts, and so on), plus 4.6 hours per week keeping abreast of developments in the field and maintenance of certification. On average, oncologists cared for 52 patients in the outpatient setting each week.
Comparison of PP and AP
Extensive differences in both demographic and practice characteristics were observed between PP and AP oncologists (Tables 1 and 2). Oncologists working in AP settings were slightly younger (median age, 50 v 52 years; P = .0037), more likely to be women (57.5% v 45.7%; P < .001), and less likely to have children (80.2% v 90.0%; P < .001). On average, oncologists in AP worked 4.3 fewer hours each week (58.6 v 62.9 hours; P < .001) and devoted less professional effort to direct patient care, with 38.5% in AP spending ≤ 50% of their effort on patient care compared with 3.4% in PP. Oncologists in AP were more likely to focus on treating patients with one specific type of cancer (80.6% v 17.4%; P < .001) and spent a greater proportion of their time supervising physicians in training.
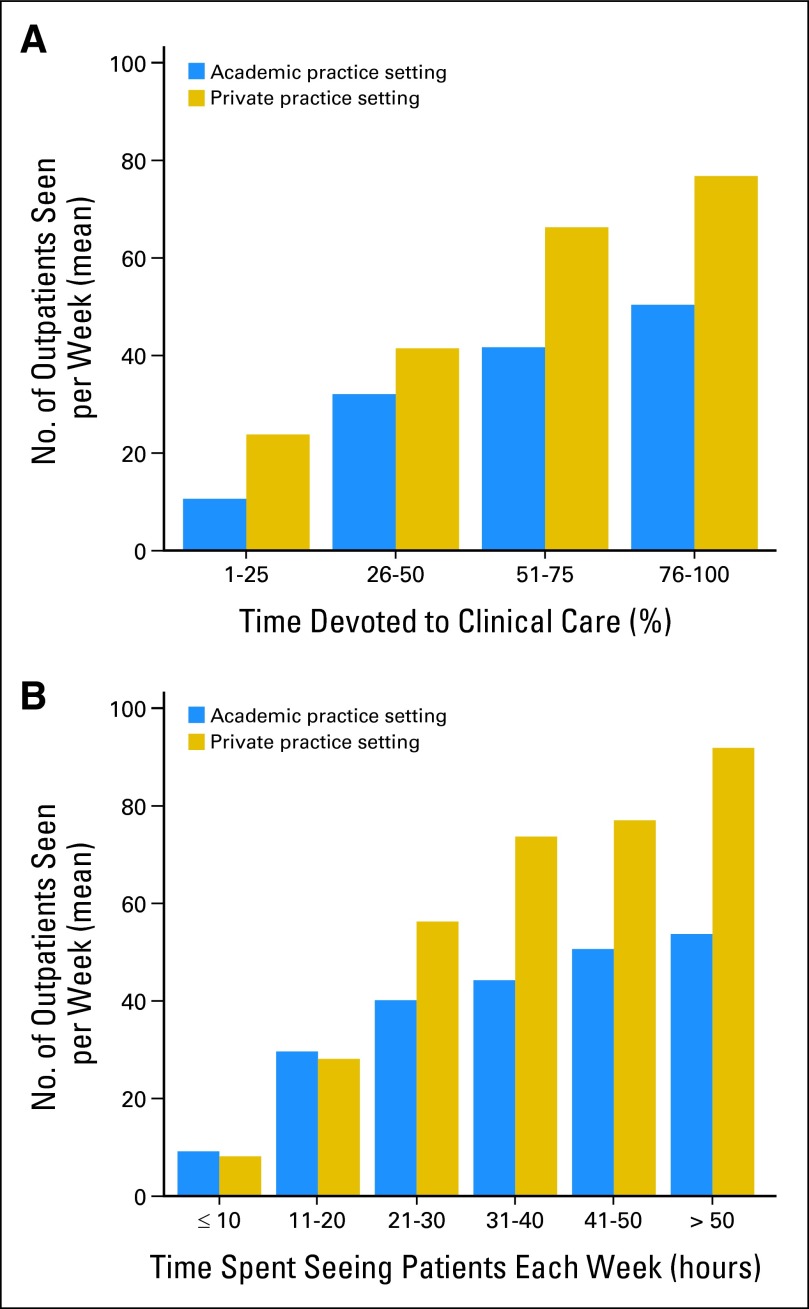
Oncologists in PP saw nearly twice as many patients each week, on average, as those in AP (74.2 v 37.4; P < .001). Despite the difference in the total number of patients seen per week, the amount of time allocated for each new patient (PP, 52 minutes; AP, 54 minutes; P = .0011) and return patient (PP, 18 minutes; AP, 21 minutes; P < .001) differed only slightly. The relationship between the number of patients seen per week and percentage of professional effort devoted to clinical care and the number of hours devoted to patient care each week is shown in Figures 1A and 1B.
Fig 1.
Hours and effort devoted to clinical care and patients seen per week. The relationship between the number of outpatients seen per week (y-axis) and (A) percentage of effort devoted to clinical care or (B) hours spent seeing patients each week on x-axis.
The method of compensation differed for AP compared with PP, with a larger proportion of PP oncologists in a purely incentive-based model (PP, 39.3% v AP, 3.1%; P < .001) and fewer in a salary-only (PP, 20.8% v AP, 38.1%; P < .001) or salary–plus–productivity bonus model (PP, 39.9% v AP, 58.8%; P < .001). PP oncologists were more likely to report a > 10% decline in compensation in 2012 relative to 2011 (PP, 35.2% v AP, 8.0%; P < .001). Other differences between PP and AP are summarized in Table 2. A subanalysis of PP oncologists according to practice setting (ie, single specialty, multispecialty, HMO) can be found in Appendix Tables A2 and A3 (online only).
Oncologist Well-Being
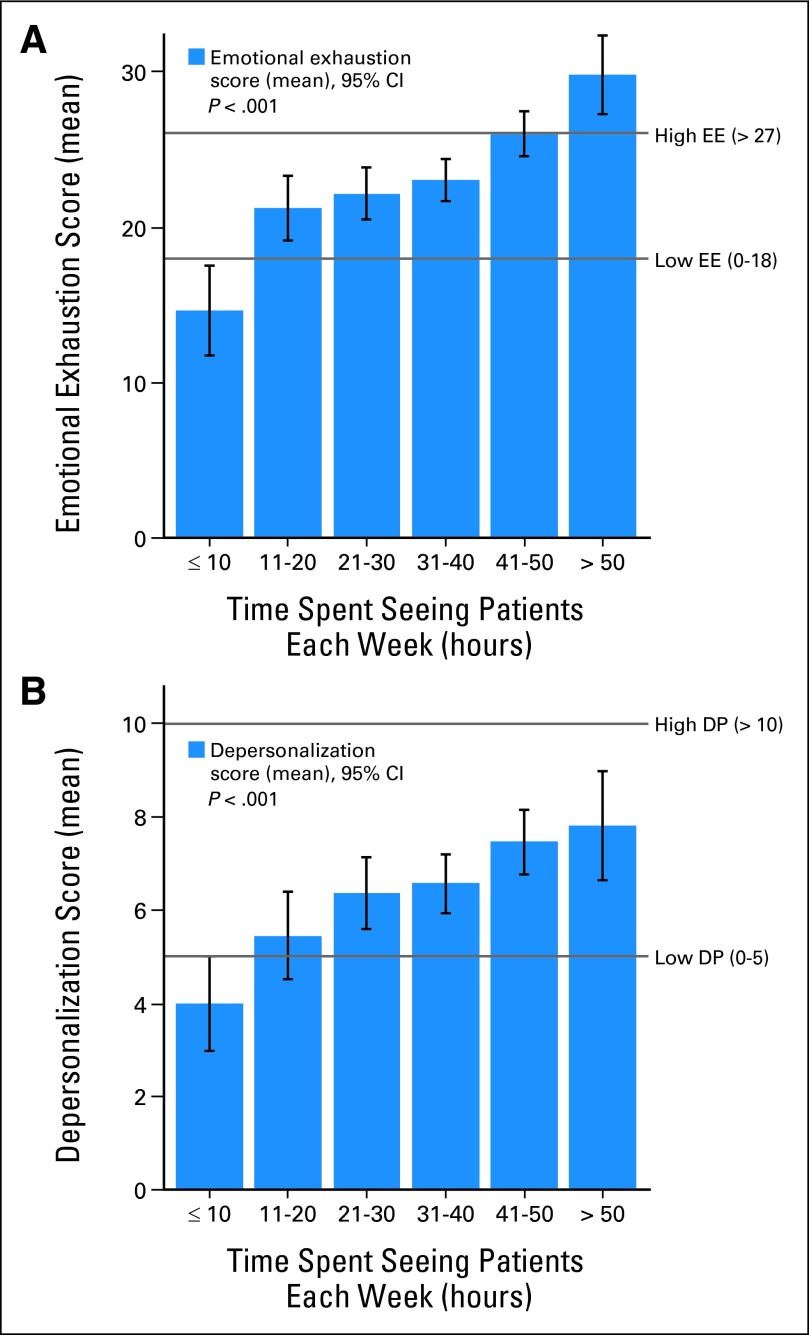
Table 3 summarizes burnout, fatigue, and career satisfaction among participating oncologists. When assessed using the full MBI, 38.3% of oncologists had high emotional exhaustion, 24.9% had high depersonalization, and 13.2% had a low sense of personal accomplishment. In aggregate, 44.7% of oncologists had at least one symptom of burnout (high emotional exhaustion score and/or high depersonalization). Demographic characteristics associated with burnout on univariable analysis included younger age, being a woman, relationship status, not having children, and greater student loan debt (Appendix Table A4, online only). Professional characteristics associated with burnout on univariable analysis (Appendix Table A5, online only) included hours worked per week, number of hours spent seeing patients per week (Figs 2A and 2B), devoting more time to patient care, seeing a larger number of patients per week, and method of compensation (burnout rates: salary only, 40.7%; salary with bonus, 47.1%; pure incentive, 53.8%; P = .011). Although oncologists in PP had higher median emotional exhaustion and depersonalization scores than did those in AP, no difference in the overall burnout rate was observed by practice setting (PP, 50.5% v AP, 45.9%; P = .177). A subanalysis of well-being among PP oncologists based on practice setting can be found in Appendix Table A6 (online only).
Table 3.
Career Satisfaction and Burnout
| Characteristic | All (N = 1,117) |
AP (n = 377) |
PP (n = 482) |
P | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Burnout indices* | |||||||
| Emotional exhaustion† | |||||||
| Median | 22 | 22 | 24 | .0895 | |||
| Low score | 433 | 40.1 | 146 | 39.0 | 157 | 33.0 | .1798 |
| Intermediate score | 233 | 21.6 | 78 | 20.9 | 113 | 23.7 | |
| High score | 413 | 38.3 | 150 | 40.1 | 206 | 43.3 | |
| Depersonalization† | |||||||
| Median | 5 | 5 | 6 | .0124 | |||
| Low score | 558 | 52.3 | 191 | 51.3 | 220 | 46.1 | .0165 |
| Intermediate score | 243 | 22.8 | 99 | 26.6 | 110 | 23.1 | |
| High score | 265 | 24.9 | 82 | 22.0 | 147 | 30.8 | |
| Personal accomplishment | |||||||
| Median | 42 | 41 | 42 | .0415 | |||
| High score | 660 | 63.0 | 225 | 61.0 | 304 | 64.0 | .3109 |
| Intermediate score | 249 | 23.8 | 89 | 24.1 | 117 | 24.6 | |
| Low score‡ | 138 | 13.2 | 55 | 14.9 | 54 | 11.4 | |
| Burned out§ | 484 | 44.7 | 172 | 45.9 | 241 | 50.5 | .1769 |
| Career satisfaction | |||||||
| Would become physician again (career choice) | 908 | 82.5 | 328 | 87.5 | 378 | 79.2 | .0016 |
| Would become oncologist again (specialty choice) | 877 | 80.5 | 314 | 85.1 | 368 | 77.5 | .0053 |
Abbreviations: AP, academic practice; MBI, Maslach Burnout Inventory; PP, private practice.
As assessed using the full MBI.
Per the standard scoring of the MBI for health care workers, physicians with scores ≥ 27 on the emotional exhaustion subscale, ≥ 10 on the depersonalization subscale, or < 33 on the personal accomplishment subscale are considered to have a high degree of burnout in that dimension.
Low scores on the personal accomplishment subscale are less favorable.
High score on emotional exhaustion and/or depersonalization subscales of the MBI (see Methods).
Fig 2.
Patient care activity and burnout. The relationship between patient care hours devoted to patient care and burnout among the 985 oncologists who completed the full-length survey and provided information on both hours and burnout is shown. The number of hours spent seeing patients each week is shown on the x-axis. Mean burnout score in the (A) emotional exhaustion (EE) and (B) depersonalization (DP) domains is shown in the y-axis. Horizontal lines indicate the standardized thresholds to categorize scores for physicians as low, intermediate, or high degree of burnout according to the Maslach Burnout Inventory.
A majority of oncologists indicated they would choose to become a physician (82.5%) and oncologist (80.5%) again if they could revisit their career and specialty choices. Career satisfaction, as measured by these items, was higher for oncologists in AP than PP (Table 3).
Multivariable Analysis
We performed multivariable analysis to identify personal and professional characteristics associated with burnout and career satisfaction. In addition to an overall model, separate models were developed by practice setting because of the profound differences in personal and professional characteristics of oncologists in PP and AP (Table 4). Younger age and greater number of hours spent seeing patients each week were independently associated with burnout in all models. Each year older reduced the risk of burnout by approximately 4% to 5% (eg, 10 years older, 40% to 50% lower risk), whereas each additional hour spent seeing patients each week increased the risk of burnout by approximately 2% to 4% (eg, 20% to 40% higher risk for each additional 10 hours). In the overall model, each additional hour per week spent on work-related tasks while at home also increased the risk of burnout by approximately 2% (eg, 10% higher risk for each additional 5 hours per week), and focusing on a specific type of cancer increased the risk of burnout by approximately 40%.
Table 4.
Factors Associated With Burnout on Multivariable Analysis
| Predictors | OR | 95% CI | P |
|---|---|---|---|
| All oncologists*†‡ | |||
| Age (for each additional year older) | 0.961 | 0.947 to 0.975 | < .001 |
| Hours/week spent seeing patients (OR each additional hour) | 1.032 | 1.022 to 1.042 | < .001 |
| Hours/week at home spent on work tasks (OR each additional hour) | 1.019 | 1.001 to 1.037 | .0392 |
| Focus on one certain type of cancer (v multiple focus) | 1.422 | 1.050 to 1.925 | .0227 |
| Private practice*†§ | |||
| Age (OR each additional year older) | 0.953 | 0.932 to 0.974 | < .001 |
| Has children (v not) | 0.447 | 0.210 to 0.950 | .0363 |
| Hours/week spent seeing patients (OR each additional hour) | 1.041 | 1.020 to 1.063 | < .001 |
| Hours/week spent administrative tasks at work/week (OR each additional hour) | 1.054 | 1.018 to 1.092 | .0032 |
| Nights on call/week (OR each additional night) | 0.877 | 0.788 to 0.975 | .0152 |
| Academic practice*†‖ | |||
| Age (OR each additional year older) | 0.961 | 0.935 to 0.987 | .0036 |
| Female (v male) | 1.678 | 1.020 to 2.762 | .0416 |
| Hours/week spent seeing patients (OR each additional hour) | 1.023 | 1.004 to 1.042 | .0190 |
| Hours/week spent at home on work tasks (OR each additional hour) | 1.035 | 1.002 to 1.069 | .0363 |
| Minutes allotted for a return outpatient appointment (OR each additional minute) | 0.964 | 0.929 to 1.000 | .0494 |
| No. of weekends on call/year (for each additional weekend) | 1.071 | 1.015 to 1.130 | .0122 |
| Focus on one certain type of cancer (v multiple focus) | 3.244 | 1.556 to 6.673 | .0017 |
NOTE. Three multivariable analyses were conducted to identify personal and professional factors associated with burnout. The first model included all oncologists. Given substantial differences in professional characteristics, separate models were also created for PP oncologists and AP oncologists.
Abbreviations: AP, academic practice; OR, odds ratio; PP, private practice.
Personal characteristics in all models: age, sex, children, youngest child, relationship status, and student loan debt.
Professional characteristics in all models: hours spent seeing patients/week, hours spent on administrative tasks/week, hours spent working at home performing work tasks/week, No. of nights on call per week, No. of outpatients seen/week, focus on certain type of cancer (yes/no), minutes allocated per new outpatient visit, minutes allocated per return outpatient visit, No. of weekends rounding in hospital/year, and method compensation (salary, salary plus bonus, pure incentive).
Additional professional characteristics in all oncologist models: practice setting.
Additional professional characteristics in PP model: practice setting (single specialty, multispecialty, health maintenance organization).
Additional professional characteristics in AP model: percentage of time spent supervising physicians in training.
Risks specific to practice setting were also observed. Having children was associated with an approximately 55% decreased risk of burnout among PP oncologists (odds ratio [OR], 0.45) but was not a significant factor for oncologists in AP. In contrast, being a woman was associated with an approximately 65% increased risk of burnout among oncologists in AP (OR, 1.68) but was not a significant factor for oncologists in PP. Each additional hour per week spent on administrative tasks at work increased risk of burnout by approximately 5% among PP oncologists (eg, 5 more hours per week, approximately 25% higher risk), whereas each additional hour per week spent on work tasks at home increased risk by approximately 3.5% among AP oncologists (eg, 5 more hours per week, approximately 17.5% higher risk). Among AP oncologists, focusing on one type of cancer was associated with an increased risk of burnout of 320% (OR, 3.24). For those in AP, having less time allocated for each return patient visit (return slots of 20 minutes in length had a 36% increased risk of burnout compared with return slots of 30 minutes in length) and each additional weekend on call per year also increased risk of burnout.
DISCUSSION
This is the first national study of US oncologists evaluating burnout and career satisfaction to our knowledge since 2003 and is the only national study to our knowledge to evaluate burnout in US oncologists using standardized instruments. Approximately 45% of oncologists had at least one symptom of burnout at the time of the survey. Although burnout was strongly related to a variety of personal characteristics on univariate analysis, younger age was the only demographic factor independently associated with risk on multivariable analysis adjusting for professional characteristics. In contrast, a variety of professional characteristics were independently associated with burnout. Hours per week devoted to direct patient care was the dominant professional factor associated with burnout. The number of hours per week spent performing work tasks at home and focusing clinical practice on a specific type of cancer were also independently associated with burnout risk.
The strong, incremental relationship between time devoted to patient care and burnout is concerning, especially given the projected shortage in the supply of oncologists during the coming decades. Medical oncologists already work more hours than physicians in most other disciplines.35 Reducing clinical work hours or the volume of patients seen may be a strategy to decrease burnout for individual oncologists but at the societal level could exacerbate the projected oncologist workforce shortage.1,14 The findings also suggest that productivity-based compensation models designed to increase the volume of care oncologists provide are associated with higher burnout and may be self-defeating in the long run.
Although the qualitative differences in AP and PP are recognized, the data collected here provide granular information about these differences and explore associations with burnout and career satisfaction. Oncologists in AP were younger, more likely to be women, and less likely to have children. Oncologists in PP saw nearly twice as many patients each week, were more likely to be compensated in a purely incentive-based model, and were less likely to focus their practice on a specific area of oncology. AP oncologists spent far more time on work tasks when at home and dedicated more of their effort to supervising physicians in training. Although no difference in the overall prevalence of burnout was observed by practice setting on multivariable analysis, many of the risk factors for burnout differed between AP and PP oncologists, suggesting that efforts to reduce burnout will need to be tailored to practice setting.
How does the prevalence of burnout among US oncologists compare with that among US adults and physicians in other specialties? A recent national study exploring the prevalence of physician burnout found that approximately 46% of US physicians were experiencing symptoms of burnout at the time of the study and that the rate of burnout was markedly higher in physicians than in a probability-based sample of US workers.32 Although a subanalysis from that study suggested oncologists may actually have a lower rate of burnout (prevalence of approximately 38%) than other internal medicine physicians, only 87 medical oncologists were included in that analysis.1 The prevalence of burnout (approximately 45%) in our sample of more than 1,000 oncologists was similar to that of US physicians overall. It was also consistent with rates observed in other internal medicine subspecialists (approximately 44%) and lower than rates in general internists (approximately 54%).32 Notably, satisfaction with career and specialty choice among oncologists in our study (both > 80%) were the highest of any group of physicians we have studied.26,32,36,37
How do these findings compare with those of previous studies of oncologists? In 1990, Whippen et al15 sent a 12-item survey with a single question about burnout to 1,000 oncologists who subscribed to Journal of Clinical Oncology. Among the 598 respondents, 56% subjectively reported that they felt burned out. In 2003, Allegra et al16 administered a similar survey to approximately 7,700 US oncologists. Among the 1,740 (23%) who responded, 61.7% endorsed a yes/no question asking, “Do you feel that you are experiencing any signs of burnout?” These historical studies are difficult to interpret because they did not use standardized metrics to assess burnout. The prevalence of high emotional exhaustion (22% to 53%) and high depersonalization (11% to 30%) as measured by the MBI in studies of oncologists from other countries are consistent with the rates of emotional exhaustion (38.3%) and depersonalization (24.9%) observed in our study.3,38–41
Our study is subject to a number of limitations. Although our participation rate of approximately 50% is consistent with42 or even higher than 26,32,36 physician surveys in general, response bias remains a possibility. We found no statistically significant differences with respect to age, sex, years in practice, or career satisfaction among oncologists who completed the postcard survey, further supporting that responders were representative of US oncologists. It should be noted that several previous cross-sectional studies have failed to identify significant differences between responding and nonresponding physicians.43 Because our survey was cross-sectional, we were unable to determine causality or the potential direction of effect for the associations observed. A survival bias may account for some associations such as age (ie, unsatisfied people leave the field). Although we were able to compare differences between oncologists in PP and AP, there were too few participants working in other practice settings to make meaningful comparisons.
Our study also has several important strengths. The oncologists in the sample were drawn from the ASCO oncologist registry, a comprehensive list of US oncologists. The survey included oncologists from all career stages and practice types, as well as a large sample of female oncologists. Our mixed-methods survey design (ie, electronic survey, full-length paper survey, postcard survey) led to a high participation rate relative to other national studies of physicians.16,26,36 The survey collected extensive information on personal and practice characteristics, providing granular insights into relationships among these variables and burnout/career satisfaction.
Given the prevalence of burnout and evidence that it erodes physicians' personal health6,7,44 and the quality of care they provide,9–11,45–50 future studies need to focus on how to address this problem. There is currently limited evidence on what interventions reduce the risk of burnout; most available information focuses on individual17,18,51–53 rather than system approaches.5,54 The high prevalence of burnout suggests that studies evaluating practice models (team-based care) and structural characteristics in the practice environment that may reduce burnout are needed.
In conclusion, the prevalence of burnout among US oncologists seems similar to or lower than that of physicians in other disciplines. Although approximately 45% of oncologists are experiencing burnout, their career and specialty satisfaction are high. The volume of patient care provided seems to be a dominant contributor to burnout for both AP and PP oncologists; however, a number of other contributing factors seem to differ by practice setting. A better understanding of the factors that sustain career satisfaction and studies testing interventions to reduce oncologist burnout are needed.
Appendix
Multivariable Analysis
Predictors included in the logistic model of all oncologists were age, sex, parental status, age of youngest child, relationship status, student loan debt, hours spent per week seeing patients, hours spent per week on administrative tasks, hours spent working at home per week, number of nights on call per week, number of outpatients seen per week, whether oncologist focused on one specific type of cancer, minutes allocated to a new outpatient visit, minutes allocated to a return outpatient visit, number of weekends spent on rounds in hospital per year, method of compensation, and practice setting. The logistic model for private practice oncologists included type of private setting (eg, health maintenance organization, single specialty, multispecialty). The logistic model for academic practice oncologists included percentage of time dedicated to supervising physicians in training.
Table A1.
Comparison of Oncologists Who Completed Full-Length With Those Who Completed Postcard Surveys
| Characteristic | Full-Length Survey (n = 1,117) |
Postcard Survey (n = 373) |
P | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Median age, years | 52 | 52 | .8693 | ||
| < 40 | 63 | 5.8 | 18 | 4.9 | .8453 |
| 40-49 | 369 | 34.0 | 132 | 36.1 | |
| 50-59 | 343 | 31.6 | 115 | 31.4 | |
| ≥ 60 | 310 | 28.6 | 101 | 27.6 | |
| Sex | .3017 | ||||
| Male | 554 | 50.4 | 176 | 47.3 | |
| Female | 545 | 49.6 | 196 | 52.7 | |
| Years in practice | |||||
| Median | 20 | 19 | .6753 | ||
| < 10 | 148 | 14.5 | 61 | 16.4 | .5950 |
| 10-19 | 337 | 33.1 | 126 | 33.9 | |
| ≥ 20 | 533 | 52.4 | 185 | 49.7 | |
| Would become oncologist again | .9028 | ||||
| Definitely not | 30 | 2.8 | 11 | 2.9 | |
| Probably not | 77 | 7.1 | 27 | 7.2 | |
| Neutral | 105 | 9.6 | 37 | 9.9 | |
| Probably | 316 | 29.0 | 98 | 26.3 | |
| Definitely yes | 561 | 51.5 | 200 | 53.6 | |
| EE*† | .2930 | ||||
| Never | 157 | 14.5 | 46 | 12.4 | |
| A few times a year | 286 | 26.4 | 100 | 27.0 | |
| Once a month or less | 149 | 13.8 | 60 | 16.2 | |
| A few times a month | 174 | 16.1 | 73 | 19.7 | |
| Once a week | 108 | 10.0 | 29 | 7.8 | |
| A few times a week | 131 | 12.1 | 44 | 11.9 | |
| Every day | 78 | 7.2 | 19 | 5.1 | |
| DP*‡ | .2936 | ||||
| Never | 439 | 40.8 | 154 | 41.3 | |
| A few times a year | 301 | 28.0 | 120 | 32.2 | |
| Once a month or less | 109 | 10.1 | 28 | 7.5 | |
| A few times a month | 83 | 7.7 | 33 | 8.8 | |
| Once a week | 65 | 6.0 | 14 | 3.8 | |
| A few times a week | 70 | 6.5 | 22 | 5.9 | |
| Every day | 9 | 0.8 | 2 | 0.5 | |
Abbreviations: DP, depersonalization; EE, emotional exhaustion; MBI, Maslach Burnout Inventory; ROC, receiver operating characteristic.
As assessed using the single-item measures for EE and DP adapted from the full MBI. Area under the ROC curve for the EE and DP single items relative to that of their respective full MBI domain scores in previous studies were 0.94 and 0.93 and the positive predictive values of the single-item thresholds for high levels of EE and DP were 88.2% and 89.6%, respectively.30,31
Individuals indicating symptoms of EE weekly or more often have median EE scores of > 30 on the full MBI and have a > 75% probability of having a high EE score as defined by the MBI (≥ 27).
Individuals indicating symptoms of DP weekly or more often have median DP scores on the full MBI of > 13 and have a > 85% probability of having a high DP score as defined by the MBI (≥ 10).
Table A2.
Personal Characteristics Among Different PP Settings
| Characteristic | Single Specialty (n = 335) |
Multispecialty (N = 124) |
HMO (n = 23) |
P | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Age, years | |||||||
| Median | 52.5 | 52.0 | 50.0 | .1222 | |||
| Missing | 6 | 5 | 1 | .0505 | |||
| < 40 | 10 | 3.0 | 12 | 10.1 | 2 | 9.1 | |
| 40-49 | 114 | 34.7 | 39 | 32.8 | 8 | 36.4 | |
| 50-59 | 113 | 34.3 | 43 | 36.1 | 9 | 40.9 | |
| ≥ 60 | 92 | 28.0 | 25 | 21.0 | 3 | 13.6 | |
| Sex | .0070 | ||||||
| Missing | 1 | 1 | 1 | ||||
| Male | 194 | 58.1 | 60 | 48.8 | 6 | 27.3 | |
| Female | 140 | 41.9 | 63 | 51.2 | 16 | 72.7 | |
| Children | .3329 | ||||||
| Missing | 1 | 1 | 1 | ||||
| Yes | 305 | 91.3 | 107 | 87.0 | 19 | 86.4 | |
| No | 29 | 8.7 | 16 | 13.0 | 3 | 13.6 | |
| Age of youngest child, years | .4001 | ||||||
| Missing | 30 | 17 | 4 | ||||
| < 5 | 27 | 8.9 | 18 | 16.8 | 2 | 10.5 | |
| 5-12 | 86 | 28.2 | 29 | 27.1 | 6 | 31.6 | |
| 13-18 | 58 | 19.0 | 21 | 19.6 | 4 | 21.1 | |
| 19-22 | 38 | 12.5 | 11 | 10.3 | 4 | 21.1 | |
| > 22 | 96 | 31.5 | 28 | 26.2 | 3 | 15.8 | |
| Relationship status | .4851 | ||||||
| Missing | 1 | 1 | 1 | ||||
| Single | 20 | 6.0 | 10 | 8.1 | 2 | 9.1 | |
| Married | 302 | 90.4 | 105 | 85.4 | 20 | 90.9 | |
| Partnered | 6 | 1.8 | 6 | 4.9 | 0 | 0.0 | |
| Widowed/widower | 6 | 1.8 | 2 | 1.6 | 0 | 0.0 | |
| Ever gone through divorce | .8326 | ||||||
| Missing | 3 | 1 | 1 | ||||
| Yes | 55 | 16.6 | 22 | 17.9 | 2 | 9.1 | |
| No | 272 | 81.9 | 99 | 80.5 | 20 | 90.9 | |
| Currently going through one | 5 | 1.5 | 2 | 1.6 | 0 | 0.0 | |
| Current student loan debt | .3009 | ||||||
| Missing | 4 | 1 | 1 | ||||
| No debt | 304 | 91.8 | 108 | 87.8 | 20 | 90.9 | |
| Debt < $25,000 | 6 | 1.8 | 3 | 2.4 | 0 | 0.0 | |
| $25,000-$49,999 | 1 | 0.3 | 1 | 0.8 | 0 | 0.0 | |
| $50,000-$74,999 | 8 | 2.4 | 1 | 0.8 | 2 | 9.1 | |
| $75,000-$99,999 | 5 | 1.5 | 3 | 2.4 | 0 | 0.0 | |
| $100,000-$125,000 | 4 | 1.2 | 2 | 1.6 | 0 | 0.0 | |
| > $125,000 | 3 | 0.9 | 5 | 4.1 | 0 | 0.0 | |
Abbreviations: HMO, health maintenance organization; PP, private practice.
Table A3.
Comparison of Practice Characteristics Among Different PP* Settings
| Characteristic | Single Specialty (n = 335) |
Multispecialty (n = 124) |
HMO (n = 23) |
P | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Mean years in practice | 21.7 | 19.5 | 18.8 | .1131 | |||
| General | |||||||
| Time devoted to patient care, % | .5415 | ||||||
| Missing | 2 | 0 | 0 | ||||
| None | 0 | 0.0 | 1 | 0.8 | 0 | 0.0 | |
| 1-25 | 4 | 1.2 | 3 | 2.4 | 1 | 4.3 | |
| 26-50 | 4 | 1.2 | 2 | 1.6 | 1 | 4.3 | |
| 51-75 | 26 | 7.8 | 12 | 9.7 | 1 | 4.3 | |
| 76-100 | 299 | 89.8 | 106 | 85.5 | 20 | 87.0 | |
| Focus on specific type cancer | .3162 | ||||||
| Missing | 12 | 4 | 0 | ||||
| Yes | 54 | 16.7 | 25 | 20.8 | 2 | 8.7 | |
| No | 269 | 83.3 | 95 | 79.2 | 21 | 91.3 | |
| Time supervising physicians in training, % | .5871 | ||||||
| Missing | 19 | 5 | 1 | ||||
| 0 | 166 | 52.5 | 63 | 52.9 | 12 | 54.5 | |
| < 5 | 101 | 32.0 | 36 | 30.3 | 4 | 18.2 | |
| 5-10 | 38 | 12.0 | 15 | 12.6 | 3 | 13.6 | |
| 11-20 | 7 | 2.2 | 3 | 2.5 | 2 | 9.1 | |
| > 20 | 4 | 1.3 | 2 | 1.7 | 1 | 4.5 | |
| Hours and call schedule | |||||||
| Median nights on call/week | 2 | 2 | 1 | .0309 | |||
| Hours spent seeing patients at work/week | .4721 | ||||||
| Mean | 43.7 | 43.1 | 40.7 | ||||
| SD | 11.7 | 12.7 | 10.0 | ||||
| Hours spent on administrative tasks at work/week | .5956 | ||||||
| Mean | 8.9 | 8.9 | 7.8 | ||||
| SD | 7.0 | 6.6 | 6.9 | ||||
| Hours spent at home on work tasks/week | .3192 | ||||||
| Mean | 7.3 | 7.0 | 6.0 | ||||
| SD | 7.6 | 6.1 | 7.7 | ||||
| Hours spent at home to keep abreast of developments/week | .2431 | ||||||
| Mean | 4.4 | 3.9 | 3.9 | ||||
| SD | 3.5 | 3.0 | 3.1 | ||||
| Total hours/week† | .2408 | ||||||
| Mean | 63.7 | 61.7 | 57.8 | ||||
| SD | 15.6 | 18.1 | 14.1 | ||||
| Outpatient practice | |||||||
| Outpatients in clinic per week | < .001 | ||||||
| Mean | 77.5 | 68.0 | 59.5 | ||||
| SD | 33.3 | 24.0 | 20.7 | ||||
| Minutes allocated/new outpatient visit | .2961 | ||||||
| Mean | 51.2 | 52.0 | 53.5 | ||||
| SD | 15.2 | 14.2 | 12.7 | ||||
| Minutes allocated/return outpatient visit | < .001 | ||||||
| Mean | 16.9 | 19.5 | 22.6 | ||||
| SD | 5.5 | 6.6 | 6.9 | ||||
| Hospital practice | |||||||
| Hospital rounding | < .001 | ||||||
| Missing | 13 | 5 | 0 | ||||
| Round own patients when hospitalized | 93 | 28.9 | 25 | 21.0 | 0 | 0.0 | |
| Share rounding with partners in blocks | 53 | 16.5 | 26 | 21.8 | 13 | 56.5 | |
| Share rounding with partners on weekends | 156 | 48.4 | 55 | 46.2 | 7 | 30.4 | |
| Attend oncology teaching service | 3 | 0.9 | 4 | 3.4 | 0 | 0.0 | |
| Do not round in hospital | 17 | 5.3 | 9 | 7.6 | 3 | 13.0 | |
| Inpatients on average hospital day | 5.2 | 5.5 | 4.9 | 4.8 | 6.3 | 5.5 | .4964 |
| No. of weekends rounding in hospital/year | 13.6 | 12.0 | 12.0 | 7.7 | 8.6 | 5.3 | .0338 |
| Compensation method | < .001 | ||||||
| Missing | 21 | 4 | 1 | ||||
| Salary no incentive | 56 | 17.8 | 24 | 20.0 | 15 | 68.2 | |
| Salary with bonus | 128 | 40.8 | 48 | 40.0 | 6 | 27.3 | |
| Pure incentive | 130 | 41.4 | 48 | 40.0 | 1 | 4.5 | |
Abbreviations: HMO, health maintenance organization; PP, private practice; SD, standard deviation.
Including single-specialty group, multispecialty group, and HMO.
Sum of above four categories.
Table A4.
Personal Characteristics and Burnout
| Characteristic | Burned Out (n = 484) |
No Burnout (n = 599) |
P | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Age, years | |||||
| Median | 50 | 54 | < .001 | ||
| Missing | 10 | 16 | < .001 | ||
| < 40 | 36 | 57.1 | 27 | 42.9 | |
| 40-49 | 194 | 52.9 | 173 | 47.1 | |
| 50-59 | 172 | 51.0 | 165 | 49.0 | |
| ≥ 60 | 72 | 24.8 | 218 | 75.2 | |
| Sex | < .001 | ||||
| Missing | 2 | 10 | |||
| Male | 212 | 39.8 | 321 | 60.2 | |
| Female | 270 | 50.2 | 268 | 49.8 | |
| Children | .0057 | ||||
| Missing | 2 | 8 | |||
| Yes | 398 | 43.2 | 523 | 56.8 | |
| No | 84 | 55.3 | 68 | 44.7 | |
| Age of youngest child, years | < .001 | ||||
| Missing | 87 | 78 | |||
| < 5 | 61 | 51.7 | 57 | 48.3 | |
| 5-12 | 125 | 51.0 | 120 | 49.0 | |
| 13-18 | 80 | 51.0 | 77 | 49.0 | |
| 19-22 | 46 | 43.8 | 59 | 56.2 | |
| > 22 | 85 | 29.0 | 208 | 71.0 | |
| Relationship status | .0456 | ||||
| Missing | 1 | 9 | |||
| Single | 52 | 53.6 | 45 | 46.4 | |
| Married | 410 | 44.4 | 514 | 55.6 | |
| Partnered | 17 | 51.5 | 16 | 48.5 | |
| Widowed/widower | 4 | 21.1 | 15 | 78.9 | |
| Ever gone through divorce | .3932 | ||||
| Missing | 4 | 10 | |||
| Yes | 78 | 41.7 | 109 | 58.3 | |
| No | 397 | 45.4 | 477 | 54.6 | |
| Currently going through one | 5 | 62.5 | 3 | 37.5 | |
| Current student loan debt | .0023 | ||||
| Missing | 4 | 9 | |||
| No debt | 410 | 42.8 | 547 | 57.2 | |
| Debt < $25,000 | 15 | 57.7 | 11 | 42.3 | |
| $25,000-$49,999 | 6 | 46.2 | 7 | 53.8 | |
| $50,000-$74,999 | 21 | 75.0 | 7 | 25.0 | |
| $75,000-$99,999 | 12 | 75.0 | 4 | 25.0 | |
| $100,000-$125,000 | 5 | 50.0 | 5 | 50.0 | |
| > $125,000 | 11 | 55.0 | 9 | 45.0 | |
Table A5.
Practice Characteristics and Burnout
| Characteristic | Burned Out (n = 484) |
No Burnout (n = 599) |
P | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| General | |||||
| Time devoted to patient care, % | < .001 | ||||
| Missing | 1 | 5 | |||
| None | 10 | 15.9 | 53 | 84.1 | |
| 1-25 | 24 | 25.8 | 69 | 74.2 | |
| 26-50 | 38 | 31.4 | 83 | 68.6 | |
| 51-75 | 99 | 50.3 | 98 | 49.7 | |
| 76-100 | 312 | 51.7 | 291 | 48.3 | |
| Focus on specific type cancer | . 3804 | ||||
| Missing | 15 | 19 | |||
| Yes | 192 | 46.4 | 222 | 53.6 | |
| No | 277 | 43.6 | 358 | 56.4 | |
| Time supervising physicians in training, % | .2539 | ||||
| Missing | 22 | 46 | |||
| 0 | 154 | 41.5 | 217 | 58.5 | |
| < 5 | 114 | 50.2 | 113 | 49.8 | |
| 5-10 | 88 | 48.6 | 93 | 51.4 | |
| 11-20 | 60 | 46.2 | 70 | 53.8 | |
| > 20 | 46 | 43.4 | 60 | 56.6 | |
| Hours and call schedule | |||||
| Mean nights spent on call/week | 2.2 | 1.8 | < .001 | ||
| Hours spent seeing patients at work/week | < .001 | ||||
| Mean | 39.3 | 30.6 | |||
| SD | 15.3 | 17.1 | |||
| Hours spent on administrative tasks at work/week | .1508 | ||||
| Mean | 11.4 | 11.7 | |||
| SD | 9.2 | 11.4 | |||
| Hours spent at home on work tasks/week | .0081 | ||||
| Mean | 9.0 | 8.2 | |||
| SD | 8.4 | 8.9 | |||
| Hours spent at home keeping abreast of development/week | < .001 | ||||
| Mean | 4.1 | 4.9 | |||
| SD | 3.6 | 4.1 | |||
| Total hours/week* | < .001 | ||||
| Mean | 63.4 | 54.3 | |||
| SD | 16.7 | 21.5 | |||
| Outpatient practice | |||||
| Outpatients in clinic/week | < .001 | ||||
| Mean | 60.0 | 46.2 | |||
| SD | 32.8 | 33.7 | |||
| Minutes allocated/new outpatient visit | .0021 | ||||
| Mean | 52.3 | 47.7 | |||
| SD | 16.2 | 21.7 | |||
| Minutes allocated/return outpatient visit | .5737 | ||||
| Mean | 18.8 | 18.0 | |||
| SD | 6.6 | 8.9 | |||
| Hospital practice | |||||
| Hospital rounding | < .001 | ||||
| Missing | 17 | 20 | |||
| Round own patients when hospitalized | 77 | 48.1 | 83 | 51.9 | |
| Share rounding with partners in blocks | 92 | 54.1 | 78 | 45.9 | |
| Share rounding with partners on weekends | 155 | 51.0 | 149 | 49.0 | |
| Attend oncology teaching service | 106 | 43.1 | 140 | 56.9 | |
| Do not round in hospital | 37 | 22.3 | 129 | 77.7 | |
| Inpatients on average hospital day | 7.9 | 7.4 | 6.5 | 7.2 | < .001 |
| No. of weekends rounding in hospital/year | 10.9 | 9.0 | 9.2 | 10.3 | < .001 |
| Compensation method | .0105 | ||||
| Missing | 21 | 63 | |||
| Salary no incentive | 135 | 40.7 | 197 | 59.3 | |
| Salary with bonus | 216 | 47.1 | 243 | 52.9 | |
| Pure incentive | 112 | 53.8 | 96 | 46.2 | |
Abbreviation: SD, standard deviation.
Sum of above four categories.
Table A6.
Career Satisfaction, Burnout, and Quality of Life Among Different PP Settings
| Characteristic | Single Specialty (n = 334) |
Multispecialty (n = 122) |
HMO (n = 23) |
P | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Burnout indices* | |||||||
| Emotional exhaustion† | |||||||
| Median | 24 | 26 | 26 | .5692 | |||
| Low score | 114 | 34.5 | 36 | 29.3 | 7 | 30.4 | .7380 |
| Intermediate score | 80 | 24.2 | 28 | 22.8 | 5 | 21.7 | |
| High score | 136 | 41.2 | 59 | 48.0 | 11 | 47.8 | |
| Depersonalization† | |||||||
| Median | 6 | 7 | 5 | .2251 | |||
| Low score | 158 | 47.7 | 49 | 39.8 | 13 | 56.5 | .4034 |
| Intermediate score | 71 | 21.5 | 34 | 27.6 | 5 | 21.7 | |
| High score | 102 | 30.8 | 40 | 32.5 | 5 | 21.7 | |
| Personal accomplishment‡ | |||||||
| Median | 42 | 42 | 41 | .5931 | |||
| Low score | 215 | 65.3 | 76 | 61.8 | 13 | 56.5 | .6827 |
| Intermediate score | 75 | 22.8 | 35 | 28.5 | 7 | 30.4 | |
| High score | 39 | 11.9 | 12 | 9.8 | 3 | 13.0 | |
| Burned out§ | 162 | 48.9 | 68 | 55.3 | 11 | 47.8 | .4692 |
| Career satisfaction | |||||||
| Would become physician again (career choice) | 260 | 78.3 | 101 | 82.1 | 17 | 77.3 | .6561 |
| Would become oncologist again (specialty choice) | 262 | 78.9 | 92 | 76.0 | 14 | 63.6 | .2284 |
Abbreviations: AP, academic practice; HMO, health maintenance organization; MBI, Maslach Burnout Inventory; PP, private practice.
As assessed using the full MBI.
Per the standard scoring of the MBI for health care workers, physicians with scores ≥ 27 on the emotional exhaustion subscale, ≥ 10 on the depersonalization subscale, or < 33 on the personal accomplishment subscale are considered to have a high degree of burnout in that dimension.
Low scores on the personal accomplishment subscale are less favorable.
High score on emotional exhaustion and/or depersonalization subscales of the MBI (see Methods).
Footnotes
Supported by the American Society of Clinical Oncology, National Institutes of Health (American College of Surgeons Oncology Group Community Clinical Oncology Program Grant No. U10 CA149950), and Mayo Clinic Department of Medicine Program on Physician Well-Being.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Tait D. Shanafelt, William J. Gradishar, Michael Kosty, Helen Chew, Leora Horn, Quyen Chu, John Pippen, Jeff Sloan, Marilyn Raymond
Financial support: Tait D. Shanafelt, Jeff Sloan, Marilyn Raymond
Administrative support: Tait D. Shanafelt, Ben Clark, Amy E. Hanley, Jeff Sloan, Marilyn Raymond
Collection and assembly of data: Tait D. Shanafelt, William J. Gradishar, Michael Kosty, Daniel Satele, Helen Chew, Leora Horn, Ben Clark, Amy E. Hanley, Quyen Chu, Jeff Sloan, Marilyn Raymond
Data analysis and interpretation: Tait D. Shanafelt, William J. Gradishar, Michael Kosty, Daniel Satele, Helen Chew, Leora Horn, Quyen Chu, John Pippen, Jeff Sloan, Marilyn Raymond
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Shanafelt T, Dyrbye L. Oncologist burnout: Causes, consequences, and responses. J Clin Oncol. 2012;30:1235–1241. doi: 10.1200/JCO.2011.39.7380. [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt T, Adjei A, Meyskens FL. When your favorite patient relapses: Physician grief and well-being in the practice of oncology. J Clin Oncol. 2003;21:2616–2619. doi: 10.1200/JCO.2003.06.075. [DOI] [PubMed] [Google Scholar]
- 3.Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–1269. doi: 10.1038/bjc.1995.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory Manual (ed 3) Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 5.Shanafelt T, Sloan J, Habermann T. The well-being of physicians. Am J Med I. 2003;114:513–517. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: Suicidal ideation among American surgeons. Arch Surg. 2011;146:54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 7.Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168–174. doi: 10.1001/archsurg.2011.1481. [DOI] [PubMed] [Google Scholar]
- 8.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: A consensus statement. JAMA. 2003;289:3161–3166. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 9.Firth-Cozens J, Greenhalgh J. Doctors' perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–1022. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- 10.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 11.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 12.West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, Massie FS, Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–1180. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt T, Sloan J, Satele D, et al. Why do surgeons consider leaving practice? J Am Coll Surg. 2011;212:421–422. doi: 10.1016/j.jamcollsurg.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Whippen DA, Canellos GP. Burnout syndrome in the practice of oncology: Results of a random survey of 1,000 oncologists. J Clin Oncol. 1991;9:1916–1920. doi: 10.1200/JCO.1991.9.10.1916. [DOI] [PubMed] [Google Scholar]
- 16.Allegra C, Hall R, Yothers G. Prevalence of burnout in the U.S. oncology community: Results of a 2003 survey. J Oncol Pract. 2005;1:140–147. doi: 10.1200/jop.2005.1.4.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shanafelt T, Novotny P, Johnson ME, et al. The well-being and personal wellness promotion practices of medical oncologists in the North Central Cancer Treatment Group. Oncology (Karger) 2005;68:23–32. doi: 10.1159/000084519. [DOI] [PubMed] [Google Scholar]
- 18.Shanafelt T, Chung H, White H, et al. Shaping your career to maximize personal satisfaction in the practice of oncology. J Clin Oncol. 2006;24:4020–4026. doi: 10.1200/JCO.2006.05.8248. [DOI] [PubMed] [Google Scholar]
- 19.Rafferty JP, Lemkau JP, Purdy RR, et al. Validity of the Maslach Burnout Inventory for family practice physicians. J Clin Psychol. 1986;42:488–492. doi: 10.1002/1097-4679(198605)42:3<488::aid-jclp2270420315>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 20.Lee RT, Ashforth BE. A meta-analytic examination of the correlates of the three dimensions of job burnout. J Appl Psychol. 1996;81:123–133. doi: 10.1037/0021-9010.81.2.123. [DOI] [PubMed] [Google Scholar]
- 21.Leiter M, Durup J. The discriminant validity of burnout and depression: A confirmatory factor analytic study. Anxiety Stress Coping. 1994;7:357–373. [Google Scholar]
- 22.Thomas NK. Resident burnout. JAMA. 2004;292:2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 23.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 24.Rosen IM, Gimotty PA, Shea JA, et al. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81:82–85. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 25.Dyrbye LN, West CP, Shanafelt TD. Defining burnout as a dichotomous variable. J Gen Intern Med. 2009;24:440. doi: 10.1007/s11606-008-0876-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuerer HM, Eberlein TJ, Pollock RE, et al. Career satisfaction, practice patterns and burnout among surgical oncologists: Report on the quality of life of members of the Society of Surgical Oncology. Ann Surg Oncol. 2007;14:3043–3053. doi: 10.1245/s10434-007-9579-1. [DOI] [PubMed] [Google Scholar]
- 27.Frank E, McMurray JE, Linzer M, et al. Career satisfaction of US women physicians: Results from the Women Physicians' Health Study—Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426. doi: 10.1001/archinte.159.13.1417. [DOI] [PubMed] [Google Scholar]
- 28.Lemkau J, Rafferty J, Gordon R., Jr Burnout and career-choice regret among family practice physicians in early practice. Fam Pract Res J. 1994;14:213–222. [PubMed] [Google Scholar]
- 29.Goitein L, Shanafelt TD, Wipf JE, et al. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165:2601–2606. doi: 10.1001/archinte.165.22.2601. [DOI] [PubMed] [Google Scholar]
- 30.West CP, Dyrbye LN, Sloan JA, et al. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24:1318–1321. doi: 10.1007/s11606-009-1129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.West CP, Dyrbye LN, Satele DV, et al. Concurrent validity of single item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27:1445–1445. doi: 10.1007/s11606-012-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 33.Sloan JA, Cella D, Hays RD. Clinical significance of patient-reported questionnaire data: Another step toward consensus. J Clin Epidemiol. 2005;58:1217–1219. doi: 10.1016/j.jclinepi.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 34.Sloan JA. Assessing the minimally clinically significant difference: Scientific considerations, challenges and solutions. COPD. 2005;2:57–62. doi: 10.1081/copd-200053374. [DOI] [PubMed] [Google Scholar]
- 35.Leigh JP, Tancredi D, Jerant A, et al. Annual work hours across physician specialties. Arch Intern Med. 2011;171:1211–1213. doi: 10.1001/archinternmed.2011.294. [DOI] [PubMed] [Google Scholar]
- 36.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 37.Balch CM, Shanafelt TD, Sloan JA, et al. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011;254:558–568. doi: 10.1097/SLA.0b013e318230097e. [DOI] [PubMed] [Google Scholar]
- 38.Grunfeld E, Whelan TJ, Zitzelsberger L, et al. Cancer care workers in Ontario: Prevalence of burnout, job stess, and job satisfaction. Cmaj. 2000;163:166–169. [PMC free article] [PubMed] [Google Scholar]
- 39.Grunfeld E, Zitzelsberger L, Coristine M, et al. Job stress and job satisfaction of cancer care workers. Psychooncology. 2005;14:61–69. doi: 10.1002/pon.820. [DOI] [PubMed] [Google Scholar]
- 40.Arigoni F, Bovier PA, Mermillod B, et al. Prevalence of burnout among Swiss cancer clinicians, paediatricians and general practitioners: Who are most at risk? Support Care Cancer. 2009;17:75–81. doi: 10.1007/s00520-008-0465-6. [DOI] [PubMed] [Google Scholar]
- 41.Asai M, Morita T, Akechi T, et al. Burnout and psychiatric morbidity among physicians engaged in end-of-life care for cancer patients: A cross-sectional nationwide survey in Japan. Psychooncology. 2007;16:421–428. doi: 10.1002/pon.1066. [DOI] [PubMed] [Google Scholar]
- 42.Asch D, Jedrziewski M, Christakis N. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 43.Kellerman S, Herold J. Physician response to surveys: A review of the literature. Am J Prev Med. 2001;20:61–71. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 44.Warde CM, Moonesinghe K, Allen W, et al. Marital and parental satisfaction of married physicians with children. J Gen Intern Med. 1999;14:157–165. doi: 10.1046/j.1525-1497.1999.00307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: A missing quality indicator. Lancet. 2009;374:1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 46.Grol R, Mokkink H, Smits A, et al. Work satisfaction of general practitioners and the quality of patient care. Fam Pract. 1985;2:128–135. doi: 10.1093/fampra/2.3.128. [DOI] [PubMed] [Google Scholar]
- 47.Linn LS, Brook RH, Clark VA, et al. Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Med Care. 1985;23:1171–1178. doi: 10.1097/00005650-198510000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122–128. doi: 10.1046/j.1525-1497.2000.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Melville A. Job satisfaction in general practice: Implications for prescribing. Soc Sci Med [Med Psychol Med Sociol] 1980;14A:495–499. doi: 10.1016/0160-7979(80)90050-8. [DOI] [PubMed] [Google Scholar]
- 50.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians' characteristics influence patients' adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 51.Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: The personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255:625–633. doi: 10.1097/SLA.0b013e31824b2fa0. [DOI] [PubMed] [Google Scholar]
- 52.Krasner MS, Epstein RM, Quill TE, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 53.Shanafelt TD, West CP, Sloan JA, et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169:990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 54.Dunn PM, Arnetz BB, Christensen JF, Homer L. Meeting the imperative to improve physician well-being: Assessment of an innovative program. J Gen Intern Med. 2007;22:1544–1552. doi: 10.1007/s11606-007-0363-5. [DOI] [PMC free article] [PubMed] [Google Scholar]